Single parathyroid adenomas are the most common cause of primary hyperparathyroidism (PHP) in our population. Parathyroidectomy is still the only potentially curative treatment and requires preoperative localization imaging studies to perform selective surgery. In patients with negative results on conventional tests, PET/CT has demonstrated higher sensitivity rates.
MethodsA prospective cohort study was designed, including 34 patients diagnosed with PHP between 2017 and 2019, candidates for surgery with negative preoperative localization tests with scintigraphy and MIBI SPECT/CT. All patients underwent PET/CT with 18F-Fluorocholine. The clinical, biochemical, and postoperative outcome results were compared with a control group of 30 patients with positive standard tests.
ResultsHyperfunctional parathyroid tissue was detected in 85% of the patients that had undergone choline PET/CT. The selective resection of the adenoma identified in these patients achieved curative criteria in 87% of the cases without undergoing bilateral cervical surgical exploration. The preoperative levels of PTH, calcemia, and gland weight were significantly lower in this group compared to the control group. No differences were identified in cure criteria or approach between the 2 groups.
ConclusionIn our study, choline PET/CT showed higher detection rates compared to the gold standard. The increase provides the opportunity to perform unilateral selected adenoma resection, especially in patients with smaller adenomas associated with lower calcemia and PTH levels and patients with previous cervical surgery.
La principal causa de hiperparatiroidismo primario en nuestro medio es el adenoma paratiroideo único. La paratiroidectomía se considera el único tratamiento potencialmente curativo y requiere de estudios de imagen de localización preoperatorios para un abordaje quirúrgico dirigido. En pacientes con negatividad en pruebas convencionales, la PET-TC colina ha demostrado tasas de sensibilidad superiores respecto al gold-standard.
MétodosSe diseñó un estudio de cohortes prospectivo que incluyó a 34 pacientes con diagnóstico de hiperparatiroidismo primario entre 2017 y 2019, candidatos a cirugía con pruebas de imagen con gammagrafía y SPECT-TC MIBI negativas. A todos se les realizó una PET-TC con 18F-fluorocolina. Los resultados se compararon con un grupo control de 30 pacientes con pruebas convencionales positivas intervenidos en el mismo período.
ResultadosLa PET-TC colina detectó tejido paratiroideo hiperfuncionante en el 85% de los pacientes con gammagrafía previa negativa. Se realizó resección selectiva del adenoma identificado en estos pacientes, con criterio de curación en el 87% de los casos, sin precisar de exploración cervical bilateral. Los niveles de PTH, calcemia y el peso glandular fueron significativamente menores en este grupo con respecto al control. No se identificaron diferencias respecto al criterio de curación ni a la vía de abordaje en ambos grupos.
ConclusiónEn nuestro estudio, la PET-TC colina demostró tasas superiores de detección que permitieron aumentar el número de pacientes candidatos a cirugía dirigida con disminución de la morbilidad quirúrgica, especialmente en grupos con adenomas de menor tamaño asociados a niveles más bajos de calcemia y PTH preoperatorias y en pacientes con cirugías cervicales previas.
Primary hyperparathyroidism (PHPT) is one of the most frequent endocrine disorders in our setting. Its incidence increases with age, and it predominantly affects middle-aged women.1 PHPT is caused by a single parathyroid adenoma in 80%–85% of cases, followed by parathyroid gland hyperplasia (10%–15%), double adenoma (4%), and, finally, parathyroid carcinoma (<1%).
Surgery is the treatment of choice in symptomatic or asymptomatic patients who meet the criteria proposed by international consensus (patients younger than 50 years, calcemia >1 mg/dL above the upper limit of normality, glomerular filtration less than 60 mL/min, osteoporosis diagnosed by hip/spine/forearm densitometry with a T index <2.5 SD, or impossibility of medical follow-up)2–6 and it is the only treatment that is considered potentially curative. In symptomatic non-operable patients, pharmaceutical block treatments are available to maintain control over the disease.
Targeted resection of the hyperfunctioning parathyroid adenoma is the technique of choice in all patients, since it has been shown to have the same efficacy as bilateral cervical exploration and is associated with a shorter operative time, lower complication rate, shorter recovery time, shorter hospital stays and, consequently, lower cost.4,7 Therefore, targeted surgery in PHPT requires preoperative imaging studies in order to detect and locate hyperfunctioning adenomas preoperatively.
