Perivascular epithelioid cell tumours (PEComa) are rare mesenchymal neoplasms that express myogenic and melanocytic markers.
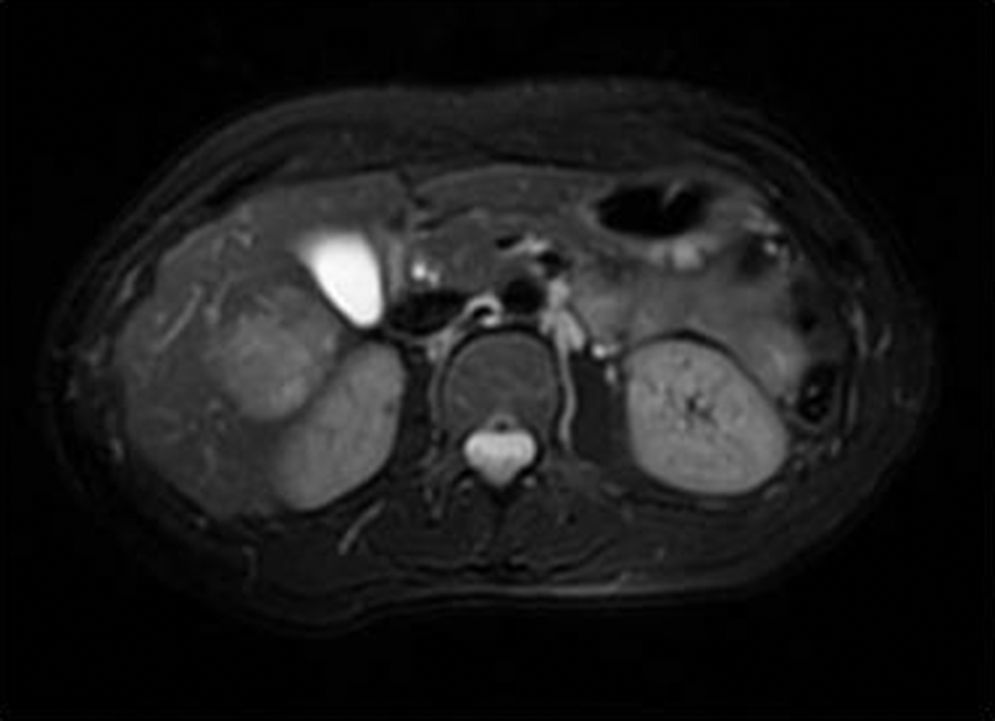
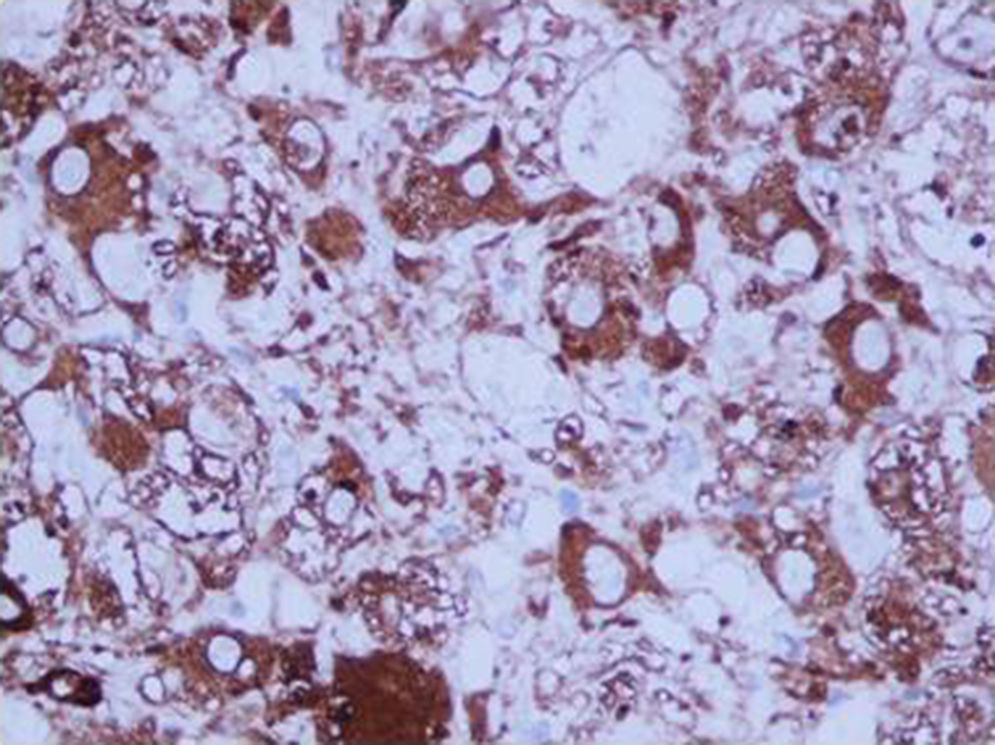
We present the case of a 45-year-old woman who was being studied for dyspepsia and elevated Ca 19.9. CT detected a 4-cm lesion in liver segments V/VI, with heterogenous enhancement in arterial phase and almost complete washout in portal phase; the uterus was myomatous, with a left adnexal cyst. MRI revealed a hyperintense lesion in T2 that was hypointense in T1, with uptake in the arterial phase and washout in portal phase, except in the periphery, which presented delayed enhancement (Fig. 1). A follow-up ultrasound demonstrated growth of the mass, and therefore we decided on resection; the patient had an uneventful recovery. The pathology study determined the tumour was a PEComa measuring 3.5cm in diameter, with free surgical margins, marked nuclear pleomorphism, and no presence of mitosis. The proliferation rate (Ki67) was 3%–5% and the tumour expressed HMB-45, Melan-A (Fig. 2), 1A4 and HHF35 with uncertain behaviour. Afterwards, and given the suspicion that the hepatic mass was probably metastasis of gynaecological origin, hysterectomy and double adnexectomy were carried out. The histopathologic study showed a myomatous uterus and 5-cm leiomyoma that expressed HHF35 and was negative for melanocytic markers (HMB-32 and Melan-A), with no other adnexal pathological findings.
PEComas are rare mesenchymal neoplasms where the epithelioid cells express muscle (actin, desmin) and melanocytic (HMB-45; Melan-A, MiTF) markers.1 Less than 50 cases of hepatic PEComa have been described.5 They predominantly affect women with a mean age of 46.3 The most frequent location is genital (especially the uterus), followed by the genitourinary apparatus, gastrointestinal tract and retroperitoneum; it is also associated with tuberous sclerosis.2–4 Symptoms are variable: from no symptoms to discomfort in the right hypochondrium or acute abdomen.
