The application of intraoperative radiation therapy to the tumor bed after resection of pancreatic cancer has been shown to be beneficial in the local control of the disease. The objective of this study was to evaluate the preliminary outcomes after the application of a single intraoperative dose to the tumor bed with a new intraoperative radiotherapy device (Intrabeam®) in terms of viability, safety and short-term results.
MethodsWe studied 5 patients who underwent pancreaticoduodenectomy for resectable pancreatic cancer in which a radiotherapy boost (5Gy) was intraoperatively applied to the tumoral bed using the portable Intrabeam® device, a low-energy point-source X-ray. Postoperative complications, hospital stay and mortality, recurrences and short-term survival were analyzed.
ResultsMean patient age was 68 years. All patients had a T3-stage tumor and one of them N1. In 3 patients, R0 resection was performed, while R1 resection was conducted in 2. Perioperative mortality was 0%. The only complications included delayed gastric emptying and postoperative hemorrhage. There were no pancreatic fistulas. During follow-up (mean: 11.2 months), there was a relapse in the patient who had undergone R1 resection.
ConclusionsThe application of radiotherapy with the Intrabeam® device in selected patients has not resulted in increased perioperative morbidity or mortality; therefore, this is a safe procedure for the treatment of resectable cancer.
La aplicación de radioterapia intraoperatoria en el lecho tumoral tras la resección de un cáncer de páncreas ha demostrado ser beneficiosa en el control local de la enfermedad. El objetivo de este estudio fue valorar los resultados iniciales obtenidos tras la aplicación de una nueva modalidad de radioterapia intraoperatoria (Intrabeam®) en términos de viabilidad, seguridad y resultados a corto plazo.
MétodosSe estudiaron 5 pacientes sometidos a duodenopancreatectomía cefálica por cáncer de páncreas resecable, en los que se aplicó intraoperatoriamente un boost de radioterapia (5Gy) en el lecho tumoral mediante la utilización del dispositivo portátil Intrabeam®, fuente puntual de rayos X de baja energía. Se analizaron las complicaciones, estancia y mortalidad postoperatorias, recidivas y superviviencia a corto plazo.
ResultadosLa edad media fue de 68 años. Todos los pacientes presentaban un estadio tumoral T3 y uno de ellos N1. En 3 pacientes se realizó una resección R0 y en 2 casos resultó ser una resección R1. La mortalidad peroperatoria fue del 0%. Solo se presentaron como complicaciones un retraso en el vaciamiento gástrico y una hemorragia postoperatoria. No hubo fístulas pancreáticas. Durante el seguimiento (media: 11,2 meses) se constató una recidiva en el paciente en el que se había practicado una resección R1.
ConclusionesLa aplicación de radioterapia con el dispositivo Intrabeam® en pacientes seleccionados no ha supuesto un aumento de la morbimortalidad peroperatoria, mostrándose como un procedimiento seguro en el tratamiento del cáncer resecable.
The incidence of pancreatic cancer is similar to its mortality rate, causing 331000 deaths per year to become the seventh cause of cancer-related death in both sexes.1 This situation is influenced by the fact that diagnosis is usually made in the late phase and due to the biological characteristics of this type of tumor, leading to these unfavorable results.2 At diagnosis, 52% of patients already have distant disease, and 26% present locoregional extension. For these reasons, only 20% of patients are resectable.3
In addition to neoadjuvant and/or adjuvant chemoradiotherapy,3 intraoperative radiotherapy (IORT) of the tumor bed has been used, which has shown a benefit in the local control of the disease and in patient quality of life.2,4–7 Most of these studies are retrospective, except for the Klinkenbilj article, which presents a non-randomized prospective study.4 In most of the published series, IORT has been administered with linear electron accelerators, requiring the transfer of the patient from the operating room to the radiotherapy room during surgery, although portable devices are already available to apply the treatment in the operating room.8 The development of portable radiotherapy equipment has been extremely important and has led to the generalized is of IORT at many hospitals. The use of low-energy X-ray therapy, such as targeted intraoperative radiotherapy using the Intrabeam® portable device, has proven to be an excellent method for the treatment of cancer of the breast9–11 and other locations, including the digestive tract.12 However, its intraoperative use for the treatment of pancreatic cancer as a complement to surgery has been poorly documented. The aim of this study was to present our initial IORT experience with Intrabeam® for the treatment of resectable pancreatic cancer in terms of viability, safety and short-term results.