Different imaging studies are available, including cervical ultrasound, computed tomography or nuclear magnetic resonance, as well as functional techniques using radiotracers, such as 99mTC-MIBI SPECT, which have allowed us to increase the detection rate of parathyroid adenoma.4,8 To date, SPECT/CT has been considered the gold standard with the highest detection rates, ranging between 84% and 88% of cases, according to different meta-analyses.4,9,10
Despite this, it is worth noting that the detection of hyperfunctioning adenoma is not possible in a percentage of patients, and intraoperative bilateral cervical examination is required. This reduced sensitivity has been classically associated with lighter adenomas as well as glandular hyperplasia (more predominant in MEN syndromes), double adenoma, or previous cervical surgery.
Recently, the role of positron emission tomography/computed tomography (PET/CT) with the use of 18F-fluorocholine has been shown to have higher detection levels of hyperfunctioning parathyroid tissue than SPECT/CT, which has increased the number of patients who are candidates for targeted interventions.11–23
This study has been designed to evaluate the sensitivity of 18F-fluorocholine PET/CT compared to MIBI SPECT/CT in the detection of hyperfunctioning adenomas, as well as to identify the existence of clinical, analytical or histological factors that may be related to a decreased sensitivity of conventional tests.
MethodsA prospective cohort study was conducted from November 2017 to May 2019.
The selected series consisted of 34 consecutive patients, all of whom were candidates for surgical treatment and had a biochemical diagnosis of PHPT of any etiology, in whom secondary causes of hyperparathyroidism had been ruled out, with negative preoperative imaging tests (scintigraphy and MIBI-SPECT/CT). Patients with a previous diagnosis of MEN syndromes were not excluded in order to study the sensitivity of choline PET/CT in these patients (classically related to the negativity of conventional tests) and to include a representative sample of patients treated in daily clinical practice. All of them underwent PET/CT with 18F-fluorocholine as a radiotracer. Cervical ultrasound was not included as an initial preoperative localization test, and it was only performed in patients in whom scintigraphy/SPECT showed concomitant thyroid disease (4 out of 34 patients) in order to complete their study to plan the operation.
After completing the preoperative localization study, the patients underwent surgery with directed excision of the hyperfunctioning adenoma detected on PET/CT. A decrease of >50% in PTH values compared to the highest pre-operative value within 10 minutes after removal was considered a criterion for cure.
In order to study the factors related with negativity in conventional preoperative localization tests (scintigraphy and SPECT/CT), a second series of 30 consecutive patients with PHPT operated on at our hospital during the same time period was used as a control group, in whom the hyperfunctioning parathyroid gland had been identified with conventional localization tests.
We collected epidemiological data for the 64 patients under study, including age, sex, baseline diagnosis, parathyroid block treatment, or previous cervical thyroid or parathyroid surgeries. Biochemical parameters were recorded at the time of diagnosis, such as calcemia, phosphatemia, and PTH levels. After surgery, both the histological pattern and gland weight were recorded, as well as postoperative biochemical parameters after 24 h and 6 months.
The preoperative localization imaging techniques used were as follows:
- •
MIBI SPECT/CT MIBI reconstruction scintigraphy: planar images were obtained 15 and 150 min after the administration of the tracer in the cervical region.
- •
PET/CT with 18F-fluorocholine: PET/CT study was performed with Gemini and Vereos equipment 60min after intravenous administration of 9.8mCi of 18F-fluorocholine.
All the data were collected in a database specially designed for this purpose and analyzed with SPSS software (V25). Since the quantitative variables did not present normal distribution, the differences between the two groups were analyzed using the Mann–Whitney U non-parametric test for independent data, and the relationship between quantitative variables was analyzed with Spearman's correlation coefficient. The categorical variables were analyzed with the chi-square test.
Results were expressed as median±interquartile range and as range for quantitative variables. Categorical variables were reported with the number of cases and the percentage. A P<.05 was considered statistically significant.
