Organ shortage has forced transplant teams to progressively expand the acceptance of marginal donors.
MethodsWe performed a comparative analysis of the post-transplant evolution depending on donor age (group I: less than 70 years old (n=474) vs group II: 70 or more years old [n=105]) over a 10 year period (2002–2011).
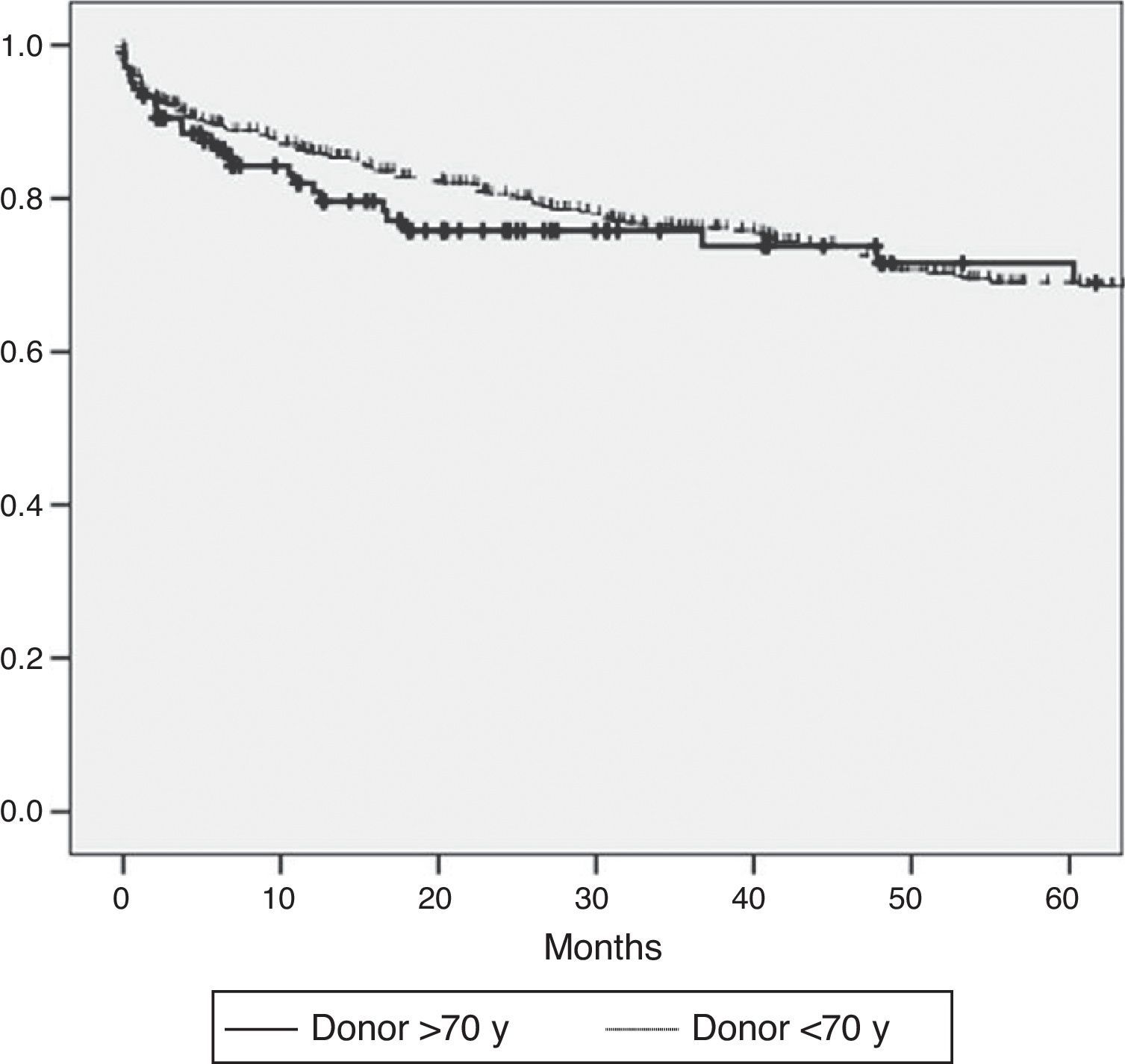
ResultsDonors over 70 years old were similar to donors less than 70 years old in terms of ICU stay, gender, weight, laboratory results, and use of vasoactive drugs. However, the younger donor group presented with cardiac arrest more often (GI: 14 vs GII: 3%, P=.005). There were no differences in initial poor function (GI: 6% vs GII: 7.7%; P=.71), ICU stay (GI: 2.7±2 vs GII: 3.3±3.8, P=.46), hospital stay (GI: 13.5±10 vs GII: 15.5±11, P=.1), or hospital mortality (GI: 5.3 vs GII: 5.8%, P=.66) between receptors of more or less than 70 year old grafts. After a median follow up of 32 months, no differences were found in the incidence of biliary tract complications (GI: 17 vs GII: 20%, P=.4) or vascular complications (GI: 11 vs GII: 9%, P=.69). The actuarial 5 year survival was similar for both study groups (GI: 70 vs GII: 76%, P=.54).