MethodsThe study design was observational with prospective data collection. Between June 2016 and May 2017, 8 patients with potentially resectable head of the pancreas cancer13 were referred to the surgery unit for treatment. After being presented in the multidisciplinary committee, 5 were selected for the surgical protocol and IORT. In the 3 remaining cases, this type of therapy could not be applied due to lack of availability of the device. The study was approved by the Clinical Research and Ethics Committee of the hospital (AEMPS Code: R-kilovolt Study, CEIC Code: 150063). All patients signed informed consent forms.
Inclusion Criteria(1) Patients aged 18 or more, of both sexes; (2) good functional state (KPS≥70%), with a life expectancy greater than 6 months; (3) potentially resectable carcinoma of the pancreas without distant metastasis, with pre- or intraoperative histological confirmation (if there was no diagnosis of adenocarcinoma, treatment was not applied); and (4) solitary pancreatic, with a diameter less than 7cm.
Exclusion Criteria(1) Metastatic disease; (2) liver failure (AST and/or ALT>2 times the normal values established by the lab reference range); renal failure (serum creatinine greater than 2mg/dL) and/or hemorrhagic diathesis; (3) inadequate bone marrow function (neutrophils<2000/L, platelets<100000/L); (4) pregnancy; (5) previous malignant tumors; (6) malignant intraductal papillary tumors; (7) patients in whom the positivity of the sample could not be determined pre- or intraoperatively; and (8) inability to comply with the study and/or follow-up treatment.
ProcedureAll patients were evaluated with computerized tomography (CT) for staging, magnetic resonance imaging (MRI) and/or endoscopic ultrasound. In all patients, the existence of the neoplasm could be confirmed histologically during surgery. Some patients underwent preoperative drainage of the bile duct due to bilirubin levels above 15ng/dL. Candidate patients were referred to the Radiotherapy and Oncology Service for assessment and signing informed consent forms.
On the day of the intervention, the protocol was as follows:
- 1.
In the surgical anteroom, the medical physics team performed the necessary calibrations to ensure a stable accelerator radiation beam.
- 2.
Using exploratory laparotomy and, after confirmation of tumor resectability. pancreaticoduodenectomy was conducted with or without pylorus preservation.
- 3.
Intraoperative confirmation of malignancy and pathology verification of the margins of the surgical piece.
- 4.
The surgical support stand for the X-ray source was prepared with a sterile cover and the sterile applicator was adjusted to the source at the end of the stand. The applicator diameter was chosen according to the surgical bed to be irradiated.
- 5.
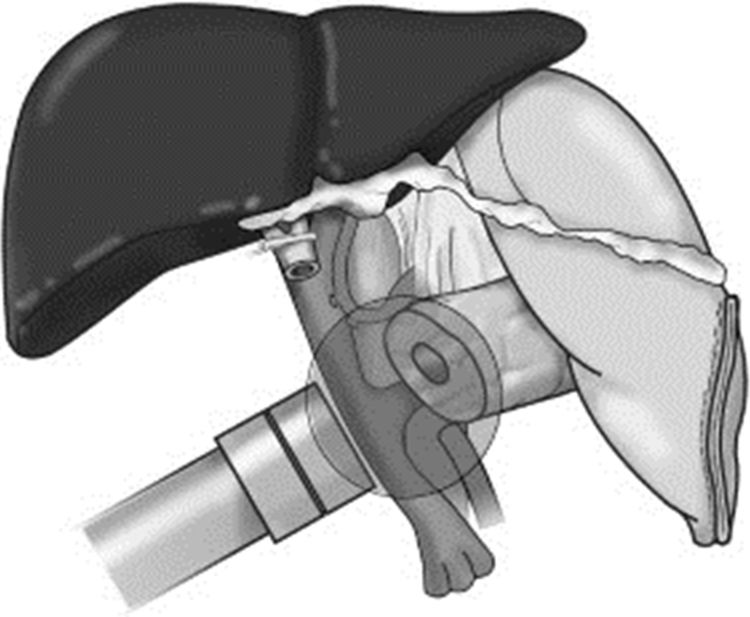
Mobilization of the holder and placement of the flat applicator 1cm from the surgical bed, using the articulated arm (Fig. 1).
- 6.
Placement of moist compresses in the rest of the surgical field.
- 7.
Tungsten sheets for radiation shielding were placed on the perimeter of the device, although using the flat applicator the dispersion of radiation is known to be minimal. These sheets block 95% of the radiation. In spite of this, personal radiation protection measures are applied at our hospital, including:
- a.
No access to the OR during therapy
- b.
Evacuation of personnel from the OR
- c.
Control of the accelerator console and anesthesia from the adjacent anteroom
- d.