The degree of diagnostic error by imaging techniques is higher than 90%,4 so it is therefore difficult to make a correct preoperative diagnosis. The differential diagnosis should include: focal nodular hyperplasia, hemangioma, hepatocarcinoma, adenoma, metastasis of endocrine or renal tumours, etc.
Standard treatment is radical surgery, both for the primary tumour as well as local recurrence or distant metastasis. The role of chemotherapy and radiotherapy is uncertain; these therapies are often considered in cases of locally advanced disease, local recurrence or distant metastasis, although their results are arguable.1,2,4
The prognosis is difficult to establish because of the lack of understanding about the biological behaviour of these tumours and the variety of results in the few studies published. According to some authors, size >5cm, mitotic rate >1/50 HPF, necrosis, cells with nuclear pleomorphism, infiltrating growth or high nuclear grade are considered factors for poor prognosis and associated with more aggressive tumour behaviour, recurrence and/or distant metastasis.2 Folpe1,6 proposed a classification based on these criteria: (a) benign, if there are none of the former parameters; (b) uncertain biological potential, if only size >5cm or giant cells with nuclear pleomorphism are found; and (c) malignant, with more than 2 criteria for poor prognosis.
In our patient, the lesion was classified as having an uncertain diagnosis, and the case was presented at a multidisciplinary committee meeting for gastrointestinal tumours, at which time close follow-up of the patient was decided upon.
As stated by Khaja,5 we believe that, in cases of space-occupying lesions of the liver with uncertain radiological diagnosis, the treatment of choice is resection with free margins.
Conflict of InterestsThe authors declare no conflict of interests.
Please cite this article as: Arribas Jurado M, Revollo I, Rubio Fernández A, Galeano Díaz F, Blanco Fernández G. PEComa hepático. Cir Esp. 2015;93:600–601.