ConclusionsIn our experience, the use of grafts from donors older than 70 years, when other risk factors are avoided (cold ischaemia, steatosis, sodium levels), does not worsen the results of liver transplantation on the short or long term.
La escasez de órganos para trasplante ha hecho aumentar progresivamente la aceptación de donantes con criterios marginales, como la edad.
MétodosSe ha realizado un análisis comparativo de la evolución postrasplante dependiendo de la edad de los donantes (grupo I: edad inferior a 70 años [n=474] vs. grupo II: edad superior a 70 años [n=105]), a lo largo de un periodo de 10 años.
ResultadosNo había diferencias significativas entre ambos grupos en días de UCI, sexo, peso y requerimientos de fármacos vasoactivos. El grupo I presentó parada cardiaca de forma más frecuente (GI: 14 vs. GII: 3%; p=0,005). No hubo diferencias en la disfunción primaria (GI: 6 vs. GII: 7,7%; p=0,71), estancia en UCI (GI: 2,7±2 vs. GII: 3,3±3,8 días; p=0,46) y hospitalaria (GI: 13,5±10 vs. GII: 15,5±11; p=0,1), ni mortalidad hospitalaria (GI: 5,3 vs. GII: 5,8%; p=0,66). Tras una mediana de seguimiento de 42 meses, tampoco se encontraron diferencias en la incidencia de complicaciones biliares (GI: 17 vs. GII: 20%; p=0,40) ni vasculares (GI: 11 vs. GII: 9%; p=0,69). La supervivencia actuarial a 5 años fue similar entre ambos grupos de estudio (GI: 70 vs. GII: 76%; p = 0,54).
ConclusionesEn nuestra experiencia, la utilización de injertos de donantes mayores de 70 años, si se evitan factores de riesgo adicionales (tiempo de isquemia, esteatosis, hipernatremia), no empeora los resultados del trasplante hepático a corto ni a largo plazo.
Donors over 70 years of age are usually considered marginal donors. Both the Donor Risk Index developed by Feng et al.1 with data from the Organ Procurement and Transplantation Network (OPTN) and the risk factors used in the Eurotransplant region for liver donation include age as risk factor for donation. Recent studies show that age, high BMI and diabetes are independent risk factors for primary graft failure (PGF).2 Older donors may not only result in a greater incidence of dysfunction and PGF,3 they may also affect the incidence of arterial complications,4–6 the recurrence of HCV,7–10 and the overall survival rate following the liver transplant11 (LT).
In spite of this, the growing disparity between supply and demand for transplant organs imposes the use of donors with extended criteria, particularly older donors. The gradual ageing of the population together with a decrease in organ donors as a consequence of trauma has increased the ratio of older donors, most of them due to cerebral vascular accidents. Thus, the use of elderly donors has become a necessity for maintaining the ability to carry out transplants, and to avoid an increase in waiting list mortality.
In a study published in 2001 by our group,11 we analysed our experience using older donors; in this study, it was concluded that patients transplanted with grafts from patients of over 70 years old had a greater incidence of graft loss and a decrease in long-term survival rate. Ten years later, we have reassessed our experience with elderly donors. Therefore, the purpose of this study is to analyse the effect of donors of over 70 years old on post LT progress.