Verification that radiation risk sign is on and that access doors to the OR are locked
- 8.
Start of radiotherapy, administered using the Intrabeam® device (Carl Zeiss Meditec, Oberkochen, Germany), which provides a precise source of low energy X-rays (maximum 50kV) at the tip of a tube that can vary in diameter and is located at the center of a flat applicator (2.5–6cm in diameter). The objective was to apply a dose of radiotherapy as a boost to the surgical site after resection, in the region closest to the excised tumor, which is considered to have the highest risk of recurrence, with the aim to decrease the likelihood of local recurrence. The application time varied depending on the diameter of the applicator, the surface area and the patient. Times ranged between 27 and 42min, calculated according to the diameter of the applicator and the activity of the source. The prescribed dose on the surface of the applicator was 20Gy, which would be a dose of 5Gy 1cm away (Fig. 2).
- 9.
Removal of the device, revision of hemostasis and Child reconstruction
All patients then underwent chemotherapy with gemcitabine and adjuvant external radiotherapy with imaging-guided intensity-modulated radiotherapy (45Gy, 1.8Gy/day) according to the protocol used at the hospital. Adjuvant treatment was administered in the cases indicated according to the guidelines of the National Comprehensive Cancer Network. For neoadjuvant therapy at our hospital, we use regimens based on the combination of gemcitabine–paclitaxel or FOLFIRINOX. All patients were followed up in the outpatient consultation and underwent quarterly testing with thoracoabdominal CT and lab work, including tumor markers.
Statistical StudyThe following data were collected prospectively: age, sex, preoperative drainage, post-operative complications staged according to the definitions of the International Study Group of Pancreatic Surgery14–16 and the Clavien-Dindo classification,17 operative mortality, hospital stay, readmissions, histology, resection type (R0, R1) following the criteria established by the International Union Against Cancer,18,19 IORT characteristics, complementary treatments and early recurrence. The qualitative variables were expressed as number and percentage, and the numerical variables were expressed as mean±standard deviation. Given the small number of patients in the sample studied, no statistical study was performed.
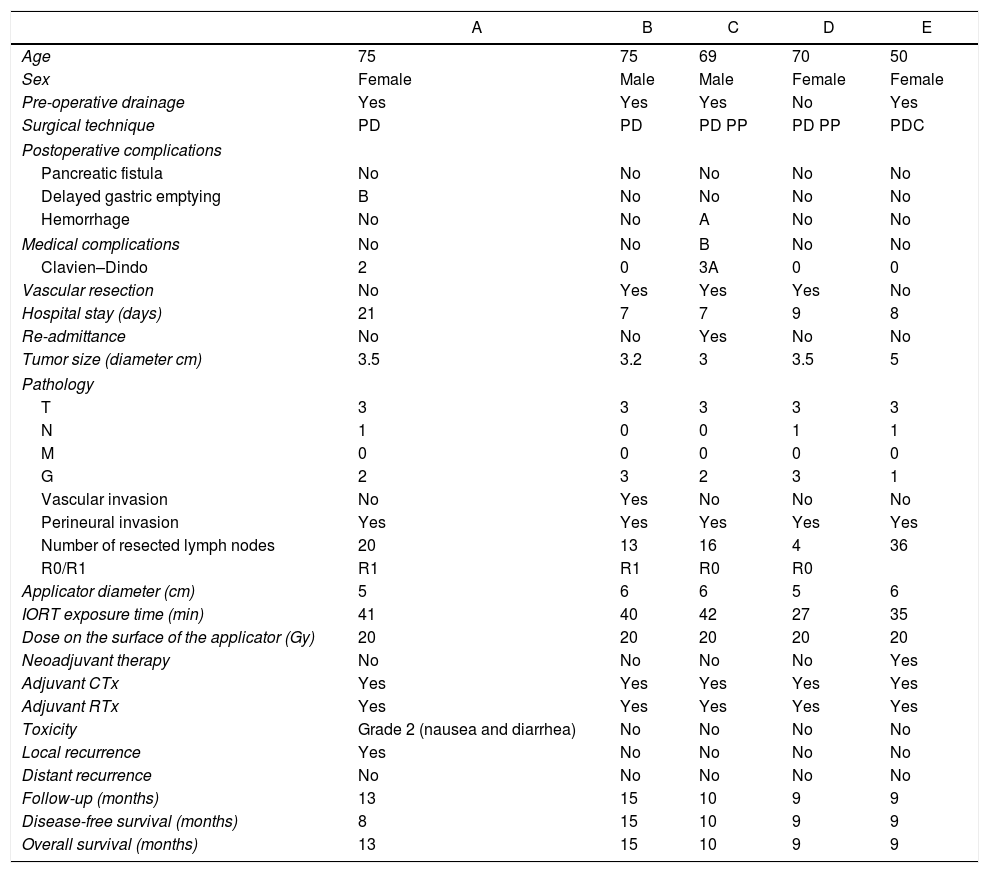
ResultsCharacteristics and results are shown in Table 1. Mean age was 67.8 years (±10.3), 2 men and 3 women. Preoperative drainage was necessary in 4 patients (80%). Partial portal vascular resection was done in 3 cases (60%) due to suspected vascular invasion, not requiring the use of vascular grafts or stents, which was only able to be confirmed in the histology study in one case. Mean hospital stay was 10.4 days (±6.0). Complications occurred