Bariatric surgery is presently the best option for achieving significant long-term weight loss and improving diseases associated with morbid obesity. Laparoscopic Roux-en-Y gastric bypass (LRYGB) is one of the most widely used techniques because of its excellent safety results and effectiveness in terms of weight loss and rate of complications.1 Post-LRYGB complications may appear in the short term (most frequently anastomotic leak and staple-line bleeding) or long term (internal hernias or anastomotic ulcers2). We present an extremely rare long-term complication after LRYGB: omental infarction.
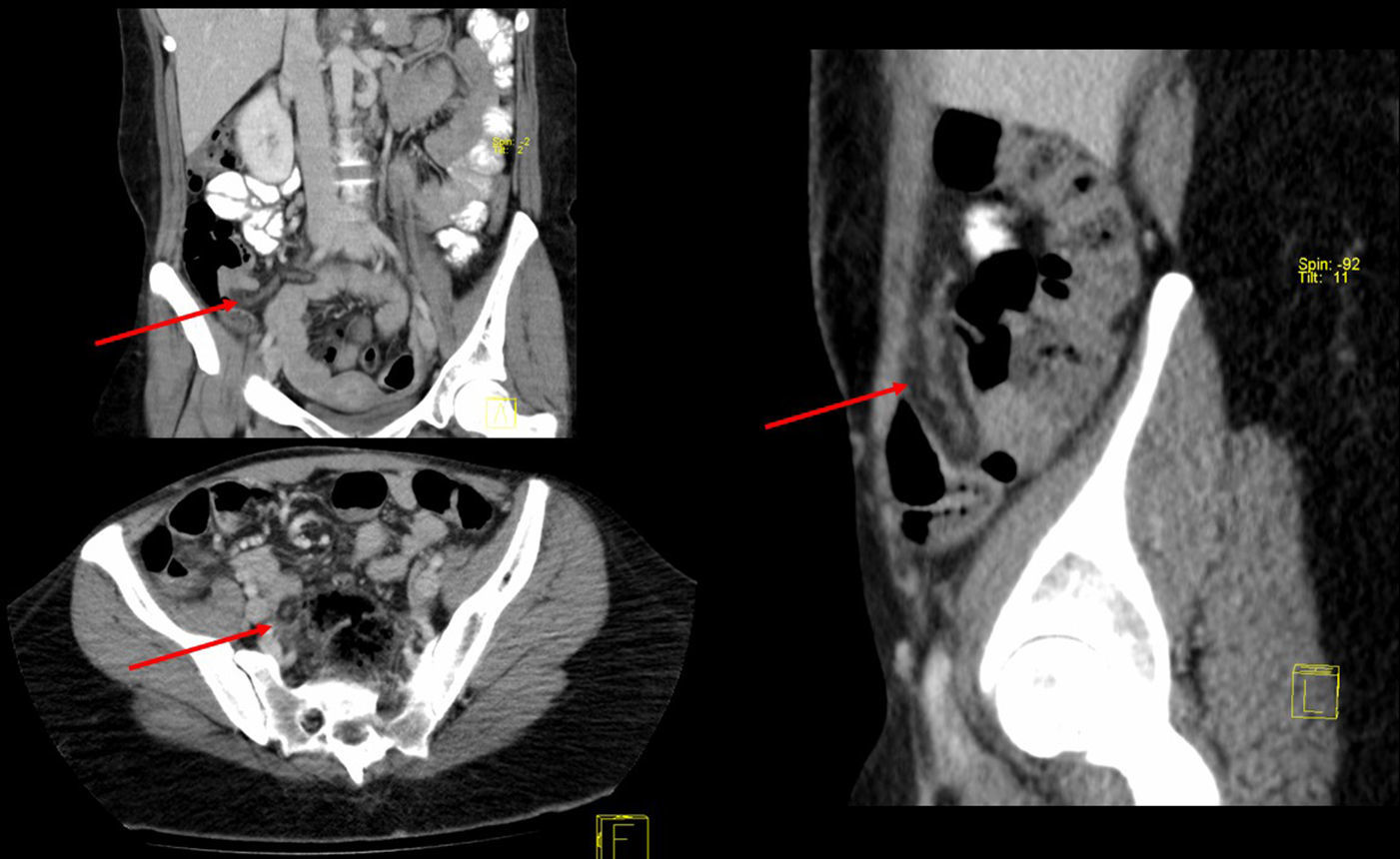
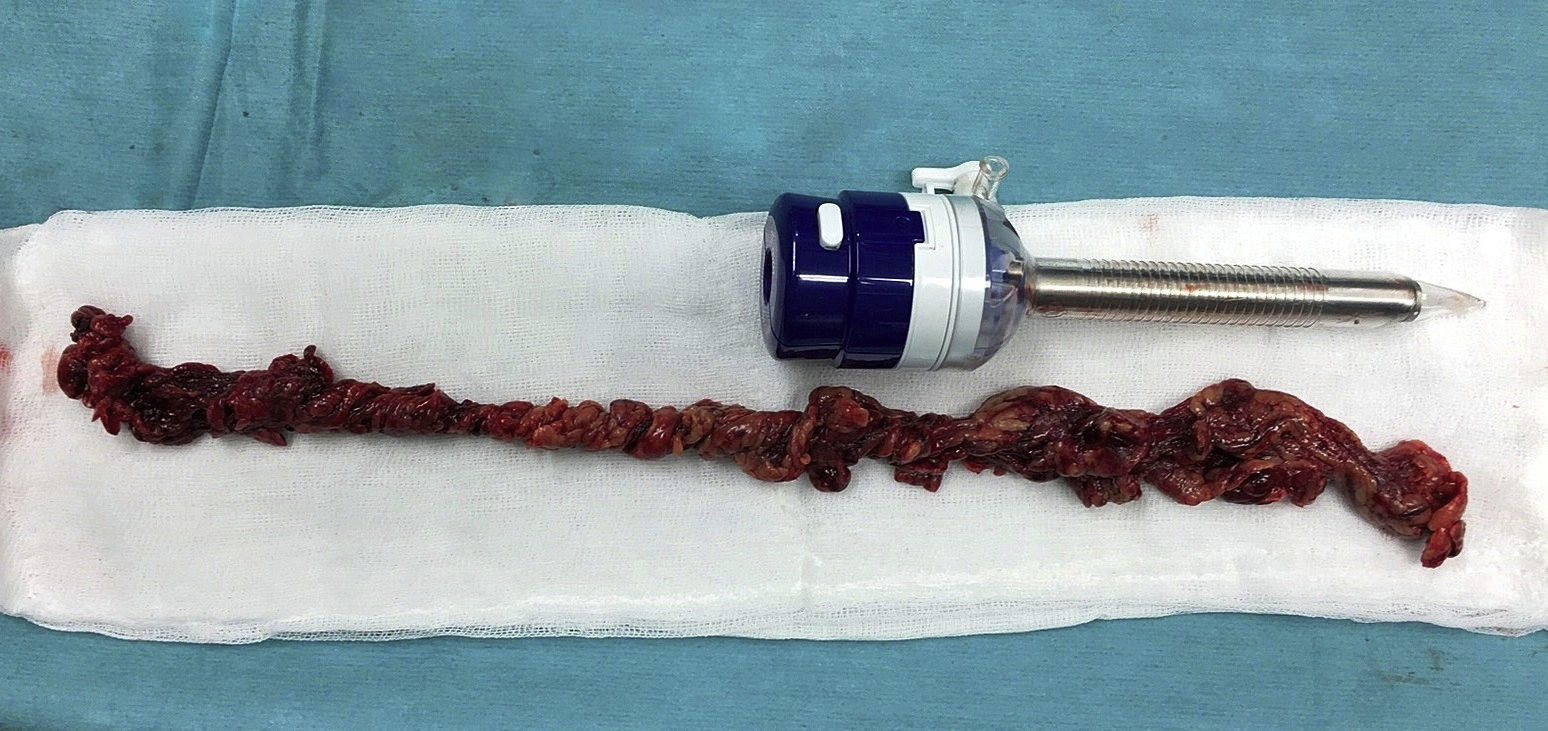
The patient is a 32-year-old woman who underwent LRYGB in 2004 due to morbid obesity (BMI 52.8) and was discharged on day 2 post-op with no complications. After surgery, the patient lost a total excess weight of 80kg. Eleven years later, the patient came to the emergency room with pain in the right iliac fossa that had been progressing over the previous 48h, with no associated fever or other symptoms. Lab work demonstrated elevated C-reactive protein levels (5.3mg/dL) and no leukocytosis. A computed tomography (CT) scan showed a tubular structure measuring some 20Ymm in diameter that was dependent on the transverse colon, compatible with inflammation of the omentum (Fig. 1). Laparoscopy revealed an omental band measuring about 40cm that was twisted and necrotized, which was resected (Fig. 2). Prophylactic appendectomy was also performed during the same surgery due to the initial suspicion of acute appendicitis, with the intention of avoiding future reoperations. After a satisfactory postoperative period, the patient was discharged.