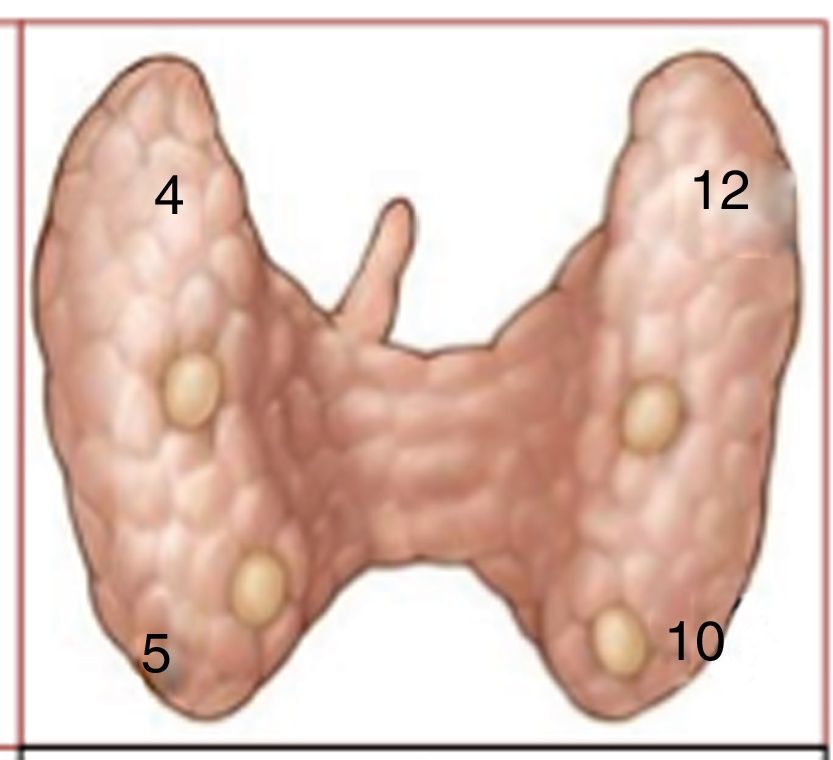
ResultsA total of 34 patients (8 men and 26 women) with a median age of 60.44±13 years (30–89) met inclusion criteria in the sample group, with negative preoperative MIBI SPECT/CT screening tests. The median age of the 30 patients collected as a control group (11 men and 19 women) was 62.97±13 years (39–83), with no observed statistically significant differences between the 2 groups in terms of sex or age (P=.25 and P=.93, respectively).
Within the group of patients with negative imaging tests, 85.3% of the patients were diagnosed with PHPT, 5.9% MEN-1, and 8.8% MEN-2. In the control group, 93.3% were diagnosed with PHPT and 6.6% with MEN-1, with no observed statistically significant differences (P=.14).
No patient in the control group had a history of previous cervical surgeries, while in the sample group 8 patients (23.5%) had a previous surgical history of parathyroidectomy or thyroid surgery; this difference is statistically significant (P=.001). The distribution between the 2 groups of patients who had received medical treatment was similar: 11 patients (32.4%) in the sample group and 5 patients in the control group (16.7%), without statistical significance (P=.144). The median time between scintigraphy/SPECT and PET/CT was 5 months.
In the sample group, the median PTH at the time of diagnosis was 15.61±9.34pmol/L, the median calcemia level was 2.64±0.20mmol/L and phosphatemia was 0.91±0.24mmol/L. In the control group, the median PTH at diagnosis was 24.88±20.47pmol/L, calcemia 2.85±0.33mmol/L, and phosphatemia 0.83±0.18mmol/L. Statistically significant differences in PTH and calcium levels were detected at diagnosis; both were significantly lower in the group of patients with negative SPECT/CT with MIBI (P=.032 for PTH and P=.004 for calcemia). No statistically significant differences were identified between the postoperative biochemical values of calcemia or PTH between the two groups after the procedure (Table 1).
Epidemiological and Clinical Characteristics of the Sample and Control Groups Pre- and Postoperative.
| Parameters Analyzed | Control Group (Positive MIBI) | Choline PET/CT (Negative MIBI/inconclusive) | P Value |
|---|---|---|---|
| Age in yrs, median (range) | 63±13 (50–76) | 60.44±13 (47.4–73.4) | .25 |
| Sex, n (%) | M: 11 (36.7)F: 19 (63.3) | M: 8 (23.5)F: 26 (76.5) | .93 |
| Preoperative location: n (%) | Eutopic: 30 (100)Ectopic: 0 | Eutopic: 31 (91.2)Ectopic: 3 (8.8) | .23 |
| Diagnostic, n (%) | PHPT: 28 (93.3)MEN-1: 2 (6.7)MEN-2: 0 (0) | PHPT: 29 (85.3)MEN-1: 2 (5.9)MEN-2: 3 (8.8) | .14 |
| Previous cervical surgery, n (%) | Yes: 0;No: 30 (100) | Yes: 8 (23.5)No: 26 (76.5) | .001 |
| Previous medical treatment, n (%) | Yes: 5 (16.7)No: 25 (83.3) | Yes: 11 (32.4)No: 23 (67.6) | .144 |
| Preoperative PTH, median (pmol/L) | 24.88±20.47 | 15.61±9.34 | .032 |
| Intraoperative baseline PTH after 10min | 4.1±2.84 | 5.89±9.36 | .256 |
| Preoperative calcemia, median (mmol/L) | 2.85±0.33 | 2.64±0.20 | .004 |
| Postoperative calcemia, median (mmol/L) | 2.35±0.19 | 2.30±0.25 | .226 |
| Preoperative phosphatemia, median (mmol/L) | 0.83±0.18 | 0.91±0.24 | .123 |
| Postoperative phosphatemia, median (mmol/L) | 0.97±0.21 | 0.98±0.28 | .428 |
| Adenoma weight, median (g) | 1.83±1.27 | 0.70±0.46 | .012 |
| Histology, n (%) | A: 26 (86.7); Hp: 4 (13.3) | A: 15 (83.3); Hp: 3 (16.7) | .599 |
A: adenoma; M: male; Hp: hyperplasia; PHPT: primary hyperparathyroidism; F: female; MEN: multiple endocrine neoplasm.
