Untreated, severe, symptomatic aortic stenosis is associated with an ominous diagnosis without intervention. This study aims to determine the impact of the COVID-19 pandemic on the mortality of patients with severe stenosis during the first wave and compare it with the same period last year.
MethodsAll patients who went to the hospitals in a spanish region during the first wave, and in the same period of previous year, were analysed using Artificial Intelligence-based software, evaluating the mortality of patients with severe aortic stenosis with and without COVID-19 during the pandemic and the pre-COVID era. Mortality of the three groups were compared. Regarding cardiac surgeries was a tendency to decrease (p = .07) in patients without COVID-19 between the pandemic and the previous period was observed. A significant decrease of surgeries between patients with COVID-19 and without COVID-19 was shown.
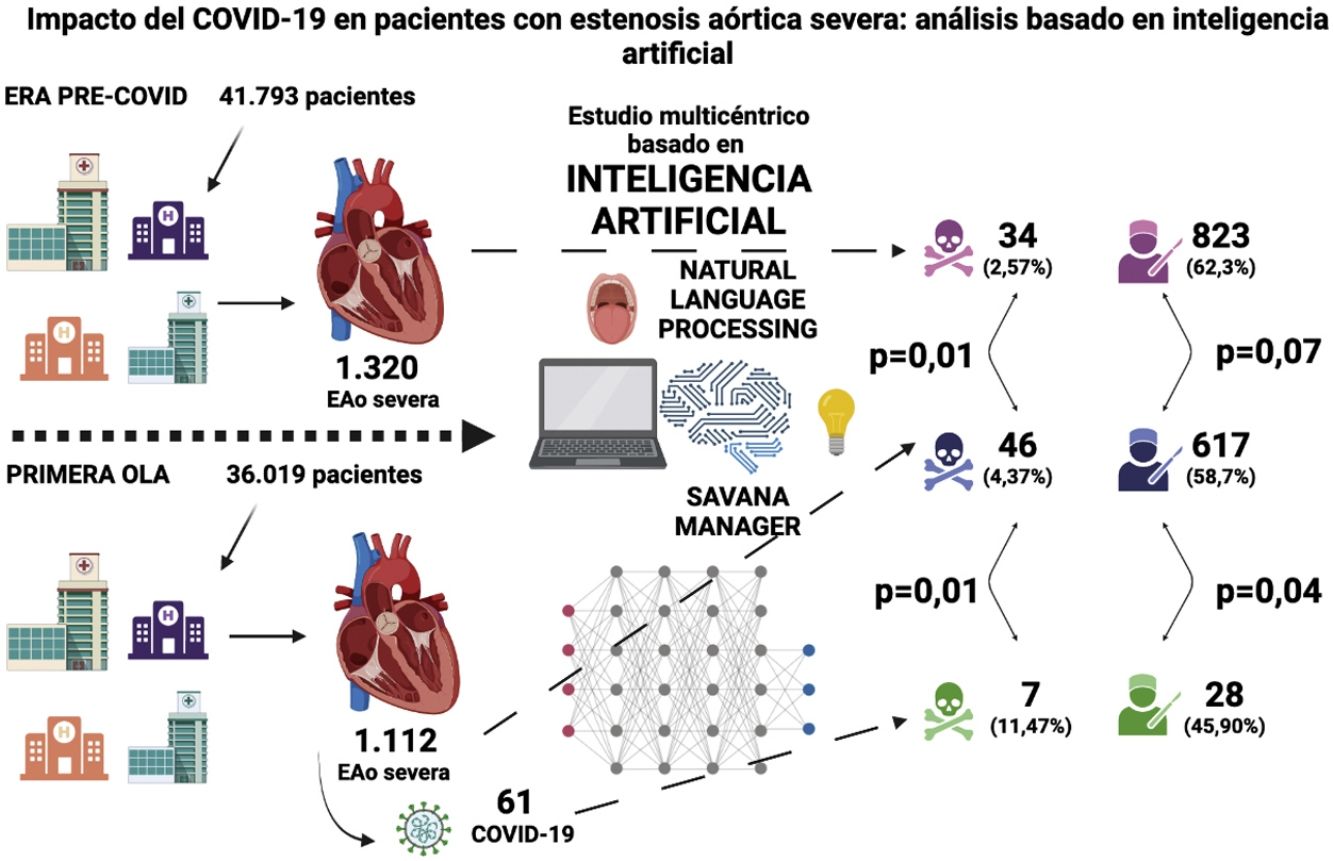
ResultsData showed 13.82% less admitted patients during the first wave. 1112 of them, had aortic stenosis and 5.48% were COVID-19 positive. Mortality was higher (p = .01), in COVID-19 negative during the pandemic (4.37%) versus those in the pre-COVID19 era (2.57%); it was also in the COVID-19 positive group (11.47%), versus covid-19 negative (4.37%) during the first wave (p = .01).
