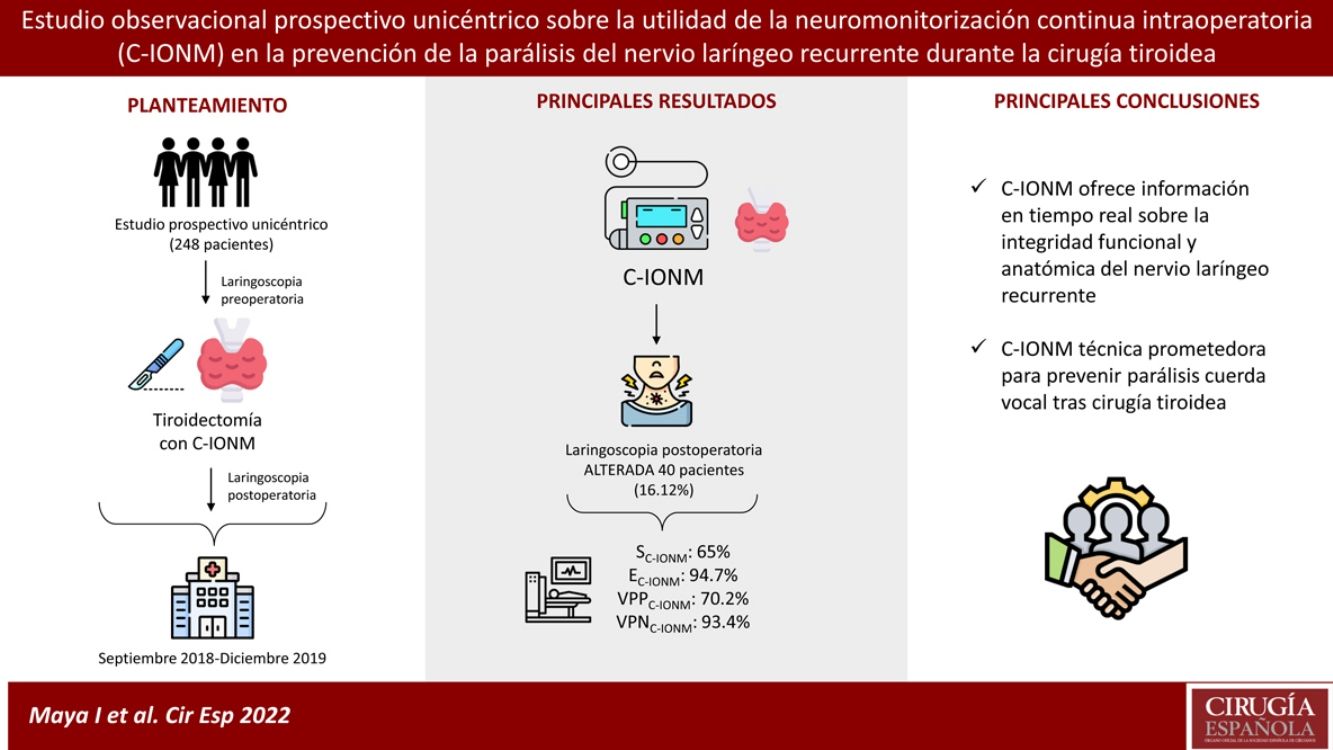
The continuous intraoperative neuromonitoring (C-IONM) of the recurrent laryngeal nerve (RLN) could help reducing the incidence of nerve paralysis after thyroid surgery, in comparison with the mere anatomical visualization of the RLN. The objective is to assess the efficacy and utility of C-IONM as a predictive test for recurrent laryngeal nerve paralysis after thyroidectomy.
MethodsA prospective observational study was performed in 248 patients who underwent thyroid surgery where C-IONM was applied, between September 2018 and December 2019, in a high-volume center. A previous and later laryngoscopy was performed, which allowed to evaluate the reliability of the C-IONM as a predictive test for recurrent paralysis. Sensitivity (SE), specificity (SP), positive predictive value (PPV), negative predictive value (NPV) were studied.