The median weight of the adenoma was lower in the patients of the sample group (0.70±0.46g) compared to the control group (1.83±1.27g), with statistically significant differences between the 2 groups (P=.012). All the glands excised as directed by the choline PET/CT findings had weights >0.06g, and all were pathological (Table 2). There were no statistically significant differences regarding the pathological anatomy between the 2 groups (control 86.7% adenoma vs. sample group 83.3%), nor for glandular hyperplasia (13.3% in the control group vs. 16.7% in the sample group; P=.599). Carcinoma was not detected in either of the groups.
Postoperative Results of the MIBI-Negative Patient Group (Sample Group) Treated Surgically.
| Patient | Sex | Age | Diagnosis | Previous Cervical Surgeries | Prior Treatment | Gland Location | Concomitant Thyroid Pathology | Time Between Tests (Months) | Thyroid Surgery | Approach | PA | Weight (g) | 6-Month Calcemia (mmol/L) | 6-Month PTH (pmol/L) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 71 | PHPT | No | No | Inferior/left | Right thyroid nodule 5mm | 6 | No | D | Adenoma | 0.15 | 2.39 | Yes | |
| 2 | F | 71 | PHPT | No | No | Sub-isthmus | Thyroid nodule, left 11mm | 4 | No | D | Adenoma | 0.22 | 2.52 | 6.29 | Yes |
| 3 | F | 79 | PHPT | No | Yes | Superior/left | No | 3 | Hemithyroidectomy left | D | Adenoma | 1.3 | 2.18 | Yes | |
| 4 | F | 67 | PHPT | Hemithyroidectomy, right | No | Superior/left | No | 2 | No | D | Adenoma | 0.32 | 2.40 | 5.48 | Yes |
| 5 | F | 89 | PHPT | No | Yes | Inferior/right | No | 72 | No | D | Adenoma | 1.05 | 2.35 | Yes | |
| 6 | M | 30 | PHPT | No | No | Superior/left | No | 3 | No | D | Adenoma | 0.67 | 2.45 | Yes | |
| 7 | M | 60 | MEN1 | Parathyroidectomy on 2 occasions | No | Inferior/left | No | 1 | No | B | Hyperplasia | 0.4 | 2.36 | Yes | |
| 8 | F | 49 | PHPT | No | No | Superior/left | Multinodular goiter | 7 | No | D | Adenoma | 0.33 | 2.45 | Yes | |
| 9 | M | 68 | PHPT | No | Yes | Superior/left | No | 1 | No | D | Adenoma | 1.33 | 2.51 | Yes | |
| 10 | F | 63 | PHPT | Directed parathyroidectomy | No | Superior/left | No | 3 | No | D | Adenoma | 0.78 | 2.42 | Yes | |
| 11 | F | 80 | PHPT | Directed parathyroidectomy | Yes | Superior/left | No | 9 | No | D | Adenoma | 0.9 | 2.53 | 67.8 | No |
| 12 | F | 74 | PHPT | No | No | Inferior/right | Left thyroid cold nodule, 2mm LTI | 1 | Hemithyroidectomy left | D | Adenoma | 0.46 | 2.45 | 3.1 | Yes |
| 13 | F | 60 | PHPT | No | No | Inferior/left | No | 4 | No | D | Adenoma | 1.27 | 2.32 | 6.52 | Yes |
| 14 | M | 69 | PHPT | No | Yes | Inferior/right | No | 13 | No | D | Adenoma | 0.3 | 2.50 | Yes | |
| 15 | F | 43 | PHPT | Directed parathyroidectomy | Yes | Double adenoma, left superior and inferior | No | 10 | No | D | Hyperplasia of both glands | 1.58/0.18 | 2.42 | 5.82 | Yes |
| 16 | F | 62 | PHPT | No | Yes | Inferior/right | Thyroid nodule, left | 10 | No | D | Adenoma | 0.78 | 2.29 | 5.95 | Yes |
| 17 | F | 68 | PHPT | Directed parathyroidectomy | No | Prevertebral C3–C4 | No | 36 | No | B | Not identified | No | |||
| 18 | F | 57 | MEN2 | Total thyroidectomy due to carcinoma | No | Inferior/left | No | 20 | No | B | Not identified | No | |||
| 19 | F | 44 | MEN1 | No | No | No detection | No | 7 | No | B | Hyperplasia | 0.4/0.2/0.3 | 2.33 | Yes | |
| 20 | M | 53 | PHPT | No | No | No detection | No | 1 | No | B | Adenoma | 0.3 | 2.33 | 6.32 | Yes |
PA: pathological anatomy; B: bilateral right; D: directed approach; M: male; PHPT: primary hyperparathyroidism; F: female; MEN: Multiple endocrine neoplasia.