MethodsWe have analysed the data from all the LTs performed at our centre between 2002 and 2011 (n=579). The inclusion of patients for this study was closed in 2011 to allow for a minimum follow-up time of two years. All the recipients were adults and all the patients received a graft from a dead donor. The mean follow-up of transplanted patients was 42 months (range 6–78 months).
The only absolute contraindications for organ donors were positive human immunodeficiency virus (HIV), hepatitis B surface antigen (HbsAg), cancers (with the exception of some brain and skin neoplasms) and uncontrolled infections. All other donors were included. Biopsies were made only when deemed necessary by the surgeon following a macroscopic assessment of the liver graft.
The most common extraction technique was a quick extraction, except for patients who were also pancreas donors. The classic hilar dissection technique was used in all cases.
Grafts were implanted into the first patient on the waiting list, except for emergencies. Between 2002 and 2007, the waiting list was based on the time that had elapsed after their inclusion on the transplant list; after 2007 the waiting list was based on the Model for End-stage Liver Disease (MELD) criteria. Weight disproportion was considered during both periods.
Data for donors and recipients was obtained from the prospective database from the Liver Transplant Unit; this data was made anonymous prior to the analysis.
The following donor characteristics were analysed: age, sex, bilirubin, serum natraemia, prothrombin time, alanine aminotransferase (ALT), shipped grafts (removal by a team from another hospital and later shipment of the organ), days at ICU, need for vasoactive drugs, hypotension episodes (TAS<60mmHg for more than one hour), cause of death, cardiopulmonary arrest, diabetes mellitus, cardiopathy, hepatic steatosis and the presence of AcHBc.
The following variables were analysed regarding the progress made by the recipients: age, sex, weight, MELD, HCV, CMV, duration of the intervention, cold ischaemia times, transfusion of packed red blood cells, days at ICU, days of admission, primary graft dysfunction (PGD), PGF, hospital mortality, surgical reintervention, retransplant, rejection episodes, biliary complications, ischaemic cholangitis, arterial complications, graft survival, and actuarial survival after five years.
PGD was defined as levels of ALT>25μkat/l, or of aspartate aminotransferase (AST)>25μkat/l, associated to prothrombin time (PT)>24s, during the first week after the transplant. PGF was defined as the death of the patient due to liver failure, or the need for a re-transplant within the first week, in the absence of technical complications.
The diagnosis and management of each patient were discussed by a multidisciplinary transplant committee. Based on clinical and radiological findings, biliary complications were classified as follows: biliary fistula, anastomotic stenosis (AS: defined as a focal stenosis in biliary anastomosis), non-anastomotic stenosis (NAS: long bile stenosis or intrahepatic stenosis with/without signs of necrosis and biloma) associated or not with arterial thrombosis, choledocholithiasis, and other biliary complications (biliary mould, sphincter of Oddi dysfunction, etc.).
Only arterial complications were considered for this study, within vascular complications (early and late arterial thrombosis, and stenosis of the arterial anastomosis).
Statistical AnalysisPatients were divided into two groups: those who received a graft from a donor aged over 70 years, and those who received a graft from a donor younger than 70 years.
For the two groups, the different variables categorised were compared using a Chi Square test, and continuous variables using a Student t-test. Differences were considered significant if P<.05. Graft survival was calculated from the date of the LT until the date of the last visit, date of death or until the date of graft loss. Patient survival was from the transplant until the last visit or patient's death. Actuarial survival was calculated using the Kaplan–Meyer method, and group differences by the long-rank test. The statistical analysis was conducted with SPSS software (SPSS version 3.0, Inc, Chicago, IL, U.S.).
ResultsA total of 579 LTs were included in our sample, of which 18% (n=105) were with donors aged over 70 years. At the start of the study in 2002, the percentage of donors aged over 70 years was 15%; whereas by the end of the study in 2011 this had increased to 25%.
