Splenic lymphangiomas are rare benign neoplasms, characterized by cystic dilatations of the lymphatic vessels in the parenchyma of the spleen.1
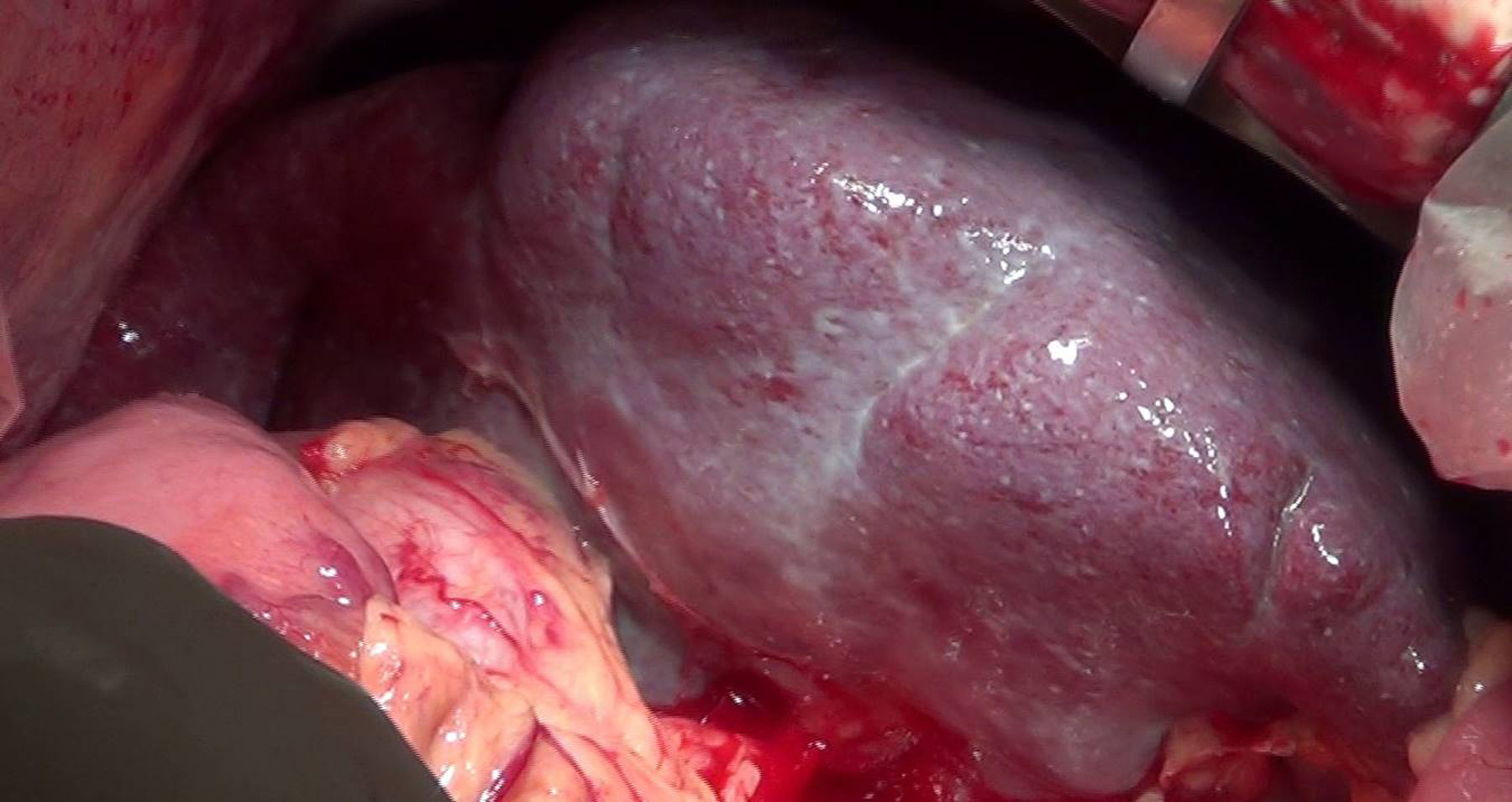
We present the case of a 62-year-old man with a history of tuberculosis and syphilis, who had been diagnosed with Crohn's disease 20 years earlier, requiring multiple hospitalizations and 2 previous surgical interventions: the first, 10 years before with resection of the proximal jejunum and ileocecum; and the second, 5 years before with resection of an ileal segment and the previous ileocolic anastomosis. He presented symptomatic stenosis of the first jejunal loop secondary to Crohn's disease and an abdominal CT image of a large splenomegaly (Fig. 1), suggestive of a splenic hydatid cyst with signs of portal hypertension. The serology for echinococcosis was negative. Midline laparotomy was used to conduct adhesiolysis, resection of the jejunal stenosis due to Crohn's and splenectomy. We observed a very enlarged, multilobular spleen (Fig. 2) measuring 18.5cm at its widest diameter, which had multiple cystic cavities that were whitish, with a pathology diagnosis of splenic lymphangiomatosis. The postoperative course was uneventful and no signs of lymphangiomas were found in other areas.
