To determine the safety of percutaneous dilatational tracheostomy (PDT) on hepatic allograft recipients.
Patients and methodsWe reviewed the records of patients who underwent liver transplantation between October 2007 and April 2013, followed by PDT. In this time period, 25 liver recipients underwent PDT in our intensive care unit. We recorded severity index scores such as APACHE II and SAPS II, number of days since intubation, ratios of PaO2/FiO2 (arterial oxygen pressure to fraction of inspired oxygen), coagulation study findings, complications, and procedure-related mortality rates. We compared these records with the general ICU population and literature reports.
ResultsThe median age was 58 (IC range 47–65) and 64% were men. The median time since intubation to PDT was 11 days (IC range 6.5–15.5) and from transplant to PDT 12 days. The median ratio of PaO2/FiO2 was 212 (IC range 177–259). The median platelet count was 89 (IC range 37–149), significantly lower than the general ICU population (272 (IC range 186–381) P=.001).
Complications were infrequent and included clinically remarkable major bleeding 8% (vs 0.3% in general ICU population; P=.005), peristomal infection of 4% and ventilator-associated pneumonia of 16% (vs 2.8% in general ICU population; P=.007). There were no deaths associated with the procedures.
ConclusionPDT was tolerated well in recipients of liver allografts and had a relatively low risk of major complications and a low procedure-related mortality rate.
Determinar la seguridad de la traqueotomía percutánea por dilatación (TPD) en los pacientes receptores de un trasplante hepático.
Pacientes y métodoSe revisaron las historias de los pacientes ingresados para control postoperatorio de trasplante hepático (n=291) entre octubre de 2007 y abril de 2013. En este periodo 25 pacientes trasplantados hepáticos requirieron la realización de una TPD. Se analizaron entre otros: índices de gravedad (APACHE II y SAPS II), número de días desde la intubación, razón PO2/FiO2, estudios de coagulación y complicaciones. Se compararon los resultados con la población general de pacientes críticos y las publicaciones similares en la literatura.
ResultadosLa mediana de edad fue 58 años (RIC 47–65) y el 64% de los pacientes eran varones. La mediana desde la intubación hasta la TPD fue 11 días (RIC 6,5–15,5) y desde el trasplante hasta la TPD, 12 días. La mediana de la PO2/FiO2 fue de 212 (RIC 177–259). El recuento de plaquetas mostró valores menores en los pacientes trasplantados 89 (RIC 37–149) vs. 272 (RIC 186–381), p=0,001.
Las complicaciones incluyeron: sangrado clínicamente significativo, 8 frente al 0,3% de los pacientes críticos no trasplantados (p=0,005), infección del estoma en el 4% y neumonía asociada a ventilación mecánica en el 16% (frente al 2,8% del resto de pacientes críticos, p=0,007). No hubo muertes relacionadas con el procedimiento.
ConclusionesLa TPD es bien tolerada en los pacientes ingresados en UCI para el control postoperatorio de trasplante hepático y presenta una tasa relativamente baja de complicaciones graves y mortalidad relacionada con el procedimiento.
Patients who have undergone orthotopic liver transplant (OLT) have some peculiarities regarding their monitoring and treatment requirements, including immunosuppression. For this reason, they are usually relocated after surgery in a specific area for better compliance with performance protocols1; therefore, postoperative care, especially in the immediate postoperative period, has become one of the competences in intensive care units (ICU). Both the surgical procedure and the postoperative care of OLT are processes with a relatively low morbidity and mortality when performed by experienced teams; however, they are not exempt from possible serious complications. Among the most common postoperative complications of OLT, we would have to include those relating to implanted organ dysfunction (primary graft dysfunction, acute rejection, arterial thrombosis, etc.), as well as immunosuppressive treatment-induced infections; in particular, pneumonia and its associated respiratory failure are the ones that make it necessary to perpetuate mechanical ventilation.2–5 Given the need for this prolonged mechanical ventilation, recent evidence suggests that performing a tracheostomy within a week after the start of mechanical ventilation could have some potential benefits over orotracheal intubation.6–8 An example of this would be a decrease in mechanical ventilation time and ICU stay, as well as a lower incidence of ventilator-associated pneumonia, although these beneficial effects are not constant in the literature.9,10
Despite the documented advantages11–13 of percutaneous dilatational tracheostomy (PDT), there are few studies that have assessed its effectiveness-convenience and checked its safety in patients admitted to the ICU for OLT postoperative control.14,15
With these considerations in mind, the purpose of this study was to assess the results and safety of PDT in a group of patients who underwent OLT through the comparison with other PDT procedures performed on critical patients admitted to our Unit for reasons other than OLT.