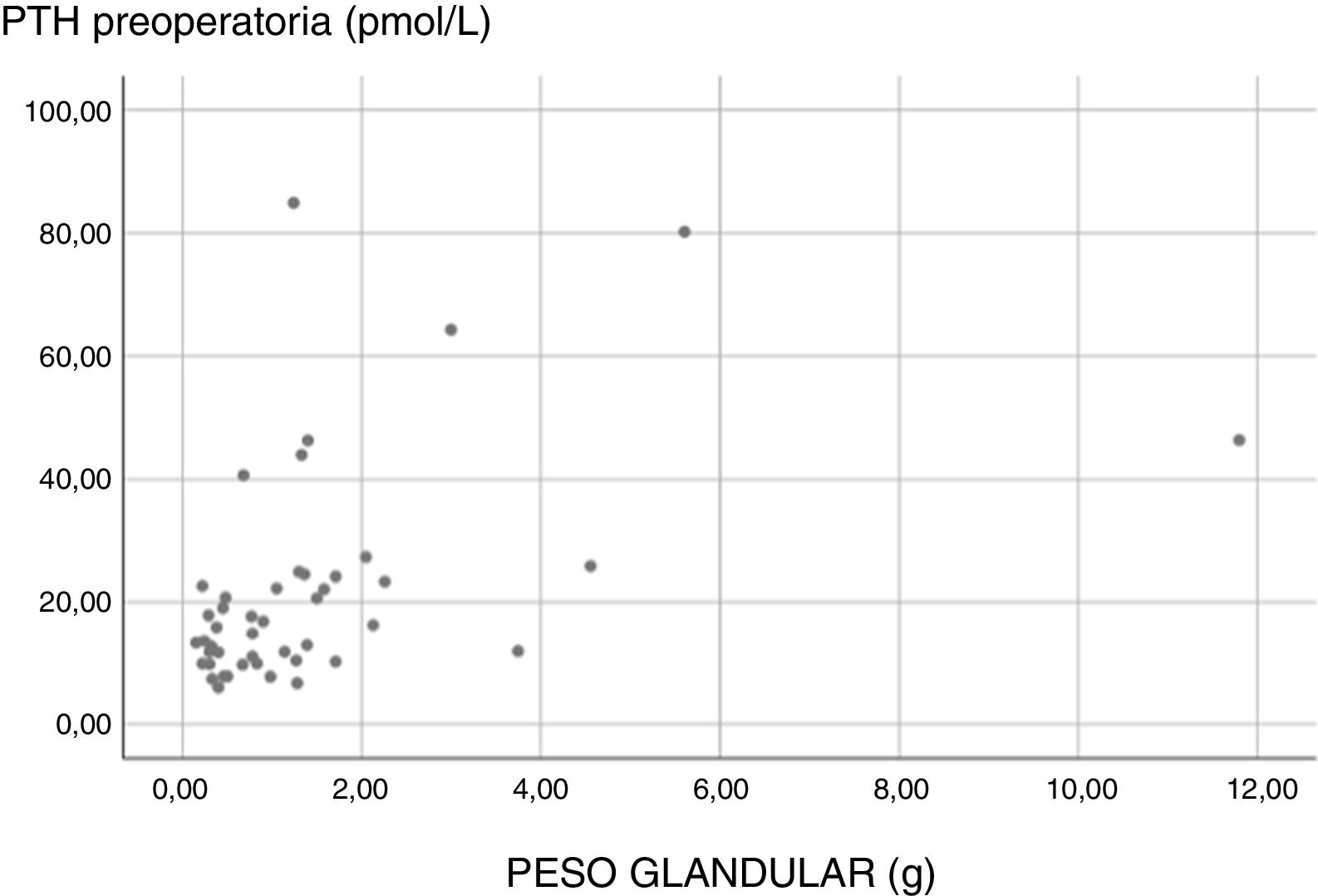
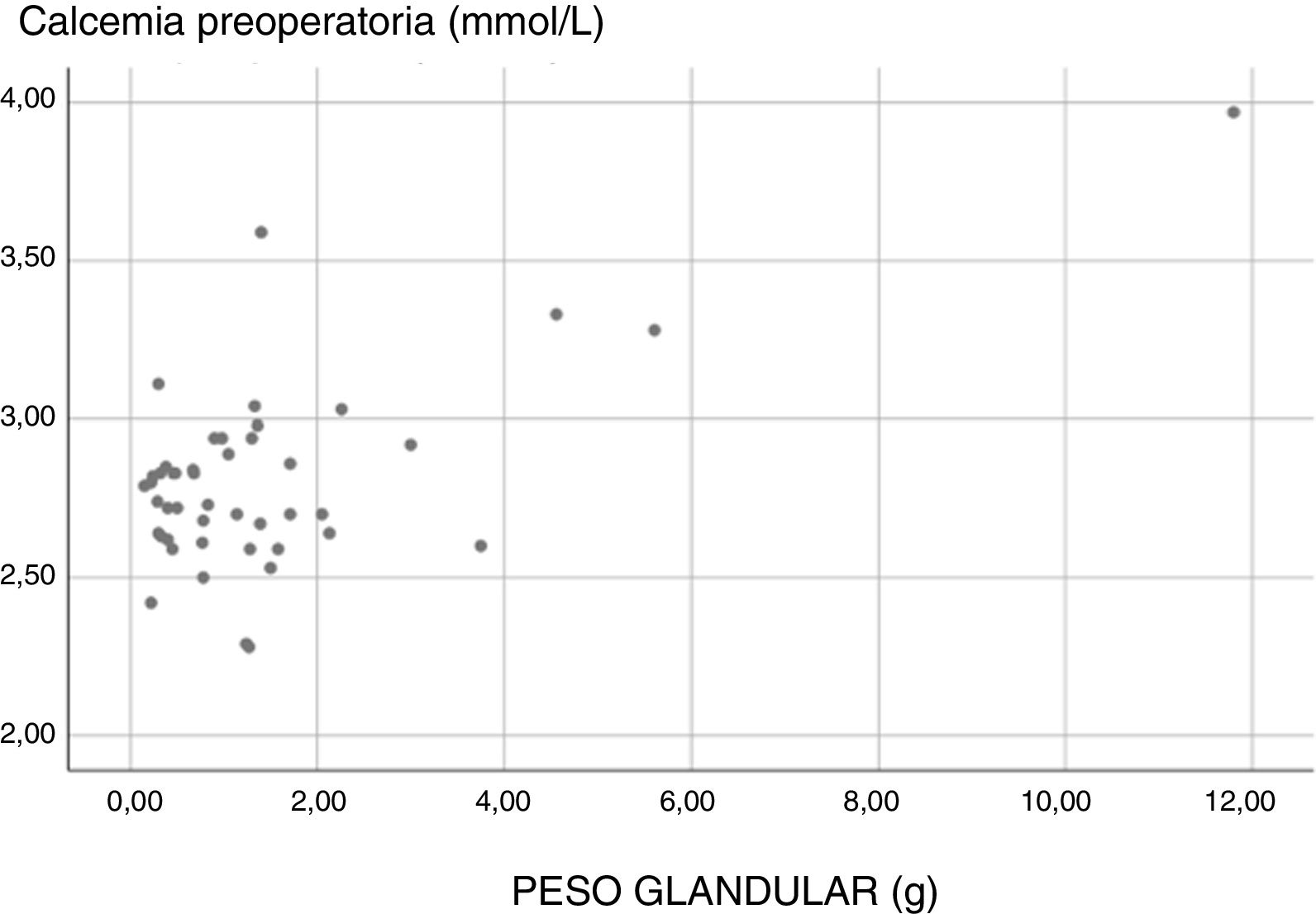
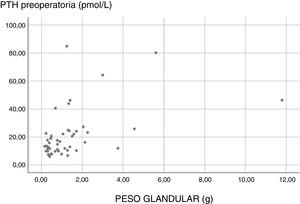
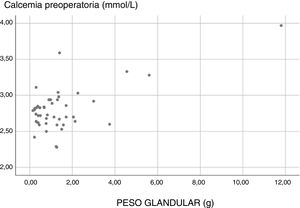
Lastly, we analyzed the correlation between gland weight and preoperative PTH and calcemia. A statistically positive relationship was only identified between glandular weight and PTH (correlation 0.493; P=.00). The correlation between calcemia and gland weight was 0.212, with a P=.157, which was not significant (Figs. 1 and 2).
