Amyloidosis is a heterogeneous group of multisystem disorders, characterized by extracellular deposition of amyloid protein fibrils in organs and systems1; all show green birefringence under polarized light when stained with Congo red dye.1,2
The 2 most common types of amyloidosis are primary or immunoglobulin light chain amyloidosis and secondary or AA amyloidosis.1 The etiology of the disease is unknown and symptoms are variable.3
The finding of a pulmonary mass corresponding with an amyloid tumor is uncommon. These are isolated lesions confused with malignant masses, both radiologically and metabolically, as on PET they can be hypermetabolic.3 Surgery is diagnostic and therapeutic.2
The first case was a 60-year-old male whose medical history included surgery for a rectal neoplasm (pT3N0). During follow-up, two millimetric lesions were observed on thoracic CT: one in the right upper lobe measuring 8mm, and another in the left upper lobe (LUL) measuring 6mm, suggestive of metastases.
A PET/CT scan was performed, which determined that the nodules had a normal metabolic profile. Atypical resection of both pulmonary nodules was performed in 2 stages by video-assisted thoracoscopy. The pathology study reported nodules of amorphous material and positive Congo red, which was compatible with pulmonary amyloidoma.
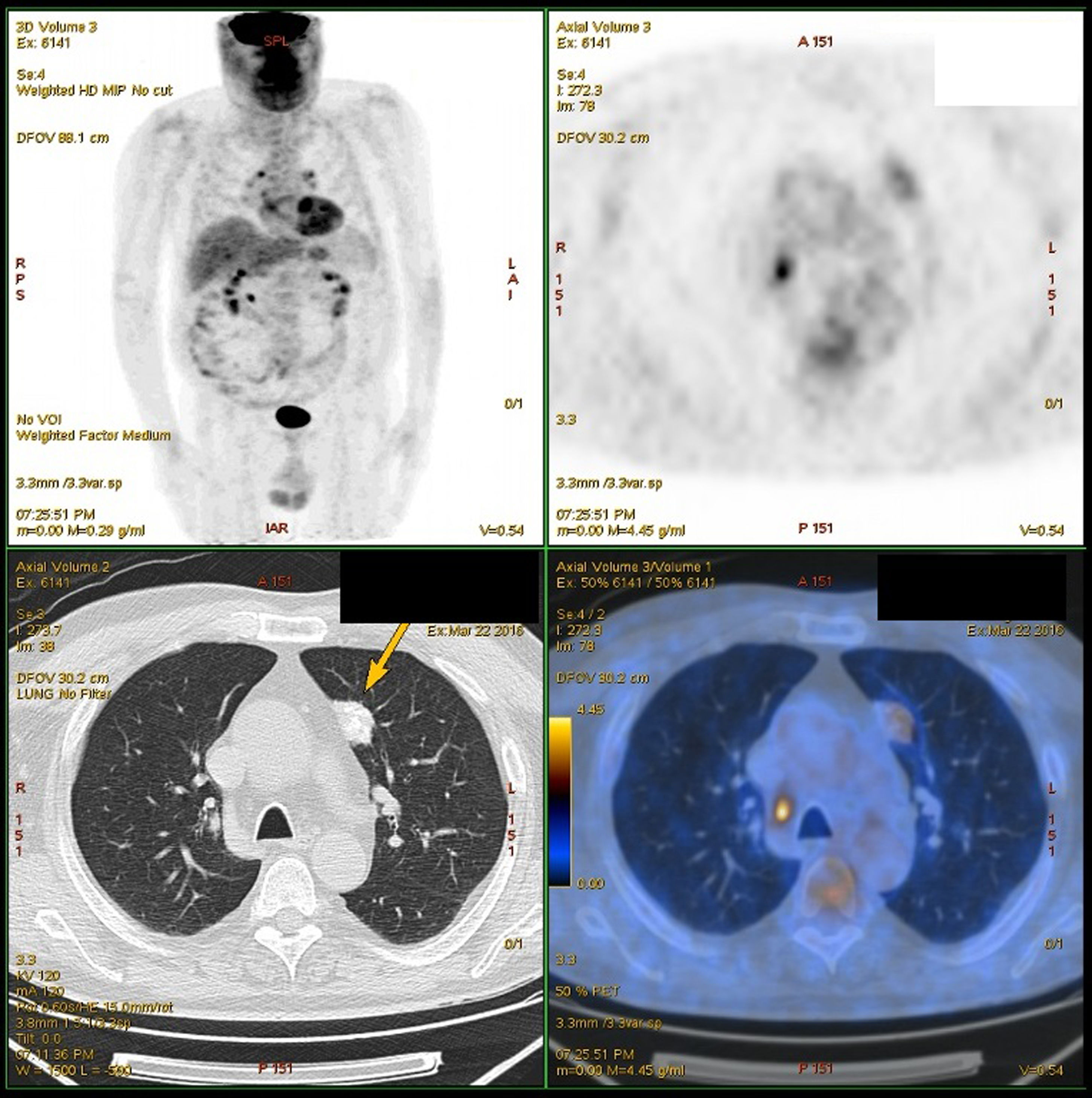
The second case was a 77-year-old male, who consulted for left thoracic pain that had been progressing for one month with pleuritic characteristics. CT scan revealed a spiculated nodule with calcifications in the apical segment of the LUL (24×21×18mm). Fiber-optic bronchoscopy and percutaneous core-needle biopsy did not provide for its identification, while the PET study (Fig. 1) showed an increase in metabolism (SUVmax 2.7g/mL). In addition, a borderline-sized lymph node that was hypermetabolic was found in the right paratracheal space (14×8mm) with SUVmax 6.3g/mL. Mediastinoscopy ruled out malignancy.