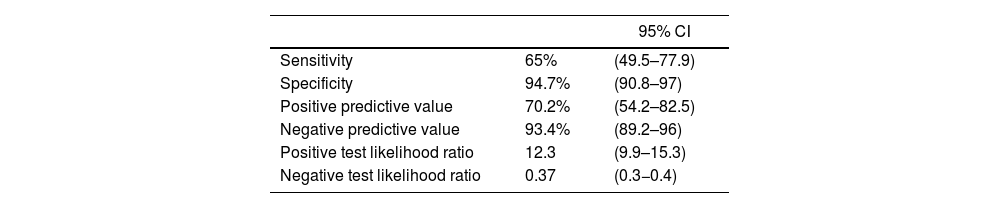
ResultsA total number of 171 thyroidectomies, 62 hemithyroidectomies, 15 totalization thyroidectomies and 27 thyroidectomy with cervical dissections were performed. Postoperative laryngoscopy was altered in 40 patients (16.12%). The SE, SP, PPV and NPV values were 65%, 94.7%, 70.2% and 93.4% respectively.
ConclusionsC-IONM is a safe technique that provides real-time information about anatomical and functional integrity of the RLN and can improve the results of thyroid surgery.
La neuromonitorización continua intraoperatoria (C-IONM) del nervio laríngeo recurrente (RLN) puede contribuir a la reducción de la incidencia de parálisis nerviosa tras una cirugía tiroidea, en comparación con la mera visualización anatómica del RLN. El objetivo de este estudio es evaluar la fiabilidad de la NCIO de los nervios laríngeos recurrentes como prueba predictora de parálisis vocal postoperatoria.
Material y métodosSe trata de un estudio observacional prospectivo realizado en 248 pacientes intervenidos de patología tiroidea en los que se aplicó la C-IONM, entre Septiembre de 2018 y Diciembre de 2019 en un único centro de alto volumen. Se realizó una laringoscopia pre y post operatoria a todos los pacientes, lo que pudo determinar la fiabilidad de la C-IONM como test predictivo de la parálisis recurrencial tras cirugía tiroidea. Se hallaron los valores de sensibilidad (SE), especificidad (SP), valor predictivo positivo (PPV) y valor predictivo negativo (NPV) de dicha técnica.
ResultadosSe realizaron un total de 171 tiroidectomías totales, 62 hemitiroidectomías, 15 tiroidectomías de totalización y 27 tiroidectomías con disección cervical. Se hallaron alteraciones en la laringoscopia postoperatoria en 40 pacientes (16,12%). Los valores de SE, SP, PPV y NPV fueron 65%, 94.7%, 70.2% y 93.4% respectivamente.
ConclusionesLa C-IONM es una técnica segura que ofrece información anatómica y funcional del NLR en tiempo real y puede contribuir a mejorar los resultados de la cirugía tiroidea.
Recurrent laryngeal nerve (RLN) paralysis is a serious complication that can significantly deteriorate the quality of life of patients after thyroid surgery.1 Routinely examination of recurrent laryngeal nerves, described in 1938 by Lahey and Hoover, is the gold standard for prevention of nerve injury during surgery.2–6 However, literature reports temporary paralysis rate between 0.4 and 12% and a permanent paralysis rate up to 5%. The most severe postoperative complication is paralysis of both RLNs, which can occur in approximately 0.5% of the cases.7
Despite the standardization of surgical procedures and systematically identification and protection of the nerve, anatomical integrity does not ensure its proper functionality. Intraoperative neuromonitoring of the RLN (IONM) in thyroid surgery helps to identify the RLN, prevent its injury and confirm its functional integrity.4,5,8–14 Continuous intraoperative neuromonitoring (C-IONM) goes a step further than IONM, since it collects real-time information and enables to anticipate the risk of RLN injury. The electromyogram (EMG) monitor alert provides enough time for the surgeon to interrupt the dissection and change the surgical strategy.8,9,15,16 However, although the use of IONM has become widespread, there is no global consensus on the role of C-IONM in the reduction of the RLN paralysis rates.12,13,15
The aim of our study is to analyze the ability of C-IONM for detecting recurrent paralysis in patients undergoing thyroid surgery.
Materials and methodsA prospective observational study was conducted in an Endocrine Surgery Unit of a high-volume center (Complejo Hospitalario de Navarra, Spain) between September 2018 and December 2019 for patients who underwent thyroid surgery. The same team of surgeons performed all the surgeries and the Institutional Review Board approved this study.
