We present the case of a 35-year-old male patient who came to our consultation with abdominal distension that had been developing over the previous 10h, with no other symptoms. The distension had begun immediately after free-diving to a depth of 39m. His personal history included left inguinal hernioplasty. On physical examination, the patient was in good general condition: no fever, hemodynamically stable and eupneic. The abdomen was soft, with great distension and generalized hyperresonance as well as crepitus upon palpation of the umbilical region, which presented a non-complicated umbilical hernia. The patient had no pain during abdominal palpation or any signs of peritoneal irritation. Air-fluid levels were detected. The remaining physical exploration was unremarkable.
Blood analysis showed 14,490 leukocytes (normal formula), GOT 53U/l, GPT 74U/l, CPK 208U/l, CKMB 40U/l and myoglobin 46.49ng/ml. The remaining determinations, including coagulation and venous blood gases, had values within normal ranges.
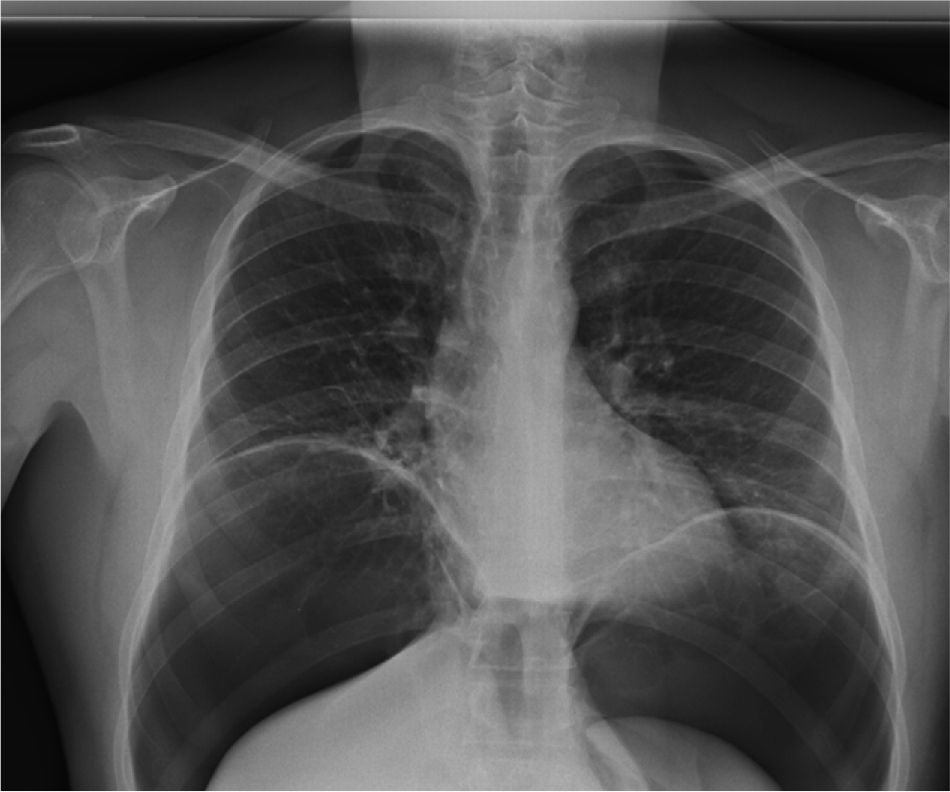
When we observed the shape of the transverse colon wall on standing chest and abdominal radiographs (Figs. 1 and 2), a normal intraluminal hydro-air pattern was seen with extraluminal free air accumulated in the subdiaphragm region as well as displacement of the lung bases and viscera of the upper abdomen. In addition to the voluminous pneumoperitoneum pushing the abdominal content in the posterior direction and umbilical hernia with fat and gas content, thoracoabdominal CT also revealed pulmonary laminar atelectasis due to compression and minimal pericardial effusion. No intraperitoneal free fluid, intravascular gas or disruption of hollow organs was observed. Electrocardiogram was normal.
Given the good general status of the patient, the lack of significance found in the analyses and the lack of evidence of perforation, we opted for conservative management with no oral intake, parenteral nutrition, normobaric high-flow oxygen therapy (MV at 35%–8lpm) and low-molecular-weight heparin at a prophylactic dosage. Oral tolerance was started 48h later, and enteral nutrition was reinstated without complications after 72h. During hospitalization, the patient passed gas and had normal bowel movements with no pathologic production. He presented isolated fever (38.1°C) on the third day after hospitalization, which responded to the administration of an antipyretic. When the patient was discharged after 30 days under observation, he was asymptomatic, with normal lab work and radiological persistence of the pneumoperitoneum, although much less than when he was first hospitalized. At the 60-day follow-up visit, we observed complete resolution of his symptoms.
There are few reports in the literature about pneumoperitoneum associated with diving incidents, including only 9 cases published since 1977.1–6 Perforation of a hollow organ should first be suspected as it is frequently the origin of pneumoperitoneum, since less than half of perforated patients show signs of peritoneal irritation.2 As for the mechanism by which the gas reaches the peritoneum in the absence of organ perforation, many theories have been postulated. It has been accepted that the most probable origin of this air is the lungs. Several authors have demonstrated in animal models that after the rupture of distended alveoli, the gas that is released dissects pleural bullas and penetrates the pleural space. If the pressure continues, the air enters the retroperitoneum and the subcutaneous cell tissue7 through dissection of muscle planes and diaphragm defects that lead to the contact between the retroperitoneal and pleural cavities. Anatomical alterations secondary to childbirth or previous abdominal surgery, as in this case, could favor the appearance of pneumoperitoneum. Another possible mechanism is the passage of air under pressure from the pleura through the thoracic duct to the abdominal cavity8 in a retrograde pathway favored by sudden ascent. It could be possible to consider a mechanism similar to what happens during colonoscopy, where, secondary to the increased intraluminal pressure, microperforations of the colon may occur in areas with thinner walls (for instance, in the diverticula) or in the lymphatic vessels in this area that are small enough to allow for gas to escape without the extravasation of any intraluminal liquid content, then closing up after the distension subsides. Or the air could even pass through walls that are intact but are less thick, with no demonstrated perforation.9
The diagnosis of pneumoperitoneum is based on symptoms and radiology. Abdominal distension and compromised respiratory function are the most frequent symptoms and are directly related to the amount of air leaked. A simple radiograph in the standing position is diagnostic, although tomography is more sensitive and is able to rule out organ perforation. Another useful tool is radiology with hydrosoluble contrast, which locates possible perforations.
If there is clinical compromise or evidence of perforation, the approach is usually surgical with emergency laparotomy, although 10% of cases can be managed conservatively.10 According to the literature, the therapeutic approach in pneumoperitoneum after barotrauma is varied: hyperbaric chamber, puncture-evacuation of the peritoneal cavity, a wait-and-see approach with no oral intake and parenteral nutrition, or surgical intervention. There is no established protocol for the management of these cases. Our criteria are that if there is no evidence of perforation of a hollow organ, there are no other manifestations of barotrauma and the clinical situation allows for it, conservative management can be used, as in the case that we have presented.
Please cite this article as: Rosado Dawid NZ, Peraza Casajús JM, Bodega Quiroga I. Neumoperitoneo secundario a barotrauma tras accidente de buceo. Cir Esp. 2014;92:368-370.