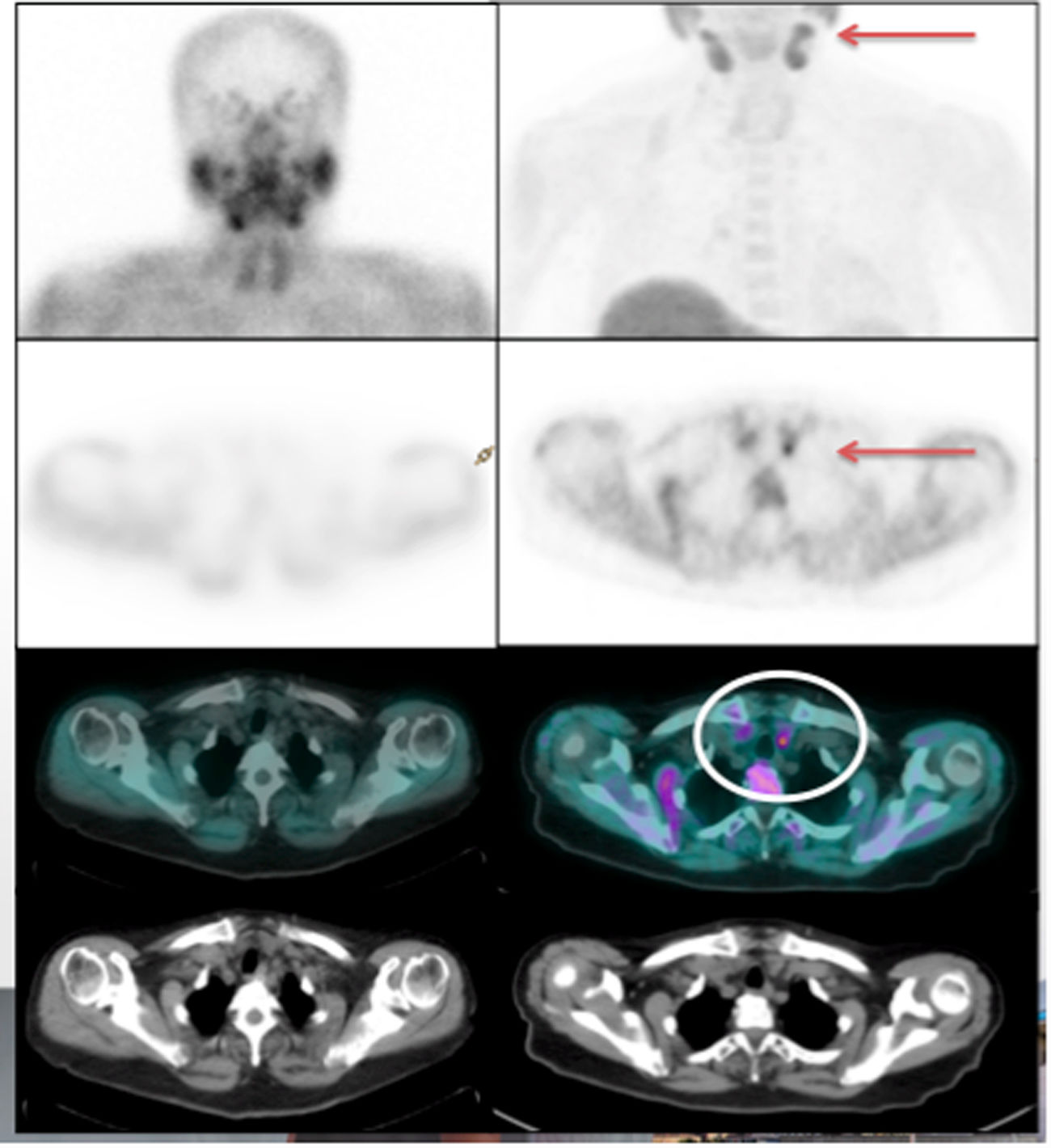
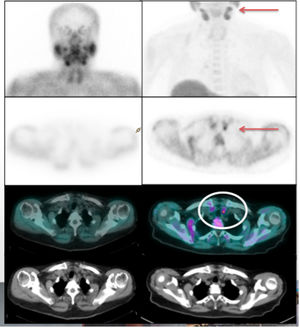
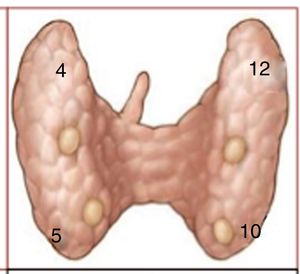
Regarding the postoperative results in the selected sample, choline PET/CT detected hyperfunctioning parathyroid tissue in 85.3% of the patients tested (29/34) (Figs. 3 and 4).