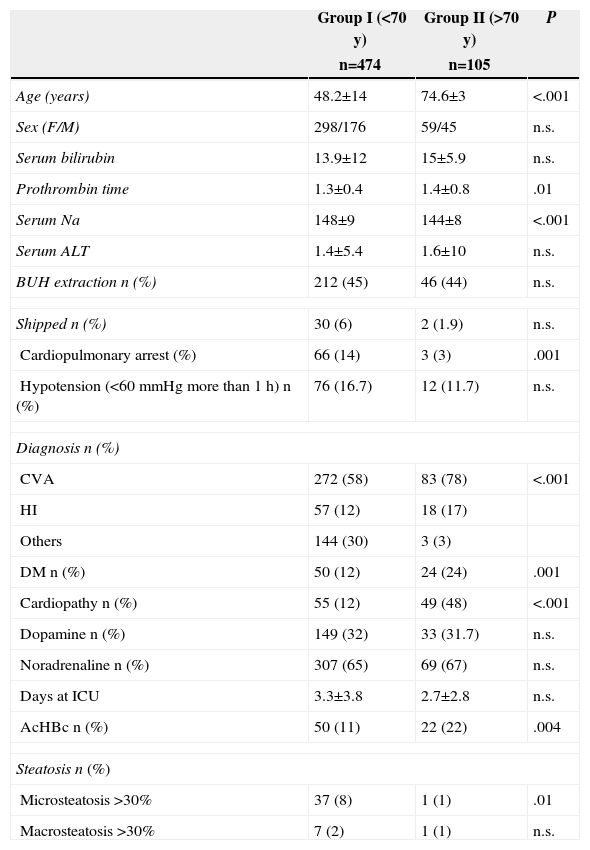
There were no significant differences between the two groups regarding sex, weight, ICU stay, bilirubin, serum prothrombin time, or vasoactive drug requirements. For the older donors, the sodium serum was significantly lower, as well as episodes of cardiopulmonary arrest. The percentage of cerebral vascular accidents (CVA) as a cause of death was more common amongst elderly donors; this group also presented a higher prevalence of comorbidities such as diabetes mellitus, basal cardiopathy and positive AcHBc, compared to the group of donors aged under 70 years. Only two donors aged over 70 years had steatosis of over 30% in their liver biopsy (one with macrosteatosis >30%, and another with microsteatosis >30%) (Table 1).
Comparison of the Variables Studied in the Donors.
| Group I (<70 y) | Group II (>70 y) | P | |
|---|---|---|---|
| n=474 | n=105 | ||
| Age (years) | 48.2±14 | 74.6±3 | <.001 |
| Sex (F/M) | 298/176 | 59/45 | n.s. |
| Serum bilirubin | 13.9±12 | 15±5.9 | n.s. |
| Prothrombin time | 1.3±0.4 | 1.4±0.8 | .01 |
| Serum Na | 148±9 | 144±8 | <.001 |
| Serum ALT | 1.4±5.4 | 1.6±10 | n.s. |
| BUH extraction n (%) | 212 (45) | 46 (44) | n.s. |
| Shipped n (%) | 30 (6) | 2 (1.9) | n.s. |
| Cardiopulmonary arrest (%) | 66 (14) | 3 (3) | .001 |
| Hypotension (<60mmHg more than 1h) n (%) | 76 (16.7) | 12 (11.7) | n.s. |
| Diagnosis n (%) | |||
| CVA | 272 (58) | 83 (78) | <.001 |
| HI | 57 (12) | 18 (17) | |
| Others | 144 (30) | 3 (3) | |
| DM n (%) | 50 (12) | 24 (24) | .001 |
| Cardiopathy n (%) | 55 (12) | 49 (48) | <.001 |
| Dopamine n (%) | 149 (32) | 33 (31.7) | n.s. |
| Noradrenaline n (%) | 307 (65) | 69 (67) | n.s. |
| Days at ICU | 3.3±3.8 | 2.7±2.8 | n.s. |
| AcHBc n (%) | 50 (11) | 22 (22) | .004 |
| Steatosis n (%) | |||
| Microsteatosis >30% | 37 (8) | 1 (1) | .01 |
| Macrosteatosis >30% | 7 (2) | 1 (1) | n.s. |
ALT, alanine aminotransferase; CVA, cerebral vascular accident; DM, diabetes mellitus; BUH, Bellvitge University Hospital; n.s., non significant; Na, sodium; HI, head injury.