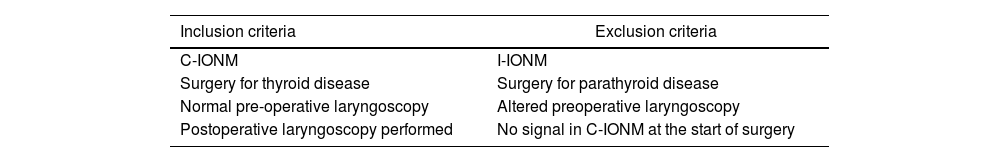
Inclusion and exclusion criteriaAll consecutive patients with thyroid disease (both benign of malignant) who underwent total thyroidectomy (with or without central and lateral cervical lymph node dissection), hemithyroidectomy or totalization thyroidectomy were included in the study. All the patients who were included had to sign an informed consent and a preoperative and postoperative laryngoscopy (1 month after surgery) to assess the vocal cords mobility were performed (Table 1). In the preoperative laryngoscopy we defined three categories: normal vocal cord, preexisting vocal cord paresia and preexisting vocal cord paralysis. Patients were excluded from the trial if there was a preexisting vocal cord injury or if they undergo parathyroid surgery.
Inclusion and exclusion criteria (C-IONM: continuous intraoperative neuromonitoring; I-IONM: intermittent intraoperative neuromonitoring).
| Inclusion criteria | Exclusion criteria |
|---|---|
| C-IONM | I-IONM |
| Surgery for thyroid disease | Surgery for parathyroid disease |
| Normal pre-operative laryngoscopy | Altered preoperative laryngoscopy |
| Postoperative laryngoscopy performed | No signal in C-IONM at the start of surgery |
Intraoperative neuromonitoring was performed using the NIM 3.0 equipment (Medtronic Xomed Inc, Florida, USA). In order to detect vocal cord activity during dissection, a Trivantage (Medtronic) endotracheal tube, containing bipolar electrodes, was placed under direct vision in close contact with vocal folds. Neuromuscular block was only used during anesthetic induction (0.6 mg/kg−1 of rocuronium) and total intravenous anesthesia was used for the surgery. Three subdermal electrodes were placed for grounding and return of stimulation.
Prior to thyroid dissection, the carotid sheath was opened in order to identify and dissect the vagus nerve. For the continuous monitoring, an automatic periodic stimulation (APS) electrode was attached to the nerve, which will conduct electrical impulses of 100 µs and 1 mA that will determine the amplitude and latency of the EMG baseline. The periodical mapping of structures was carried out using a standard monopolar probe to identify and locate the RLN (intensity 0.8 mA with a threshold of 100 µs).
Variations of the EMG baseline in terms of latency and amplitude were recorded and analyzed following the guidelines of the International Neural Monitoring Study Group.17 During surgery, the C-IONM alerts if there is a reduction in >50% of baseline amplitude or an increase of >10% of baseline latency. The complete loss of signal (PSC) implies the total absence of response after stimulation of the RLN.
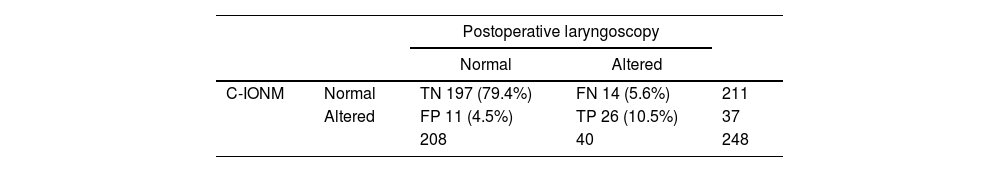
DefinitionsIn this study, both the loss and the decrease of signal (at the end of the surgery) during neuromonitoring of the RLN have been categorized as altered C-IONM, with no differentiation between the two concepts. Therefore, based on the results of the C-IONM and postoperative laryngoscopy, the following definitions were considered: True positive (TP): those patients with altered C-IONM and vocal cord paralysis in postoperative laryngoscopy; True negative (TN): C-IONM was correct during surgery and laryngoscopy was normal; False positive (FP): Altered C-IONM with normal laryngoscopy; False negative (FN): Normal C-IONM but postoperative laryngoscopy was altered.