Material and MethodsThis study was conducted in a polyvalent Intensive Care Medicine Unit with 32 beds, of which 6 are used for patients undergoing OLT or another solid organ transplantation. Immediate postoperative care is performed in close collaboration between the Unit members assigned to this area and the Departments of General and Digestive Surgery in charge of this activity. These six beds are equipped with the usual computer-based electrocardiographic and haemodynamic monitoring system (ICIP®). Patients admitted for OLT postoperative control are treated under a specific protocol that includes, in addition to the usual controls, measurement of the debits of the different drainage systems used during the surgery, serial evaluation of liver function tests, coagulation tests and tests assessing the potential inflammatory response. The population of this study was composed of patients who underwent OLT and were admitted to our unit during the period between October 2007 and April 2013 and who required PDT (25 patients). In all cases, PDT was performed in situ, at the patient's bedside, by at least two physicians specialised in Intensive Care Medicine or residents of that specialty. The monitoring of the procedure was verified in all cases by a specialist in Intensive Care Medicine.
The indication for the PDT was established according to the standard clinical criteria of the physicians in charge, based on propensity scores attempting to anticipate the eventual need for prolonged mechanical ventilation (including, but not limited to: respiratory failure with radiographic pulmonary infiltrates, low level of consciousness of morphological origin, multiple organ failure, [and] severe malnutrition).
The PDT technique used is a minor variant of the procedure described by Ciaglia in 1985.16 Most of the patients were sedated using deep intravenous sedoanalgesia, with midazolam plus fentanyl and atracurium on an optional basis. Then, the technique was performed following the usual steps.16
After completing the procedure, an arterial blood gas monitoring and a chest X-ray were performed.17
The Portex ULTRAperc® (Smiths Medical) percutaneous tracheostomy kit was used for all the procedures performed.
Variables relating to the patient's baseline condition were prospectively collected (age, sex, comorbidities); those regarding severity index scores on admission (APACHE II, SAPS II and SAPS III), coagulation parameters (activated partial thromboplastin time, platelet count and prothrombin activity), and prior ventilator status (partial arterial oxygen pressure to fraction of inspired oxygen [PO2/FiO2] ratio). Additionally, the number of days of mechanical ventilation before and after PDT, and the reason for their indication were some of the collected variables. Regarding complications, those relating to the procedure (such as bleeding, local infection of the stoma, atelectasis, oesophageal injuries, pneumothorax or death) and those potentially attributable to it (onset of pneumonia, delayed bleeding of the stoma, etc.) were considered.
With respect to bleeding complications and in order to minimise observer subjectivity, the following consideration was taken into account:
- –
Major bleeding: requiring surgical revision or a drop in haematocrit >8 points.
- –
Minor bleeding: scarce bleeding reported in at least four of the six nurses’ progress notes following the PDT procedure.
Regarding infectious complications, the presence of inflammatory signs on the edges of the stoma was considered as tracheostomy infection. A simple chest X-ray was performed for the post-procedure diagnosis of atelectasis or pneumothorax. For other complications, the usual diagnostic criteria were used.
For study purposes and regarding patients’ final outcome at discharge from the ICU, three possibilities were contemplated: death during ICU admission due to any cause; discharge from the ICU to the hospitalisation ward with the tracheostomy tube in place and discharge from the ICU to the ward once withdrawal of the tracheostomy tube was well tolerated.
In all elective procedures, informed consent from patients or their legal representatives was obtained.