ConclusionsThe study revealed a decrease in patients who went to the hospital and an excess of mortality in patients with severe AD without infection during the first wave, compared to the same period last year; and also, in COVID-19 positive patients versus COVID-19 negative.
La estenosis aórtica severa es una enfermedad mortal en caso no ser intervenida. El estudio pretende conocer el impacto de la pandemia por COVID-19 en la mortalidad de pacientes con estenosis severa durante la primera ola y compararlo con el mismo período del año anterior.
MétodosSe analizaron mediante software basado en inteligencia artificial todos los pacientes que acudieron al hospital en una región española durante la primera ola, y en el año anterior, evaluándose la mortalidad comparada entre pacientes con estenosis aórtica severa con y sin COVID-19 durante la pandemia y la era pre-COVID. Se comparóla mortalidad en tres grupos diferentes. En cuanto al número de cirugías cardiacas, se observóuna tendencia a la baja en los pacientes sin COVID-19 con respecto al mismo período del año anterior (p = 0,07), y un descenso significativo entre pacientes COVID-19 positivo y COVID-19 negativo.
ResultadosDurante la primera ola, acudieron un 13,82% menos de pacientes totales. 1112 tenían estenosis aórtica, de los cuales, 5,48% fueron COVID-19 positivo. La mortalidad fue mayor (p = 0.01), en COVID-19 negativo durante la pandemia (4,37%) frente a los de la era pre-COVID19 (2,57%); también lo fue en el grupo COVID-19 positivo (11,47%), frente a los COVID-19 negativo (4,37%) durante la primera ola (p = 0.01). Se observó una tendencia a la disminución de cirugías (p = 0.07) en los pacientes COVID-19 negativo durante la pandemia y disminuyeron significativamente en pacientes COVID-19 positivo, frente a los COVID-19 negativo (p = 0.04).
ConclusiónEl estudio reveló una disminución de los pacientes que acudieron al hospital y un exceso de mortalidad en pacientes con EA severa sin la infección durante la primera ola, frente al mismo período del año anterior; y también, en los pacientes COVID-19 positivo, frente a los COVID-19 negativo.
Symptomatic severe aortic stenosis (AS) is a disease with high mortality if left untreated. The impact of the COVID-19 pandemic on interventions and mortality is unknown. We present the first multicentre retrospective observational multicentre study using artificial intelligence-based software (SAVANA Manager®) that analysed mortality in patients with severe AS during the first wave of the COVID-19 pandemic.
MethodsThe SAVANA Manager® software interpreted, through the use of artificial intelligence, the information collected on a large scale from any clinical report in the region (big data), using free-text multilingual reading recognition, and extrapolated the data over 2 time periods. First, we studied patients with severe AS attending hospital centres in the region of Castilla-La Mancha, Spain, during the first wave stage period from 31 January to 10 May 2020, differentiating between COVID-19 positive and negative patients, and subsequently, we compared the available data of patients with severe AS in the pre-COVID-19 era in the same time period in 2019. The time period of the study starts from the date of the first diagnosed COVID-19 patient in Spain, and includes the toughest months of the pandemic, March and April 2020.1 For data filtering, the following keywords were used: “severe aortic stenosis”, “transcatheter aortic valve implantation” and “cardiac surgery”. The software used has implemented a special technology called EHRead® for multilingual free text recognition (natural languageprocessing). In this way, it allows the free text of millions of stories to be read almost instantaneously. From this, a patient database with protected information is created, so that patients are neither traceable nor identifiable, i.e. only big data is handled. Based on the above, indexed terms that have undergone clinical validation by doctors and researchers in each field were used, so that indexed terms, as well as similar terms that have been validated, are interpreted by the software algorithm as if they were the same. For example, in the case of “severe aortic stenosis”, it would also read “severe aortic valve disease” or “severe aortic valvular heart disease” in the medical records.
Subsequent statistical analyses were performed using SPSS® software (v. 25.0). For the significance analysis, the Student's t-test was used for the comparison of numerical variables and Chi2 for qualitative variables. A significance value of p < .05 was set in all cases.