Lymphangiomas are benign tumors that originate from a congenital malformation of the lymphatic system that causes lymphangiectasis secondary to the absence of normal communication between the lymphatic ducts, which end at the bottom of a sac and slowly dilate to form a cyst. Most lymphangiomas appear in the neck and axillae (95%), where they are called cystic hygromas. All other locations, including abdominal locations, are uncommon and represent 5% of all cases.3 When different organs are compromised, this lymphatic alteration is called “systemic lymphangiomatosis”.4 When splenic lymphangiomas appear, they may affect the spleen alone, or they may compromise multiple organs.1 On rare occasions, they may also form part of the Klippel-Trenaunay syndrome.6 Lymphangiomatosis that affects the spleen alone is very rare, and only 8 cases have been reported between 1990 and 2010.2 They mainly affect females, and 80%–90% are detected within the first 2 years of childhood.3,7,8
In most cases, isolated splenic lymphangiomas are asymptomatic and incidentally detected on ultrasound or CT scan of the abdomen performed for another reason, as occurred in our patient. In large lesions, symptoms may include pain in the left hypochondrium, nausea, vomiting, loss of appetite, symptoms of abdominal distension and possibly the presence of palpable splenomegaly. Infection or rupture may present with symptoms of acute abdomen. Cases have been reported of giant lymphangiomas complicated with consumption coagulopathy, bleeding, hypersplenism and portal hypertension. In very large lesions, diaphragmatic immobility may occur in conjunction with the onset of atelectasis or pneumonia, while on rare occasions hypertension due to compression of the renal artery by the splenic mass has been observed.5
Imaging studies used in the diagnosis of splenic disease include abdominal ultrasound, CT scan and MRI. Color Doppler echocardiography can demonstrate cyst vascularization.3,7 A characteristic “Gruyère cheese” image has been described on ultrasound, CT scan and MRI, with images of multiple and well-defined cysts. CT scan is the ideal diagnostic method and has been established as the preoperative study of choice.1
Although in recent years the use of imaging-guided fine-needle aspiration biopsies has increased in a large variety of benign and malignant splenic lesions,3 there are authors who consider it a contraindication due to the risk of bleeding and the limited amount of tissue for correct diagnosis.2
The differential diagnosis should include lesions with similar tomographic characteristics, such as hemangiomas, primary or metastatic tumors, vascular infarction, infection, granulomatous disease, previous trauma and simple cysts.1 Serology for Echinococcus can establish the definitive diagnosis of the hydatid origin of the lesion.
The treatment of choice for splenic lymphangiomas is complete surgical resection. Some authors prefer conservative treatment in cases of small asymptomatic lesions that are incidentally detected, reserving splenectomy for large, multiple or symptomatic lesions.5,6 Conservative treatment of splenic lymphangiomas with interferon-alpha has been conducted in a child by Reinhardt et al.9 successfully and with good tolerance. However, optimal treatment times and doses to cure this disease indefinitely have not yet been determined.3 Laparoscopic splenectomy is becoming the procedure of choice for normal or moderately enlarged spleens, although it may not be suitable for patients with massive splenomegaly. Partial resections have also been used in cases of limited disease; however, in cases of diffuse involvement, the remaining splenic tissue increases the risk of recurrence and consequently the need for a second surgical intervention.5
Prognosis after complete resection is favorable. Recurrence has been reported in 9.5% of patients, mainly due to incomplete resection.5,6
In conclusion, despite its rarity, this disease must be included in the differential diagnosis of splenic lesions with cystic features, such as hydatid cysts.
Please cite this article as: Toval Mata JA, Carrasco Campos J, Ruiz López M, González Poveda I, Mera Velasco S. Linfangioma quístico esplénico. Cir Esp. 2017;95:53–54.