Statistical AnalysisThe PDT results from the group of 25 patients with OLT (OLT patients) were compared with those from the 781 patients having undergone PDT whose reason for admission to the ICU was other than OLT postoperative control (non-OLT patients). Variables were considered based on their distribution. The Chi-square test was used for categorical variables. Abnormal distribution variables were compared by means of the Mann–Whitney [sic: Whitney] U-test.
The Statistical Package for the Social Sciences (SPSS), version 20.0, was used for the analysis of the data collected.
ResultsDuring the study period, 291 patients were treated in our unit for OLT postoperative control. Of these patients, 25 (8.6%) had complications requiring prolonged mechanical ventilation, and tracheostomy was indicated, carried out via PDT in all cases. During the study period, none of the OLT patients underwent conventional surgical tracheostomy. During the same period, 781 more PDTs were performed on patients admitted to our Unit for reasons other than OLT postoperative care. The final causes that led to the indication for PDT were the following, in order of frequency: respiratory failure in 16 cases, coma in 5 cases and multiple organ failure in the remaining 4 cases.
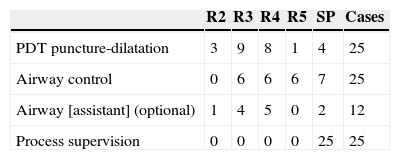
Regarding the different responsibilities in the performance of the procedure, direct supervision was undertaken by an Intensive Care Medicine specialist in all cases. The percutaneous puncture and subsequent dilation were performed by a specialist physician or senior resident, except for three cases where they were performed by a junior third-year resident (Table 1).
Responsibilities in the Performance of the 25 PDT Cases.
| R2 | R3 | R4 | R5 | SP | Cases | |
|---|---|---|---|---|---|---|
| PDT puncture-dilatation | 3 | 9 | 8 | 1 | 4 | 25 |
| Airway control | 0 | 6 | 6 | 6 | 7 | 25 |
| Airway [assistant] (optional) | 1 | 4 | 5 | 0 | 2 | 12 |
| Process supervision | 0 | 0 | 0 | 0 | 25 | 25 |
SP: specialist physician; R2: second-year resident; R3: third-year resident; R4: fourth-year resident; R5: fifth-year resident; PDT: percutaneous dilatational tracheostomy.
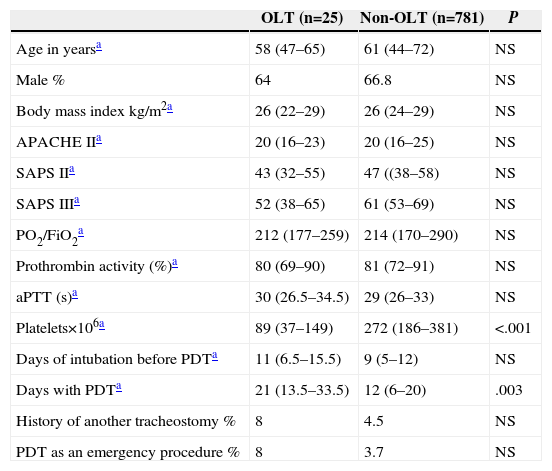
Baseline characteristics of OLT and non-OLT patients are shown in Table 2. In comparison with non-OLT patients, OLT patients showed, as the only statistically significant difference, a lower platelet count and a greater number of days wearing the tracheostomy tube during their stay in the ICU. Also observed was a non-statistically significant trend towards performing PDT earlier in non-OLT patients than in OLT patients.
