Gastric pneumatosis is defined as a collection of gas within the stomach wall and can encompass 2 processes with very different etiologies, symptoms and prognoses: gastric emphysema and emphysematous gastritis.1 Frequently, gastric pneumatosis appears in association with intestinal pneumatosis related to ischemia/intestinal infarction, but when located exclusively in the gastric wall it is a rare entity.2 Gastric emphysema is usually asymptomatic and generally derives from a mechanical cause that causes acute gastric dilatation and increased intraluminal pressure. Emphysematous gastritis is a rare form of gastritis secondary to infection of the gastric wall by gas-forming organisms; in this case, early diagnosis and treatment are essential to avoid the high mortality rate. The treatments of the two conditions are opposing. Patients with gastric emphysema do not require surgical treatment and progress well with conservative treatment, typically nil per os and an NG tube to reduce gastric distension. However, patients with emphysematous gastritis require more aggressive early treatment with broad-spectrum antibiotics, fluid therapy and urgent surgery in certain cases, which is usually indicated when conservative treatment fails or there is perforation.3 Depending on the degree of involvement, surgical treatment may entail partial gastrectomy or even total gastrectomy, depending on the degree of involvement.
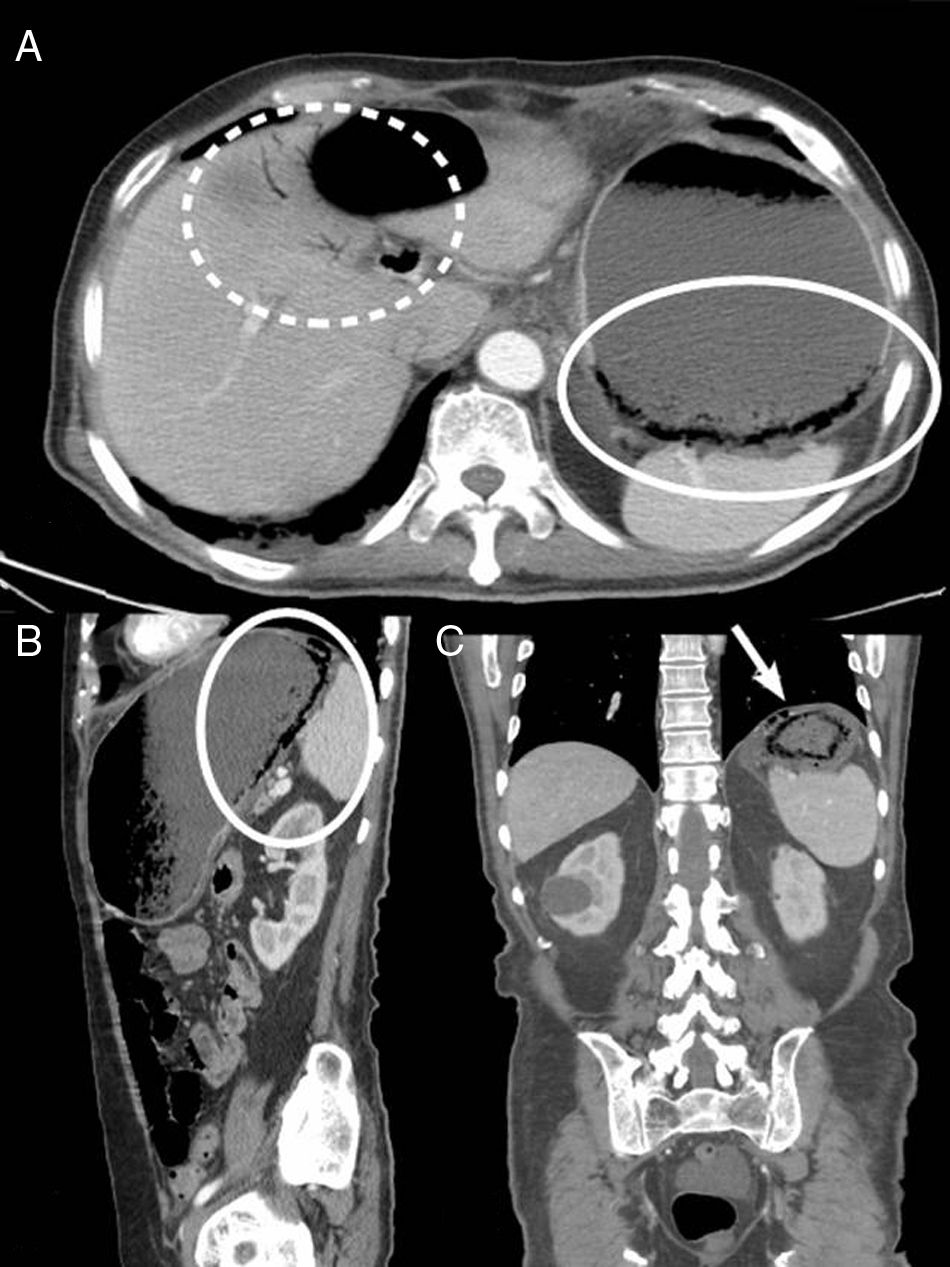
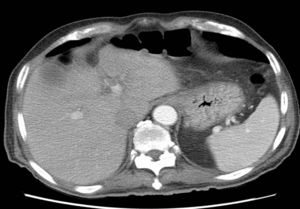
We present the case of a 77-year-old man with a history of DM, HTN, cholelithiasis, and recent hospitalization for severe acute pancreatitis with pancreatic pseudocysts, who was re-admitted due to abdominal pain. Abdominal-pelvic CT scan showed a reduction in pseudocysts, with no peripancreatic inflammatory changes. Incidental findings included important gastric distension with limited wall enhancement in the fundus, multiple gas bubbles and linear images in the gastric wall suggestive of gastric pneumatosis and free fluid, adjacent ectopic gas bubbles (Fig. 1) as well as the presence of portal gas (Fig. 1). Given the CT findings, the patient, who was asymptomatic, was reassessed clinically with abdominal examination and laboratory tests, which were normal. In this case, the differential diagnosis included emphysematous gastritis secondary to a complication of acute pancreatitis or gastric emphysema caused solely by gastric distension. Given that the patient was asymptomatic and hemodynamically stable, we decided to proceed with conservative treatment with NG tube placement and nil per os. The patient progressed favorably, and a follow-up CT scan 7 days later demonstrated complete disappearance of the gastric pneumatosis, portal gas, free fluid and ectopic gas (Fig. 2), and the patient was discharged 3 days later.
Abdominal-pelvic CT with intravenous contrast in axial (A), sagittal (B) and coronal (C) planes, showing important gastric distension with limited wall enhancement in the fundus, where multiple intramural gas bubbles are observed, suggestive of gastric pneumatosis (circle), free fluid and bubbles of ectopic gas (arrow), as well as venous gas in left main portal branch and distal portal branches of the left hepatic lobe (dashed circle).