In the PET/CT choline group, 20 patients had undergone surgery at the conclusion of the preliminary study (Table 2). In 15/20 cases, a targeted approach was possible (75% of patients rescued for bilateral exploration surgery) with positive choline PET/CT, in whom intraoperative cure was achieved.
In the group of patients who required bilateral cervical exploration (5/20), one of them was a patient with 2 previous parathyroidectomies at another hospital who was diagnosed with MEN-1 and had positive choline PET/CT. Despite meeting the cure criterion after resection of the adenoma identified by choline PET/CT, given the patient's history, it was decided to perform bilateral revision. There were 2 cases of patients with a cervical surgical history with positive choline PET/CT in whom the adenoma could not be identified intraoperatively, and therefore did not meet cure criteria. Lastly, there were two other cases with negative PET/CT in whom bilateral exploration was performed. In the control group, one patient with a previous diagnosis of MEN-1 underwent bilateral cervical surgery and required subtotal parathyroidectomy due to no cure after directed excision of the adenoma identified by SPECT/CT.
In the positive choline PET/CT group, 11.1% (2/18) of the patients had demonstrated polyglandular disease: in one case previously detected by PET/CT, and in another identified during the 6-month follow-up after presenting biochemical recurrence (having presented intraoperative cure after excision directed by PET/TC). Within the control group, 6.6% (2/30) of the patients presented confirmed polyglandular disease: one of them shown intraoperatively and resolved after subtotal parathyroidectomy (MEN-1), and the other due to recurrence during follow-up, which was confirmed in the reoperation.
Among the patients with positive PET/CT 6 months after surgery, 83.33% (15/18) maintained normocalcemia in the follow-up testing. Out of the remaining 3, 2 of them were part of the group that did not reach the intraoperative cure criterion after failing to identify parathyroid glandular tissue, and the third was the patient who presented recurrence during follow-up with hypercalcemia and elevated PTH, having met the intraoperative cure criterion. The 2 patients with MIBI and negative PET/CT met the cure criterion after 6 months of follow-up. The cure rate in the control group 6 months after selective resection was 93.33% (29/30), with one case of recurrence that had shown polyglandular disease during follow-up.
DiscussionIn our study, choline PET/CT showed sensitivity rates greater than 85% in the detection of hyperfunctioning adenomas in patients with negative prior imaging tests.
With regards to the criteria classically related with scintigraphy/MIBI SPECT/CT in the literature, significant differences have been identified between the two groups: gland weight, PTH level and preoperative calcemia were significantly lower in the MIBI-negative group. PTH and preoperative calcemia presented a correlation with gland weight, which was significant in the case of PTH: lower gland weights can be related to lower preoperative PTH levels. We believe that these preliminary data could be useful in the future to determine biochemical parameters for the predictive diagnosis of negativity for scintigraphy/SPECT/CT, which could indicate the test with the highest performance in each case during biochemical diagnosis.
Among the limitations of our study, we should mention the small sample size of cases treated surgically at the conclusion date of the preliminary study. Likewise, since choline PET/CT was not performed in healthy patients, we were not able to evaluate parameters such as specificity or positive/negative predictive values. We may consider designing new studies to determine these parameters in the future, with larger sample sizes that would support the preliminary results of this study.
In conclusion, choline PET/CT is a safe, non-invasive imaging test that has shown greater sensitivity in preoperative localization studies in patients with PHPT compared to the current gold standard, MIBI SPECT/CT. This increase in sensitivity seems to be due to its ability to detect parathyroid adenomas of lower weight that present lower PTH and calcemia at diagnosis, parathyroid tissue that is hyperplastic or in an ectopic location, as well as patients with a history of previous cervical surgeries and polyglandular syndromes that show negative results in standard screening tests.
Its use would increase the rate of patients who, despite presenting negative conventional detection tests, could benefit from a targeted approach, with shorter intraoperative times, less morbidity, shorter hospital stays and lower healthcare costs.
For all these reasons, we believe that in the future choline PET/CT should be considered a valid test for preoperative detection in these patients with PHPT and that it will increase the number of patients who may benefit from targeted surgery.
Conflict of InterestsThe authors have no conflict of interests to declare.
We would like to thank Dr. Ignasi Gich for his collaboration and assistance with the statistical analysis of this article.
Please cite this article as: Ballester Vázquez E, Pérez García JI, López Mora DA, Galán Martínez C, Pareja Nieto E, Clos Enrríquez M, et al. Identificación de adenomas ocultos en hiperparatiroidismo primario con PET-TC 18F-fluorocolina. Cir Esp. 2020;98:395–402.