Patient Characteristics.
| OLT (n=25) | Non-OLT (n=781) | P | |
|---|---|---|---|
| Age in yearsa | 58 (47–65) | 61 (44–72) | NS |
| Male % | 64 | 66.8 | NS |
| Body mass index kg/m2a | 26 (22–29) | 26 (24–29) | NS |
| APACHE IIa | 20 (16–23) | 20 (16–25) | NS |
| SAPS IIa | 43 (32–55) | 47 ((38–58) | NS |
| SAPS IIIa | 52 (38–65) | 61 (53–69) | NS |
| PO2/FiO2a | 212 (177–259) | 214 (170–290) | NS |
| Prothrombin activity (%)a | 80 (69–90) | 81 (72–91) | NS |
| aPTT (s)a | 30 (26.5–34.5) | 29 (26–33) | NS |
| Platelets×106a | 89 (37–149) | 272 (186–381) | <.001 |
| Days of intubation before PDTa | 11 (6.5–15.5) | 9 (5–12) | NS |
| Days with PDTa | 21 (13.5–33.5) | 12 (6–20) | .003 |
| History of another tracheostomy % | 8 | 4.5 | NS |
| PDT as an emergency procedure % | 8 | 3.7 | NS |
NS: non-significant; OLT: orthotopic liver transplantation; PDT: percutaneous dilatational tracheostomy; aPTT: activated partial thromboplastin time.
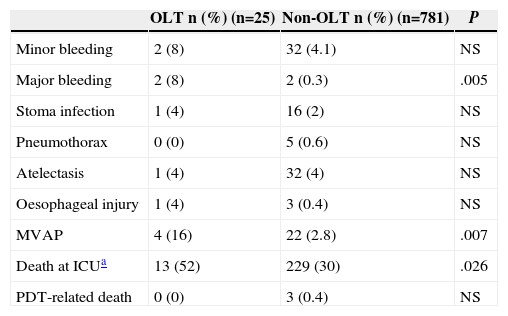
Regarding the incidence of PDT-related complications (Table 3), major bleeding occurred more frequently in the OLT group, but was limited to two patients. In both cases, the bleeding was controlled in the ICU through compression and simple suture of a vessel, without the need for conversion to an open surgical procedure, and without serious complications endangering the patients’ lives. With respect to the incidence of mechanical ventilator-associated pneumonia (MVAP), a significantly higher rate was observed in the OLT group, as compared to the control group (non-OLT).
PDT-associated Complications.
| OLT n (%) (n=25) | Non-OLT n (%) (n=781) | P | |
|---|---|---|---|
| Minor bleeding | 2 (8) | 32 (4.1) | NS |
| Major bleeding | 2 (8) | 2 (0.3) | .005 |
| Stoma infection | 1 (4) | 16 (2) | NS |
| Pneumothorax | 0 (0) | 5 (0.6) | NS |
| Atelectasis | 1 (4) | 32 (4) | NS |
| Oesophageal injury | 1 (4) | 3 (0.4) | NS |
| MVAP | 4 (16) | 22 (2.8) | .007 |
| Death at ICUa | 13 (52) | 229 (30) | .026 |
| PDT-related death | 0 (0) | 3 (0.4) | NS |
Expressed as number of cases (percentage).
MVAP: mechanical ventilator-associated pneumonia; OLT: orthotopic liver transplantation; PDT: percutaneous dilatational tracheostomy; ICU: intensive care unit.
With regard to the patients’ final outcome at discharge from the ICU, those in the OLT group had a higher mortality in the Unit as compared with the non-OLT patients (52 vs 30%; P=.026). There was also a higher proportion of patients who underwent tracheostomy tube removal before being discharged to the ward, in favour of non-OLT patients over OLT patients (25 vs 8%; P=.007).
Regarding the percentage of total complications in our series, no significant differences have been found based on the performance of the procedure by an ICU R3 (13.9%), R4 (12.4%), R5 (11.6%) or a consultant (13.5%).