In the case of gastric emphysema of generally mechanical etiology, cases have been described after gastroscopy, vigorous vomiting and aerophagia in situations of obstructed distal gastric emptying4 (duodenal ulcer, gastric volvulus, cancer of the antrum, small bowel obstruction), even in patients with spinal trauma, associated with pneumothorax or rupture of pleural bullae, associated with acute pancreatitis, prolonged and repeated inhalations and a history of general anesthesia.1
The main differential diagnosis of gastric emphysema includes emphysematous gastritis, which is the infectious form of gastric pneumatosis and has a worse prognosis if not treated appropriately. In the case of emphysematous gastritis, there is usually a lesion in the gastric mucosa that enables passage of gas-producing germs. Predisposing factors include: ingestion of caustic substances, alcohol abuse, abdominal surgery, gastroenteritis and, less commonly, the ingestion of soft drinks, diabetes, gastric mucormycosis,5 ischemia or gastric infarction6 and parasites. Several germs are associated: Clostridium welchii, Clostridium perfringens, Escherichia coli, etc. In this case, contrary to what happens with gastric emphysema, symptoms appear suddenly and vary from epigastric pain, nausea, vomiting, fever, tachycardia, etc., to a state of shock, with high mortality.
The radiological findings of both entities are similar and well defined: presence of bubbles or linear images of air that dissect the gastric wall. Thus, clinical parameters differentiate between these processes and guide the management approach.1 Other associated radiological findings may be observed, such as the presence of portal venous gas,7 which is more frequent in cases of emphysematous gastritis and with a very poor prognosis8; however, it can also be associated with gastric emphysema, with survival rates close to 100%.8 Radiologically, a gastric emphysema can also be distinguished from an emphysematous gastritis by the presence of gastric wall thickening, which is more frequently present in emphysematous gastritis, as well as the finding of other signs that can lead to determining the origin of this gas in the wall gastric (for example, intestinal ischemia).8
In short, gastric pneumatosis is a rare radiological finding. When detected, it is essential to establish whether it is due to gastric emphysema or emphysematous gastritis, since the treatment and prognosis are different and the distinction provides for adequate patient management, while avoiding unnecessary surgical interventions. The fundamental tools for making this distinction are imaging tests (mainly CT8) and the assessment of the patient's clinical status.
Please cite this article as: Belda González I, Soliva Martínez D, Castro García A, Cantero Ayllon MJ, de Miguel Ibañez R. Neumatosis gástrica: cuándo no operar. Cir Esp. 2018;96:121–123.