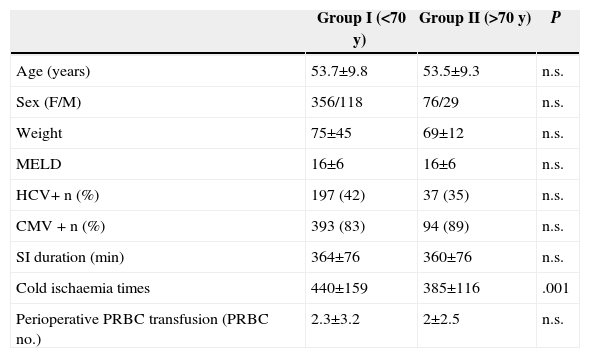
As for the recipients’ variables (Table 2), the age, sex, weight, MELD, presence of HCV or CMV, duration of intervention or perioperative blood transfusion were comparable in the two study groups, regardless of the donor age. The only variable of statistical significance was the cold ischaemia time of the liver graft, which was lower in the group of elderly donors.
Comparison of Variables Studied in Recipients.
| Group I (<70 y) | Group II (>70 y) | P | |
|---|---|---|---|
| Age (years) | 53.7±9.8 | 53.5±9.3 | n.s. |
| Sex (F/M) | 356/118 | 76/29 | n.s. |
| Weight | 75±45 | 69±12 | n.s. |
| MELD | 16±6 | 16±6 | n.s. |
| HCV+ n (%) | 197 (42) | 37 (35) | n.s. |
| CMV + n (%) | 393 (83) | 94 (89) | n.s. |
| SI duration (min) | 364±76 | 360±76 | n.s. |
| Cold ischaemia times | 440±159 | 385±116 | .001 |
| Perioperative PRBC transfusion (PRBC no.) | 2.3±3.2 | 2±2.5 | n.s. |
PRBC, packed red blood cells; CMV, cytomegalovirus; SI, surgical intervention; MELD, Model for End-stage Liver Disease; n.s., non significant; HCV, hepatitis C virus.
The post-transplant days of admission in ICU, hospital stay, and hospital mortality were comparable in both groups. There were no differences either between the incidence of PGD, rejection episodes, or need for retransplant.
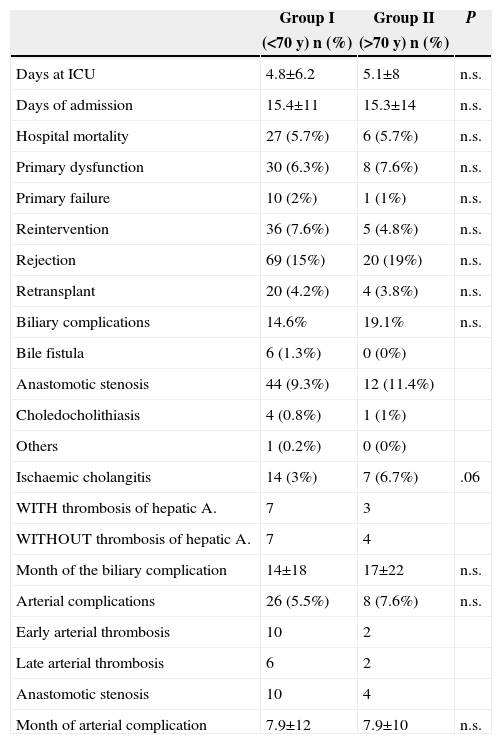
With regard to post-transplant biliary complications, we found that the appearance of postoperative biliary fistula and stenosis of the biliary anastomosis or choledocholithiasis were comparable in the two groups. Of the 105 patients with grafts from donors over 70 years, seven presented ischaemic cholangitis, compared to 14 patients in the group of donors under 70 years. The incidence of arterial complications (arterial thrombosis or anastomotic stenosis) in the group of patients with grafts from younger donors was 5.5%, and in the group of elderly donors it was 7.6%, but these differences were not significant (Table 3).