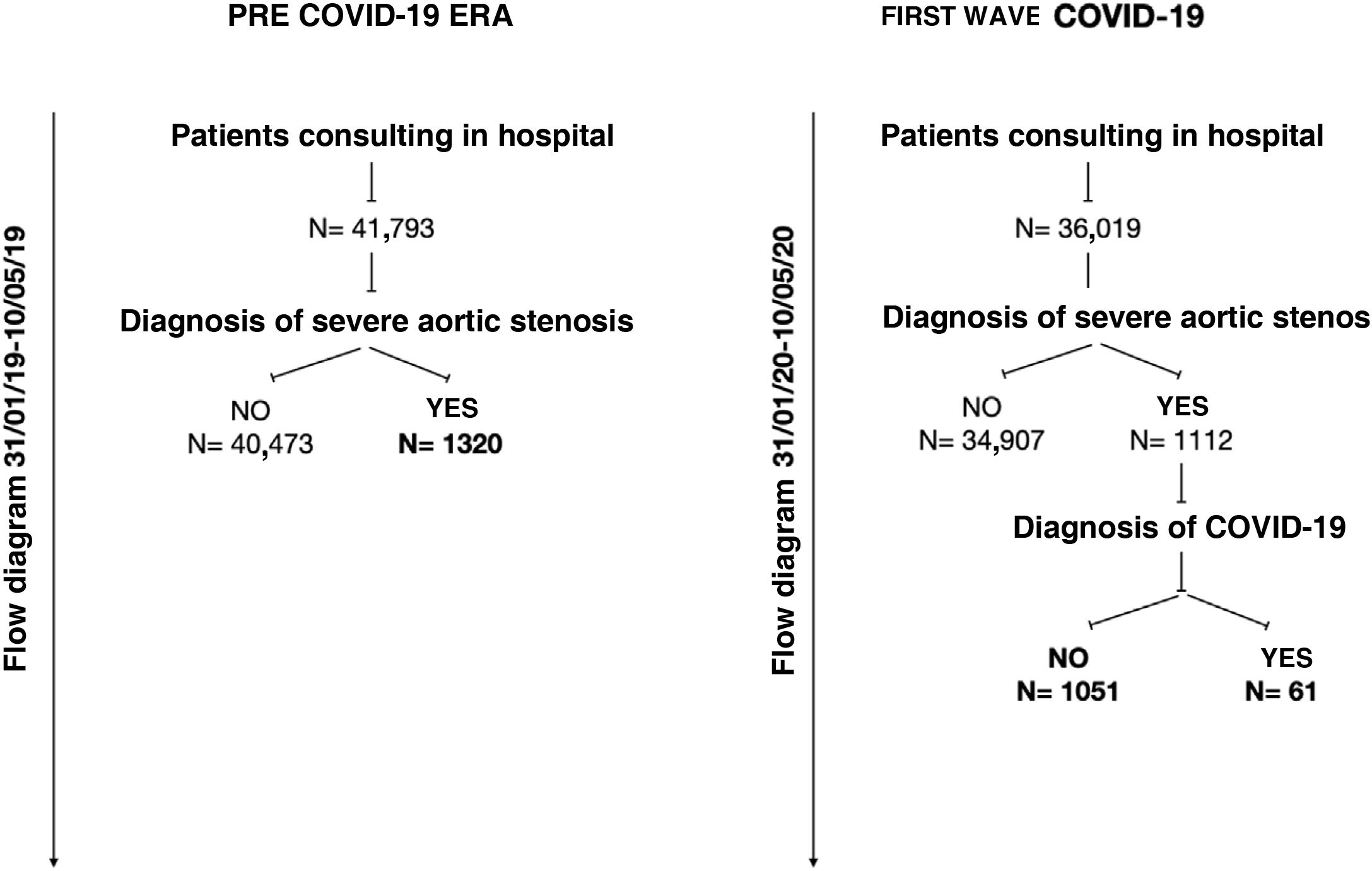
ResultsForty-one thousand, seven hundred and ninety three patients were identified who attended the hospital in the pre-COVID 19 period from 31 January to 10 May 2019, of whom 1320 had a diagnosis of severe AD. In the period 31 January to 10 May 2020, during the first wave, 13.82% fewer patients attended, 36,019; 1112 had severe AD, and of these, 61 patients (5.48%) were COVID-19 positive.
The flow diagram of the data obtained from all patients who consulted the hospital, as well as from patients with severe AS with and without COVID-19 in the referenced period of 2020 and 2019, is reflected in Fig. 1. The baseline characteristics, main symptoms of the disease, number of aortic valve interventions and mortality of the patients attending the ED are reflected in Table 1. There were no significant differences in baseline patient characteristics in any of the 3 groups, nor in cardinal symptoms, except in COVID-19 patients, where the percentage of patients with dyspnoea increased significantly (p < .01). Mortality was significantly higher (p = .01) in the group of COVID-19 negative severe AS patients who consulted during the pandemic (4.37%) compared to those who consulted in the pre-COVID-19 era (2.57%). Mortality was also significantly higher in the COVID-19 positive group (11.47%) compared to COVID-19 negative (4.37%) during the first wave (p = .01).