Statistic analysisData were analyzed with IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp program. Sociodemographic and clinical characteristics of the sample were described using frequencies and percentages for qualitative variables and means with standard deviations for quantitative variables. Sensitivity (SE), specificity (SP), positive predictive value (PPV) and negative predictive value (NPV) of the C-IONM were obtained based on the postoperative laryngoscopy, with a confidence interval of 95%.
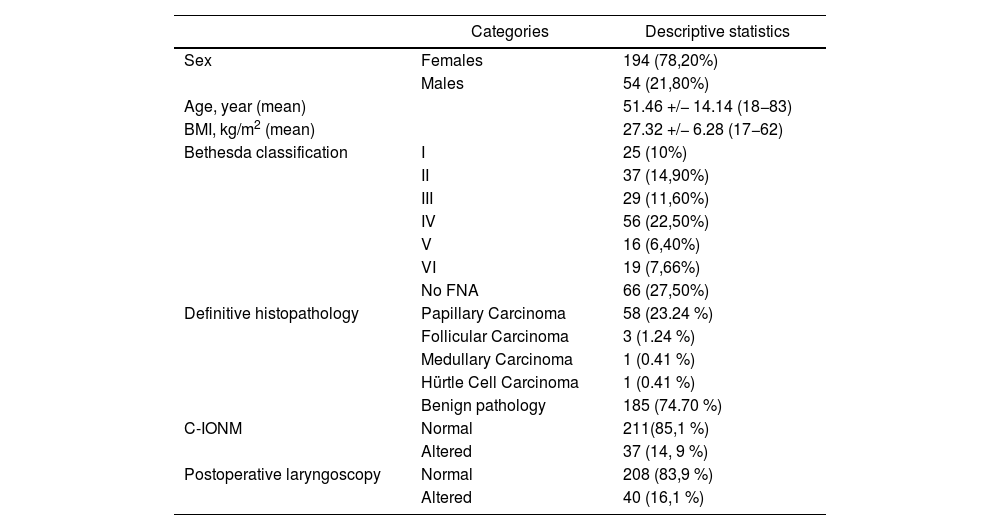
ResultsBetween September 2018 and December 2019, 384 patients underwent thyroid surgery at the Complejo Hospitalario de Navarra, of which 248 met the inclusion criteria. 78.2% of the patients were women and the range of age varies from 16 to 83 years, the average age was 51.46 years. The average BMI was 27.32 kg/m2. 36.5% of the patients had a Bethesda classification greater than or equal to IV in the FNAB (fine-needle aspiration biopsy). The demographic and clinical characteristics of the sample are presented in Table 2.
Demographic and clinical characteristics of the sample (n = 248). BMI: body mass index. FNA: fine-needle aspiration.
| Categories | Descriptive statistics | |
|---|---|---|
| Sex | Females | 194 (78,20%) |
| Males | 54 (21,80%) | |
| Age, year (mean) | 51.46 +/− 14.14 (18−83) | |
| BMI, kg/m2 (mean) | 27.32 +/− 6.28 (17−62) | |
| Bethesda classification | I | 25 (10%) |
| II | 37 (14,90%) | |
| III | 29 (11,60%) | |
| IV | 56 (22,50%) | |
| V | 16 (6,40%) | |
| VI | 19 (7,66%) | |
| No FNA | 66 (27,50%) | |
| Definitive histopathology | Papillary Carcinoma | 58 (23.24 %) |
| Follicular Carcinoma | 3 (1.24 %) | |
| Medullary Carcinoma | 1 (0.41 %) | |
| Hürtle Cell Carcinoma | 1 (0.41 %) | |
| Benign pathology | 185 (74.70 %) | |
| C-IONM | Normal | 211(85,1 %) |
| Altered | 37 (14, 9 %) | |
| Postoperative laryngoscopy | Normal | 208 (83,9 %) |
| Altered | 40 (16,1 %) |
171 total thyroidectomies (69%), 62 hemithyroidectomies (25%), and 15 totalization thyroidectomies (6%) were performed. 27 cervical lymphadenectomies (central and/or lateral) were performed for malignant pathology (10.9%).