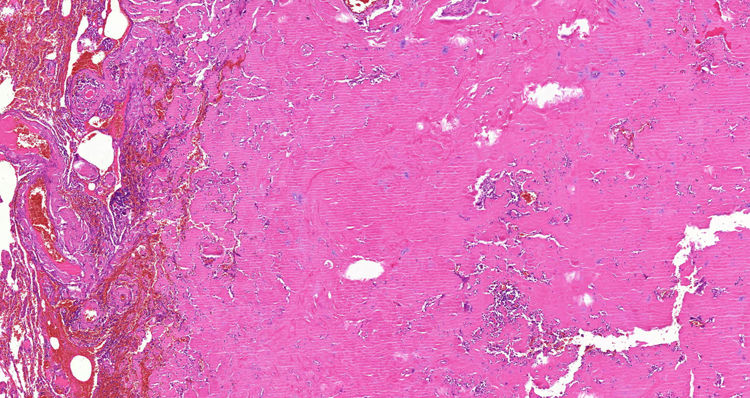
Given the suspicion of neoplasm, we performed left upper lobectomy with mediastinal lymphadenectomy by anterolateral thoracotomy. The pathology report identified an amyloid nodule that was Congo-red positive (Fig. 2).
The presentation of pulmonary amyloidosis occurs in 4 different patterns2,3: nodular, tracheobronchial, alveolar-septal and as a component of a low-grade B-cell lymphoma. The nodular and tracheobronchial types are produced by immunoglobulin light chain fragments, with no manifestations of systemic amyloidosis, and typically present as either solitary or multiple asymptomatic lung lesions. On the other hand, the alveolar-septal type is associated with systemic amyloidosis, resulting in pulmonary interstitial disease with respiratory failure and a grave prognosis.2,3 None of the patients presented systemic amyloidosis, and, due to their intraparenchymal location, they would be defined as localized pulmonary amyloidosis of the nodular type.
The results reported regarding presentation are contradictory, as some studies observed that the majority of patients presented this disease as a single nodule,4 while others described multiple lesions.3
The diagnosis of pulmonary amyloidoma is very frequently an incidental radiological finding, as in the cases described.4,5 On CT, there may be a non-pathognomonic but frequent sign, since deposits of amyloid material are associated with calcification,4 as was observed in the patient with the solitary lesion.
Regarding PET, not many cases have been published, but the existence of false positives has been demonstrated, as it is possible to find an abnormally high SUVmax in pulmonary amyloidoma,4,5 as in one of our cases. Even so, the usefulness of this test is not ruled out for 2 reasons: the rarity of the disease and the high cost-effectiveness of a non-invasive test for the diagnosis of pulmonary lesions of unknown etiology.5
Radiology-guided fine-needle aspiration biopsy of a peripheral pulmonary nodule has a high diagnostic capacity and lower risk of adverse effects than transbronchial needle aspiration.2 Provided that a lung nodule cannot be identified by the aforementioned methods, surgical biopsy is justified, as a pathology study is required2,3 as in the cases presented.
In summary, localized nodular pulmonary amyloidosis is a rare disease. However, when presented as incidental lung lesions, it is necessary to rule out a malignant etiology. Surgical biopsy is justified when a definitive diagnosis with less invasive methods is not possible.
Please cite this article as: Guasch M, Ojanguren A, Gómez JR. Amiloidosis pulmonar: un desafío diagnóstico. Cir Esp. 2020;98:50–52.