Baseline characteristics, interventions and mortality of patients with severe aortic stenosis attending hospital during the referral periods.
| AoS + 2019 (n = 1320) | AoS + 2020 COVID-19− (n = 1051) | p | AoS + 2020 COVID-19− (n = 1051) | AoS + 2020 COVID-19+ (n = 61) | p | |
|---|---|---|---|---|---|---|
| Age (years), median [range] | 78 [77.4−78.7] | 78 [77.3−78.7] | .98 | 78 [77.3−78.7] | 82.8 [80.5−85.1] | .09 |
| Women, n (%) | 625 (47.3) | 481 (45.77) | .44 | 481 (45.77) | 29 (47.54) | .78 |
| HBP, n (%) | 1.032 (78.4) | 832 (79.1) | .56 | 832 (79.1) | 54 (88.52) | .07 |
| DLP, n (%) | 727 (55.08) | 594 (56.2) | .48 | 594 (56.2) | 31 (50.82) | .38 |
| DM, n (%) | 520 (39.3) | 417 (39.6) | .88 | 417 (39.6) | 20 (32.7) | .28 |
| Smoker, n (%) | 34 (2.5) | 39 (3.7) | .11 | 39 (3.7) | 2 (3.2) | .86 |
| Dyspnoea, n (%) | 562 (42.5) | 457 (43.44) | .65 | 457 (43.44) | 40 (65.57) | <.01 |
| Syncope, n (%) | 153 (11.5) | 113 (10.7) | .52 | 113 (10.7) | 8 (13.1) | .56 |
| Angina, n (%) | 179 (13.5) | 142 (13.51) | .97 | 142 (13.51) | 10 (16) | .52 |
| Interventions on AoV, n (%) | 1.065 (80.65) | 820 (78) | .11 | 820 (78) | 38 (62.3) | <.01 |
| SAVR, n (%) | 823 (62.3) | 617 (58.7) | .07 | 617 (58.7) | 28 (45.90) | .04 |
| TAVI, n (%) | 220 (16.66) | 181 (17.22) | .72 | 181 (17.22) | 8 (13.11) | .40 |
| Valvuloplasty, n (%) | 22 (1.66) | 22 (2.093) | .44 | 22 (1.66) | 2 (3.27) | .53 |
| Total mortality, n (%) | 34 (2.57) | 46 (4.37) | .01 | 46 (4.37) | 7 (11.47) | .01 |
AoS: aortic stenosis; AoV: aortic valve; DLP: dyslipidaemia; DM: diabetes mellitus; HBP: high blood pressure; SAVR: surgical aortic valve replacement; TAVI: transcatheter aortic valve implantation. DATA in bold denotes where a statistically significant p value was found.
Aortic valve interventions, including surgery, transcatheter aortic valve implantation (TAVI) and valvuloplasty, did not vary significantly between the pre-COVID and COVID period in COVID-negative patients (p = .11). However, there was a downward trend in surgery (p = .07), but not in TAVI (p = .72) or valvuloplasty (p = .44), which remained more or less stable. There was a significant decrease in interventions in COVID-positive patients compared to COVID-negative patients (p < .01), mainly at the expense of a decrease in surgeries (p = .04). In this case, there was no separate significant decrease in TAVI and valvuloplasty in COVID-19 positive patients.
DiscussionThe overall decrease in the number of patients attending hospital during the first wave could be mainly due to the following 3 reasons: fear of going to hospital and becoming infected, lack of referral of patients from primary care – due to overcrowding – and the competing risk with other diseases.2 Patients with severe AS who do attend die more, probably because they arrive in a worse condition, and although this excess mortality cannot be attributed to the decrease in interventions overall, there was a trend towards a reduction in surgeries, without an increase in TAVI that could act as a compensatory element.3 Furthermore, the deterioration in the functioning of the hospital system during the first wave was evident, due to a lack of foresight and resources in the face of the enormous pressure of care. Finally, the increased mortality of COVID-19 positive patients compared to COVID-19 negative patients can be explained both by the mortality associated with infection, which has already been documented in other diseases such as infarction,4 and by the significant decrease in interventions in these patients.5–8
There are several limitations that must be taken into account when interpreting this study, such as those inherent to the methodology used, as it is a retrospective study using software that uses artificial intelligence, so there is an absence of documented information, unlike in standard studies. Also, the selection of specific terms for screening, despite the clinical validation of the software, could lead to selection bias. Nevertheless, the mortality data were reliable, and the large number of patients meant that we obtained sufficient statistical significance to draw tentative conclusions, although the potential implementation of the software may allow us to obtain more accurate results in the near future.
In conclusion, the study revealed a decrease in the number of patients consulting the hospital, as well as excess mortality in patients with severe AS in those without infection during the first wave, compared to the same period of the previous year; and also in COVID-19 positive versus COVID-19 negative patients. Further studies are needed to further investigate the causes of this excess mortality.
Conflict of interestThe authors declare that they have no conflicts of interest.