We differentiate between temporary (16%) and permanent (2.3%) paralysis rate of the RLN. The temporary paralysis allows to recover the mobility of vocal cords in a period of one year after surgery. It is more frequent that the permanent, and it is usually caused by a neuroapraxia of the recurrent laryngeal nerve. On the contrary, permanent paralysis persists more than a year after a surgery, being detected by postoperative laryngoscopy.
We included pathologies with increased permanent neurological risk, as multinodular goiter (4.8%), Graves disease (4.2%), totalization thyroidectomy (2.7%), and total thyroidectomy associated with central lymphadenectomy (0%).
The postoperative permanent vocal fold paralysis percentage was 4.8% in hemithyroidectomies, 2.7% in totalization thyroidectomies and 0% in total thyroidectomies, and lateral or central lymphadenectomies. With a transitional hypoparathyroidism of 26.3% and permanent of 3.3%.
When comparing the C-IONM and the postoperative laryngoscopy, the TN, TP, FN, FP were obtained, and the results are shown on Table 3.
The SE and SP of the RLN C-IONM as a predictor of vocal cord paralysis were obtained. Furthermore, the PPV obtained was 70% and the NPV 93%. Confidence intervals of 95% were found in each of these values (Table 4).
Statistical results obtained from the C-IONM of the RLN based on the findings of the postoperative laryngoscopy.
| 95% CI | ||
|---|---|---|
| Sensitivity | 65% | (49.5–77.9) |
| Specificity | 94.7% | (90.8–97) |
| Positive predictive value | 70.2% | (54.2–82.5) |
| Negative predictive value | 93.4% | (89.2–96) |
| Positive test likelihood ratio | 12.3 | (9.9–15.3) |
| Negative test likelihood ratio | 0.37 | (0.3−0.4) |
The incidence of RLN paralysis during thyroid surgery described in the literature ranges between 1 and 20%.4 The majority of lesions are caused by traction (70%), electrical and thermal injury (16%) or excessive pressure on RLN (13%).6,7,10,16,18 The higher rates of accidental section or damage to the RLN occur during endothoracic goiter surgery, toxic multinodular goiters, oncologic surgery of thyroid cancer with lymphadenectomy and reinterventions.7 De la Quintana11 found that intrathoracic goitre surgery resulted in significantly more recurrent nerve injuries (p = 0.019), as it is noted by other authors.
Over the decades, the surgeon's strategy has evolved from avoiding the RLN to its routine visualization and identification. However, the anatomical identification of the nerve does not confirm its correct functional integrity.4,13,15 Recently, intraoperative neuromonitoring of the RLN has been introduced as a technique that not only helps to identify the RLN but also tries to prevent its neurological damage during thyroid surgery.8 Several studies have described its utility. Calò et al.1 compared simple nerve visualization and neuromonitoring of the RLN. They studied 2,365 patients divided in two groups and obtained a SE and PPV above 99%, with SP and PPV values also high, supporting the use of IONM. Barczyński et al. 6 obtained similar results, once again proving the superiority of IONM over the visualization of the RLN, but only in the incidence of transient paralysis and not in permanent ones. Furthermore, the German Association of Endocrine Surgeons,19 the International Neural Monitoring Study Group16 and the American Academy of Otolaryngology and Head and Neck Surgery20 recommend its use.
C-IONM’s effectiveness has been described in the literature as a safe and effective technique that allows identifying the RLN and preventing its injury during surgery. Some authors report that an amplitude decrease of >50% on the EMG baseline during C-IONM should be interpreted as a warning to change surgical strategy in order to avoid permanent injury of the RLN.9–11,20 However, the C-IONM offers different limitations: this technique can be affected by the type of anesthesia, tracheal manipulation, dislocation of the electrode of the vagus nerve and difficulty to access to it in high volume goiters. Furthermore, the C-IONM increases operative time (although it can be minimized thanks to protocols) and the surgeon must know to interpret the results and pay attention to the alarms.