in 2 patients (40%): one delayed gastric emptying, and one grade B extraluminal postoperative hemorrhage,16 which was treated by transfusion. There were no pancreatic fistulae. In 3 patients, there were no complications. Perioperative mortality was 0%. There were no complications secondary to the use of IORT. In 2 cases, after the definitive histology study, R1 resection was confirmed (microscopic involvement of the margin). According to the TNM classification, all tumors were ductal adenocarcinomas and staged as T3, 3 of which were N1. Perineural invasion was observed in all cases. One of them was well differentiated (G1), 2 were moderately differentiated (G2) and the other 2 poorly differentiated (G3). Adjuvant therapy with gemcitabine and RT was administered to all patients. In one patient, grade 2 gastrointestinal toxicity was observed, with nausea and diarrhea. Mean follow-up was 11.2 months (±2.7). During this short follow-up period, one patient whose definitive histology was R1 relapsed.
Patient Characteristics and Results of the Patients Treated With Radical Surgery and IORT With Intrabeam for Resectable Cancer in the Head of the Pancreas.
| A | B | C | D | E | |
|---|---|---|---|---|---|
| Age | 75 | 75 | 69 | 70 | 50 |
| Sex | Female | Male | Male | Female | Female |
| Pre-operative drainage | Yes | Yes | Yes | No | Yes |
| Surgical technique | PD | PD | PD PP | PD PP | PDC |
| Postoperative complications | |||||
| Pancreatic fistula | No | No | No | No | No |
| Delayed gastric emptying | B | No | No | No | No |
| Hemorrhage | No | No | A | No | No |
| Medical complications | No | No | B | No | No |
| Clavien–Dindo | 2 | 0 | 3A | 0 | 0 |
| Vascular resection | No | Yes | Yes | Yes | No |
| Hospital stay (days) | 21 | 7 | 7 | 9 | 8 |
| Re-admittance | No | No | Yes | No | No |
| Tumor size (diameter cm) | 3.5 | 3.2 | 3 | 3.5 | 5 |
| Pathology | |||||
| T | 3 | 3 | 3 | 3 | 3 |
| N | 1 | 0 | 0 | 1 | 1 |
| M | 0 | 0 | 0 | 0 | 0 |
| G | 2 | 3 | 2 | 3 | 1 |
| Vascular invasion | No | Yes | No | No | No |
| Perineural invasion | Yes | Yes | Yes | Yes | Yes |
| Number of resected lymph nodes | 20 | 13 | 16 | 4 | 36 |
| R0/R1 | R1 | R1 | R0 | R0 | |
| Applicator diameter (cm) | 5 | 6 | 6 | 5 | 6 |
| IORT exposure time (min) | 41 | 40 | 42 | 27 | 35 |
| Dose on the surface of the applicator (Gy) | 20 | 20 | 20 | 20 | 20 |
| Neoadjuvant therapy | No | No | No | No | Yes |
| Adjuvant CTx | Yes | Yes | Yes | Yes | Yes |
| Adjuvant RTx | Yes | Yes | Yes | Yes | Yes |
| Toxicity | Grade 2 (nausea and diarrhea) | No | No | No | No |
| Local recurrence | Yes | No | No | No | No |
| Distant recurrence | No | No | No | No | No |
| Follow-up (months) | 13 | 15 | 10 | 9 | 9 |
| Disease-free survival (months) | 8 | 15 | 10 | 9 | 9 |
| Overall survival (months) | 13 | 15 | 10 | 9 | 9 |
PD: pancreaticoduodenectomy; PD PP: pancreaticoduodenectomy with pylorus preservation.