Approximately 60% of all bariatric procedures are LRYGB.3 At our hospital, with an experience of more than 1500 interventions since the year 2000, the short-term and long-term rates of complications are 13.4% (mainly due to infection of the surgical wound) and 10.5%, respectively. However, omental infarction is a very uncommon complication: this is the first case recorded in our hospital and few cases have been published in the literature.4,5
According to the classification proposed by Leitner et al., omental infarction is defined as either primary or secondary.6 There are numerous articles and reviews published in the literature describing multiple causes, such as adhesions, tumors, internal hernias, vascular anomalies or abdominal trauma.7 In the absence of a direct cause, it is considered primary.
During LRYGB, we perform linear dissection of the greater omentum to the vicinity of the transverse colon with electrocoagulation to subsequently perform antecolic gastroenteric anastomosis. This maneuver lessens the forces of traction on the anastomosis, thereby reducing the potential risk for leaks.4 This could explain an ischemic infarction due to the asymmetric dissection of the omentum and the secondary compromise of the vascularization of a part of the omentum. However, we believe that this would explain a complication in the immediate postoperative period, as has already been reflected in the literature,4 but not 11 years after surgery, as in the case of our patient. Other predisposing factors for omental torsion have been proposed in patients with LRYGB, such as anatomical malformations or vascular abnormalities, asymmetric distribution of omental fat and adhesions or hernias caused by the surgical technique.8
The clinical manifestations are frequently limited to sudden-onset abdominal pain located in the epigastrium with no associated nausea, vomiting, anorexia, or other gastrointestinal clinical signs. Therefore, it may begin as an acute abdomen and a differential diagnosis should include other conditions, such as cholecystitis, epiploic appendagitis, sclerosing mesenteritis, gynecological disease like cystic torsion, and acute appendicitis. In addition, in patients who have undergone LRYGB, it is necessary to consider other possible long-term complications related with the technique, including internal hernia or anastomotic ulcer.
With regards to diagnosis, acute phase reactants may be normal or slightly elevated. Ultrasound may guide the diagnosis, although abdominal CT scan is the test of choice in patients with LRYGB in order to rule out other types of intra-abdominal complications. On CT, the typical sign of omental infarction is the presence of a pattern of hyperattenuating concentric strands in the fat mass, called the “whirl sign”.9
Without treatment, omental infarction may develop complications such as intraabdominal adhesions and abscesses,9 so its treatment should be surgical, including resection of the necrotic omentum. Laparoscopy continues to be the definitive diagnostic and therapeutic method for the evaluation of acute abdominal pain, especially after gastric bypass surgery. Although conservative treatment has been described in the literature, at our hospital we are not in favor of this approach because of the possible complications derived from the necrotic segment and the need for follow-up CT studies in subsequent years.10
Therefore, although torsion and infarction of the greater omentum after Roux-en-Y gastric bypass is a rare complication, it should be considered in the differential diagnosis of possible complications.
Authorship/CollaboratorsData collection: D. Ferreras.
Article composition: J. Abrisqueta y N. Ibáñez.
Critical review of the final version: J. Luján and P. Parrilla.
Please cite this article as: Abrisqueta J, Ibañez N, Luján J, Ferreras D, Parrilla P. Torsión e infarto omental: una infrecuente complicación tardía del bypass gástrico. Cir Esp. 2017;95:483–484.