Nevertheless, the superiority of the C-IONM over the I-NMIO remains controversial.9 Some studies report complications after continuous stimulation of the vagus nerve, such as cardiac arrhythmias, bronchospasm, vagal neuroapraxias, and hemodynamic alterations.2,8 In our sample, no adverse effects derived from the use of the C-IONM were recorded. A French prospective trial comparing I-IONM and C-IONM showed no significant difference when comparing one with another.21 However, Sedlmaier et al.22 compared I-IONM and C-IONM in a retrospective clinical study with 357 patients and found a statistically difference in reduction of early postoperative unilateral vocal fold paralysis (10.5% vs 4.9%) and permanent paralysis (1.5% vs 1.0%) for C-IONM. In our hospital, we use the C-IONM instead of the I-NMIO in our patients due to real-time data that allow us to detect in the EMG an initial stress of the RLN and therefore, modify our surgical technique in order to avoid nerve injury.2,3,6,8–11,20,22
Our results showed that the highest postoperative temporary vocal fold paralysis percentage was 22.6% in hemithyroidectomies, even more risky than in total thyroidectomies (20.8%) and in totalization thyroidectomies (20%). In addition to this, the postoperative permanent vocal fold paralysis percentage was higher in hemithyroidectomies (4.8%), in comparison with total thyroidectomies (0%). In view of the results, hemithyroidectomies are technically easier to realize in comparison to total thyroidectomies. One of the reasons of this result could be the fact that hemithyroidectomies are more prone to be performed by surgery residents, leading to an increase on morbidity in comparison with total thyroidectomies. Residents of surgery or low experienced surgeons start with this surgery because, even though the nerve can be equally damaged, the consequences are less serious than in a total thyroidectomy.
When comparing our results with the literature, we observed that C-IONM is a promising technique for preventing injury to the RLN23–25. De la Quintana11 reported in a prospective study carried out on a cohort of 248 patients, a SE and SP values of the C-IONM of 100% and 97.7%, respectively with a PPV of 47% compared to a 24 h postoperative laryngoscopy. We obtained a SE of 65% and a SP of 94.7% with a laryngoscopy performed 1 month after surgery. A retrospective review from UK26 used C-IONM for 27 months in a total of 256 at-risk nerves. SE and NPV for detecting postoperative vocal cord immobility were both 100%. However, the SP and PPV of this review are 85% and 18% respectively, lower values comparing with our results (94.7% and 70.2% respectively). The reason for the difference between our results and the results of the literature is certainly unknown.
The high NPV obtained (93.4%) in our study enables us to be confident about the integrity of the RLN if the C-IONM is correct. However, when C-IONM is altered it would not translate into an altered laryngoscopy. Our results show that 70 out of 100 patients in whom C-IONM was abnormal will develop some degree of vocal cord paralysis (PPV 70.2%). We obtained a global postoperative temporary vocal fold paralysis percentage of 17.8%, and a global postoperative permanent paralysis percentage of 2.3%. We compared these results with the research of Caló et al.,1 who included 1,356 patients in whom intermittent IONM was utilized (not the C-IONM), and who observed a total percentage of 0.4% permanent vocal fold paralysis and 1.7% transient vocal fold paralysis. In the same article, bilateral palsy was observed in 0.1% of the cases, requiring a tracheostomy. Florio et al.4 included 128 patients using C-IONM who were followed 6 months after surgery. Only one patient (0.8%) was found to have unilateral temporary vocal fold paralysis. In the case of Onoda et al.,9 the percentage of temporary vocal fold paralysis rose up to 14.3%, however, the research only included 43 patients. Despite the favorable results of the aforementioned articles, it is important to take into consideration that these studies were conducted with intermittent IONM instead of C-IONM, or they included a low volume of patients, making it difficult to compare them with our results.
Our study suffers the following limitations: firstly, it does not differentiate between temporary or permanent injuries, nor complex or non-complex and benign or malign pathologies. Secondly, it is an unicentric study, meaning a lower quality research than a multicentric one.
Our study shows that the high SP and NPV of C-IONM (94,7% and 93,4%, respectively) offer a guarantee regarding the absence of paralysis of the RLN when this C-IONM is normal in a high percentage of patients. We consider that C-IONM is a safe and effective technique, which improves the results of thyroid surgery. More studies are needed to support these findings and to evaluate their true effectiveness.
Author contributionAll authors have participated in the design of the paper, the data collection, analysis and interpretation as well as the writing of the article, the revision and the final approval of the version to be published.
Conflict of interestAll authors declare that they have no conflict of interest.
Funding statementThere is no source of funding.
Ethical approvalall procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consentThe institutional review board of our institute approved this prospective study, and the requirement to obtain informed consent was waived.
All authors declare no acknowledgement.