Surgery is considered the only therapeutic option for pancreatic carcinoma capable of providing a cure. However, locoregional and/or metastatic recurrence appears from 9 to 15 months after diagnosis, and life expectancy is between 12 and 15 months without adjuvant therapy.2 The presence of distant and locoregional subclinical disease is responsible for the limited survival of these resectable patients. Although theoretically a R0 resection would imply greater survival than in cases of residual disease after resection, long-term control of the disease has not yet been achieved.20 To date, the standardized use of locoregional treatments, such as external radiotherapy, or systemic treatments, such as chemotherapy, have only led to a modest improvement in clinical outcomes.20,21
These modest results are due to 2 fundamental reasons. First is the limited efficacy of systemic treatments available to date, which make it difficult to control subclinical distant disease, despite the use of new combinations (FOLFIRINOX and nab-paclitaxel) in addition to gemcitabine.22,23 The second reason is the technical difficulty that exists for administering high doses of adjuvant radiotherapy when external radiotherapy is used. Although the new intensity-modulated radiotherapy techniques with imaging guidance24 have improved the distribution and precision of the radiotherapy dose administered, the existence of healthy organs with a low tolerance to radiation in the area adjacent to the surgical bed does not allow us to administer the entire dose of radiotherapy that would be necessary to improve the results obtained to date.
Perhaps the only way we currently have to administer a high dose of radiation to the tumor bed, with extreme precision in its location, no loss of time and in the same operation, would be IORT. It has the advantage of being able to modify the microenvironment of the surgical site, limiting the growth of residual tumor cells.25 Defined as the application of a single fraction of a high dose of radiation during surgery on the tumor bed, it is able to reduce the radiation dose to the surrounding normal tissues, which are separated from the radiation field during the procedure.26,27 IORT for pancreatic cancer would therefore be used as a boost before adjuvant external beam radiotherapy (EBRT). Some may consider that, due to the drop in dosage from the time it leaves the applicator until it arrives in the surgical bed, the dose used might be insufficient, but it is a dose equivalent to the one applied to the pancreas with electron therapy. There is no certainty that higher doses are safe in terms of perioperative morbidity and mortality. After demonstrating its safety in larger studies, such an increase could be considered. All the studies published to date26–34 have demonstrated the utility of IORT for local control of the disease, and the Sindelair study34 is the only prospective randomized study that has demonstrated local control. However, there has been a stagnation in this technique, probably induced by the lack of improved survival, although with the new chemotherapy strategies it is possible that the IORT would improve this factor.
The application of IORT with Intrabeam® offers several advantages over other techniques. The radiation dose is applied to the extension of the tumor bed necessary in each case, with a minimum dispersion of the radiation with the flat applicator and maximum precision of the application to the tumor bed. The radiation dose can be modified and the exposure time does not significantly increase surgical time. Since the beginning of the application of this therapy to treat breast cancer at our hospital, the technical problems that arose in its initial implementation have improved,11 and today we consider it a safe and reproducible technique for the treatment of resectable tumors of the pancreas. This study is limited by the small number of patients included and the limited follow-up. In order to better assess the results of this new approach, long-term results are necessary, especially from multicenter studies with a control group.
Nonetheless, in spite of the limitations mentioned, we have demonstrated the safety, validity and reliability of radical surgery treatment combined with IORT using a portable low-energy X-ray device for targeted intraoperative radiotherapy. No complications inherent to the application of the technique were observed.
AuthorshipAida Cristina Rahy-Martín: study design, data collection, article composition, critical review and approval of the final version.
Francisco Cruz-Benavides: study design, critical review and approval of the final version.
Mar Sánchez-Lauro: critical review and approval of the final version.
Álvaro Rodríguez-Méndez: critical review and approval of the final version.
Íñigo San Miguel: study design, critical review and approval of the final version.
Pedro Lara: study design, critical review and approval of the final version.
Joaquín Marchena-Gómez: study design, analysis and interpretation of the results, critical review and approval of the final version.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Rahy-Martín AC, Cruz-Benavides F, Sánchez-Lauro M, Rodríguez-Méndez Á, San Miguel Í, Lara P, et al. Radioterapia intraoperatoria con Intrabeam® para el tratamiento del adenocarcinoma de páncreas resecable. Cir Esp. 2018;96:482–487.
Part of the information contained in this article was presented at the following conferences: 17th Congress of the Sociedad Canaria de Cirugía, Las Palmas de Gran Canaria (Spain), November 24–26, 2016; and the 14th National Meeting of the Minimally Invasive Surgery and Innovative Technology Divisions of the Asociación Española de Cirujanos, Toledo (Spain), May 11–13, 2017.