Post-Transplant Progress and Complications.
| Group I | Group II | P | |
|---|---|---|---|
| (<70 y) n (%) | (>70 y) n (%) | ||
| Days at ICU | 4.8±6.2 | 5.1±8 | n.s. |
| Days of admission | 15.4±11 | 15.3±14 | n.s. |
| Hospital mortality | 27 (5.7%) | 6 (5.7%) | n.s. |
| Primary dysfunction | 30 (6.3%) | 8 (7.6%) | n.s. |
| Primary failure | 10 (2%) | 1 (1%) | n.s. |
| Reintervention | 36 (7.6%) | 5 (4.8%) | n.s. |
| Rejection | 69 (15%) | 20 (19%) | n.s. |
| Retransplant | 20 (4.2%) | 4 (3.8%) | n.s. |
| Biliary complications | 14.6% | 19.1% | n.s. |
| Bile fistula | 6 (1.3%) | 0 (0%) | |
| Anastomotic stenosis | 44 (9.3%) | 12 (11.4%) | |
| Choledocholithiasis | 4 (0.8%) | 1 (1%) | |
| Others | 1 (0.2%) | 0 (0%) | |
| Ischaemic cholangitis | 14 (3%) | 7 (6.7%) | .06 |
| WITH thrombosis of hepatic A. | 7 | 3 | |
| WITHOUT thrombosis of hepatic A. | 7 | 4 | |
| Month of the biliary complication | 14±18 | 17±22 | n.s. |
| Arterial complications | 26 (5.5%) | 8 (7.6%) | n.s. |
| Early arterial thrombosis | 10 | 2 | |
| Late arterial thrombosis | 6 | 2 | |
| Anastomotic stenosis | 10 | 4 | |
| Month of arterial complication | 7.9±12 | 7.9±10 | n.s. |
A., artery; n.s., non significant; ICU, intensive care unit.
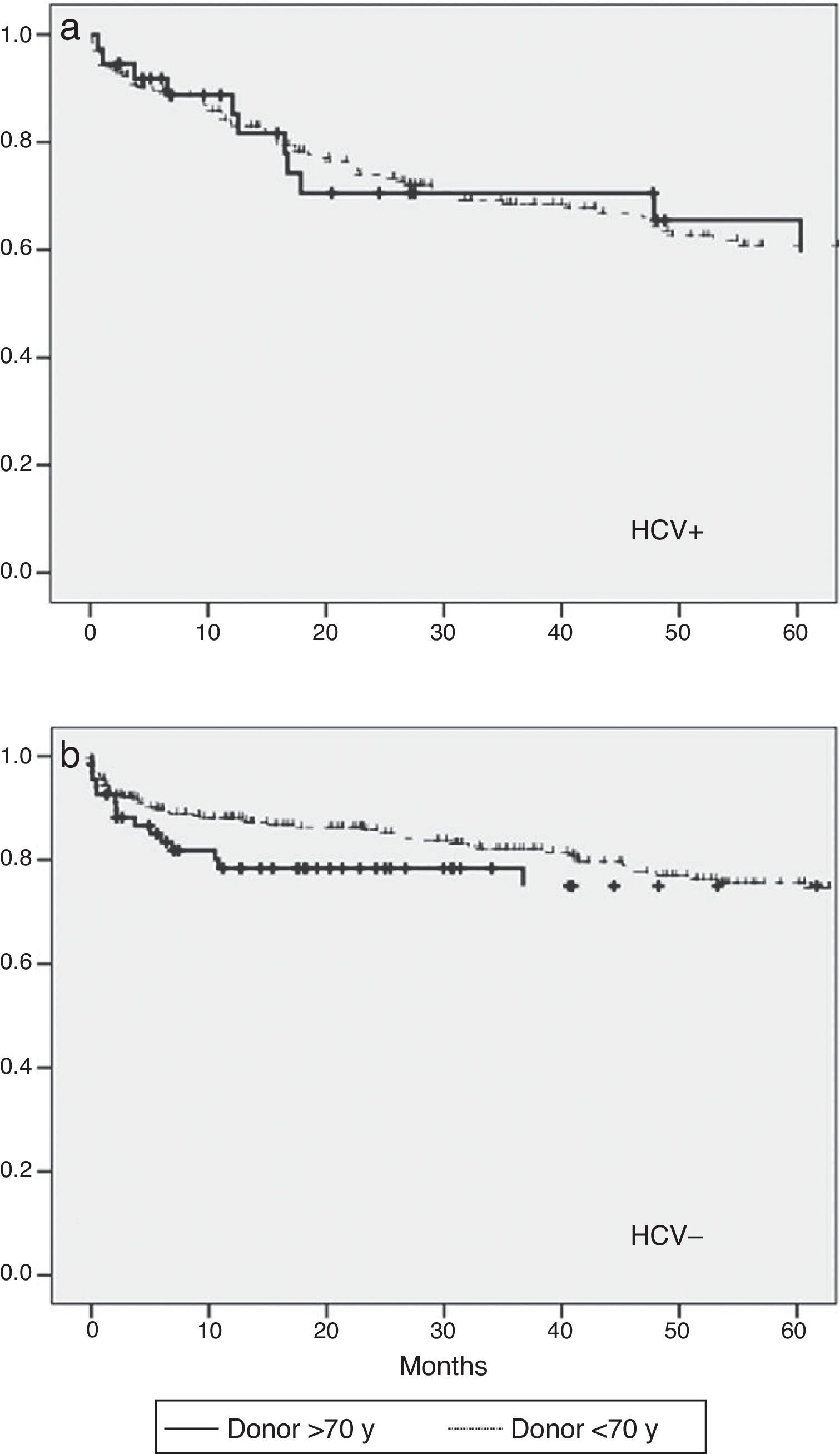
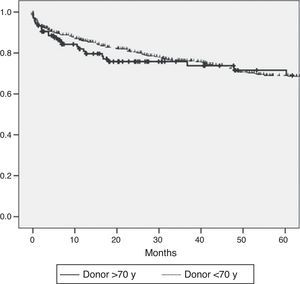
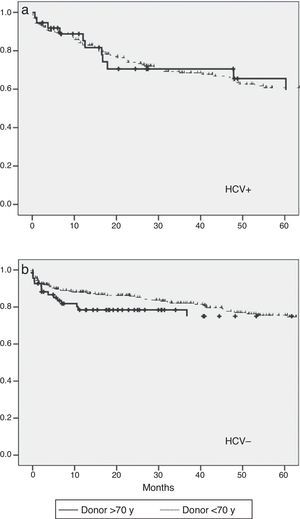
The actuarial survival after five years was analysed using the Kaplan–Meier method, without identifying statistically significant differences between the two study groups (Fig. 1). Even though the study was not specifically designed to assess the post-transplant evolution of patients with HCV, given the relevance of research on the effect of the age of donors on patients that have received transplants due to cirrhosis due to hepatitis C, we have analysed survival rates depending on the presence of this virus. When the analysis is conducted separately between positive and negative HCV patients, there are no differences in survival depending on the age of the donors Fig. 2). Conversely, the overall survival of patients with HCV is lower in relation to non HCV, regardless of donor age.
Due to the growing need for expanding the pool of LT donors, strategies have been developed to increase potential donors. One of these strategies has been the use of marginal grafts, or grafts with extended criteria, for which an increase in the PGF risk and a decrease in patient and graft survival should be expected. Donors with extended criteria currently include more than 50% of the total of donors in the Eurotransplant region.3,12
The advanced age of a liver donor is considered by many authors to be an indicator of poor post-transplant progress. Some even argue that a donor age of over 60 years is the greatest risk factor for PGF.1,11,13 However, disparate results have been published with regard to LTs from older donors. One of the first groups to publish its experience with donors over 70 years was Emre et al.,14 which concluded that there were no significant differences in the post-transplant progress when compared to a control group of donors aged under 70 years. More recently, other groups argued that age alone does not adversely affect progress after a LT, rather, it is necessary to aggregate several risk factors to see a harmful effect on post-transplant progress.3,15–17 Specifically, Anderson et al.17 stated that age alone should not be a contraindication for liver donation, although, even if it is true that grafts from older donors are more susceptible to damage of the endothelial cells due to the effect of ischaemia/reperfusion; but if ischaemia times are maintained below 8h, then post-transplant liver function is comparable with LT from younger donors.