DiscussionThe PDT described by Ciaglia in 198516 has been widely accepted as an alternative to conventional surgical tracheostomy. Some of its main advantages include that it can be easily performed at the patient's bedside by physicians not specifically trained in the surgical field, the rapidity of its performance and reduced cost. In addition, PDT seems to entail less complications.18 Probably for all these reasons, it has become, in many cases, the technique of choice when performing a tracheostomy in critically ill patients.19–22
The practice of PDT in the immediate postoperative period of OLT patients appears to be a safe technique, comparable to that performed on other patients. This statement must be weighed against the fact that evidence of major bleeding, in our series, was more frequent in OLT patients. While this may be attributed to coincidence, as it occurred in only two cases within a relatively small number of patients, it cannot be ruled out that a greater tendency towards bleeding in OLT patients may be attributable to the lower number of platelets associated with this group and the potential platelet dysfunction. Our results coincide with the series of Andrew et al.,14 which shows two major bleeding complications in the greatest published series of patients who underwent PDT in the postoperative period of solid organ transplantation. Similarly, the aforementioned study refers to comorbidity conditions at the time of PDT, but does not provide an assessment of the usual prognostic severity scores (APACHE, SAPS).
Despite these considerations, in view of our data, in the performance of any invasive procedure, including PDT, it is necessary to be particularly cautious and take into consideration that OLT patients often have severe coagulation disorders and receive large amounts of blood products, including platelet concentrates, which are potentially dysfunctional, and may put them at a high risk of experiencing bleeding complications.23
Regarding infectious complications, only one patient from the OLT group had infection of the tracheostomy stoma, which accounts for a 4% incidence, similar to that usually reported in the literature.24 Although in the study by Andrew et al., the incidence of MVAP is not mentioned, in our case, four patients (16%) from the OLT group presented it. This complication implies 6 cases of pneumonia per 1000 ventilator days (6/1000), a rate more than 3 times that of the non-OLT group (1.7/1000 days). This higher incidence of MVAP in the OLT group may lie in the use of immunosuppression, which, even though it is necessary for the treatment of these patients, puts them at a particularly high risk of acquiring infections.
With respect to fatal complications related to the PDT procedure, no case was reported in the OLT group and no significant differences were observed, as expected, as only three fatal cases were recorded in the non-OLT group (0.38%). The three deceased patients from the non-OLT group died due to loss of the airway during the PDT procedure, where reintubation was not possible and was followed by severe desaturation and cardiac arrest. The three cases described showed mean values similar to the rest of the patients in terms of APACHE II (19 vs 20), SAPS II (37 vs 48), body mass index (30 vs 28), age (49 vs 56) and PO2/FiO2 ratio (192 vs 232).
With regard to overall mortality due to causes not related to PDT, in our results, intra-ICU mortality of patients who underwent liver transplantation followed by PDT was 52%, significantly higher than other patients who did not undergo transplantation but required PDT upon admission to ICU (30%). Naturally, the mortality of OLT patients,25 who were not the subject of our study, depends on several factors related to the causes of respiratory failure or impaired consciousness requiring prolonged mechanical ventilation in postoperative, immunodepressed patients with a complicated postoperative period. In their study, Andrew et al., describe an overall in-hospital, all-cause mortality of 55% in patients with solid organ transplantation requiring PDT; this outcome is similar to those of our series.14
There are other series in the literature comprising a small number of patients, such as that of Pirat et al.,15 which gathers data on five transplanted patients who underwent PDT (two liver transplants, two kidney transplants and one heart transplant); therefore, their results are hardly comparable.
A peculiarity of our study, unlike that of Andrew et al., is that PDT in OLT was compared with the rest of PDTs performed. In this sense, our bleeding rate (4.4%) in critical patients who did not undergo transplantation yielded similar results to those described in other series.26
In addition, it should be noted that it has not been possible to compare PDT results with an open surgical tracheostomy control group, since in our centre all tracheostomy procedures in critical patients have been performed using the PDT technique for more than 10 years.
Always considering the greater tendency towards bleeding and the required use of immunosuppression, PDT is nowadays a safe procedure in liver transplant patients, with a relatively low number of complications, similar to that of the general population of ICU critical care patients.
Conflicts of InterestThe authors declare that they do not to have any conflicts of interest.
Please cite this article as: Royo-Villanova Reparaz M, Andreu Soler E, Sánchez Cámara S, Herrera Cateriano GA, Ruiz Rodriguez A, Martinez Martinez M, et al. Utilidad de la traqueotomía percutánea en el postoperatorio inmediato del trasplante hepático. Cir Esp. 2015;93:91–96.