The study conducted at our centre in 200011 was contrary to these results, as it was concluded that LTs from donors aged over 70 years had a greater mortality in the long term and higher graft loss. In spite of this, in our centre and due to the scarcity of organ donors, such organs continued to be used, paying special attention not to include additional risk factors such as long ischaemia times or macrovesicular steatosis >30%.
Taking as a reference a study that we published in 2000, we wanted to review the results in our centre during the years after its publication.
In our analysis, PGF and PGD were similar in both study groups. The actuarial survival of patients depending on donor age was also comparable, as well as the need for re-transplant, which leads us to conclude that the survival of liver grafts in both groups was also similar.
In all cases, ischaemia times for the group of elderly donors were below 9h, as recommended by the group of Cescon et al.18 Only one patient out of 105 in the group of elderly donors had macrovesicular steatosis >30%. This was because in donors aged over 70 years, a liver graft was abandoned in the presence of macroscopic steatosis. We also believe it should be noted that the group of elderly patients had significantly lower natraemia (P=.001) than the control group, attributable to better maintenance of homeostasis after brain death.
We also believe that both short ischaemia times, the absence of macrovesicular steatosis and the selection of patients who had suitable pre-transplant maintenance (as shown by their lower hypernatraemia) was key in obtaining favourable results in our study, and has allowed us to safely increase our donor pool using this type of liver graft, as may be extrapolated from the fact that elderly donors have increased by 10% during the study period.
Stewart et al. noted an increase in the graft loss risk due to late thrombosis of the hepatic artery in donors aged over 70 years,6 although more recent publications describe a gradual decrease of the incidence of this complication over time, due to improved surgical techniques.19 In our analysis we found no differences in the incidence of early or late arterial thrombosis, nor in the stenosis of the arterial anastomosis between the two groups studied.
It should be noted that, although the differences in the incidence of ischaemic cholangitis were not significant (P=.06), the appearance of this complication in the group of donors aged over 70 years was twice that of the control group. This fact does not appear to influence progress in the short or long term, since the survival of patients and re-transplant requirements are comparable for both groups.
Finally, the use of grafts from elderly donors in patients with HCV has been associated with worse progress post LT, mainly due to an aggressive recurrence of the virus.7 Although this study was not meant to analyse the progress of transplant patients with HCV in depth, we noted that the survival of these patients was unrelated to the age of the organ donors. We can conclude, as it is known, that the survival of patients with HCV is overall lower than that of patients without HCV, regardless of the age of the donor.8–10
The favourable results obtained are probably secondary to the application of stricter selection criteria for donors aged over 70 years. Even though this information is not available, the liver rejection percentage for the group of elderly donors might be higher than for the lower age group, and stricter selection criteria could be a key factor to obtain the results described.
ConclusionIn our experience the use of liver grafts from donors aged over 70 years, where additional risk factors such as prolonged ischaemia times, steatosis or hypernatraemia are avoided, does not compromise the results of a LT in the short or long term, and allows for a reduction in the number of patients on the waiting list.
AuthorshipMils K (Data acquisition and gathering, analysis and interpretation of results, article drafting). Lladó L (Design, data acquisition and gathering, analysis and interpretation of results, article drafting, critical review and approval of the final version).
Fabregat J (Data acquisition and gathering, critical review and approval of the final version). Baliellas C (Data acquisition and gathering, critical review and approval of the final version). Ramos E (Data acquisition and gathering, critical review and approval of the final version). Secanella L (Data acquisition and gathering, critical review and approval of the final version). Busquets J (Data acquisition and gathering, critical review and approval of the final version).
Pelaez N (Data acquisition and gathering, critical review and approval of the final version).
Conflict of InterestThe authors declare that there are no conflicts of interest.
Please cite this article as: Mils K, Lladó L, Fabregat J, Baliellas C, Ramos E, Secanella L, et al. Resultados del trasplante hepático con donantes de más de 70 años. Cir Esp. 2015;93:516–521.
This document has been presented orally at 12th Catalan Transplant Congress 2012 in Barcelona and as a poster at the Congress of the Spanish Society of Liver Transplantation, 2013 in Cordoba, where received award for Best Poster of the Congress.