Our primary aim was to compare the long-term survivorship rates and the rates of successful osseointegration between two different types of uncemented acetabular components.
INTRODUCTION:Two types of alloys have primarily been used for the manufacture of the uncemented acetabular components: titanium-based and cobalt-based alloys. A titanium-based alloy appears to be more effective with regard to interface stress transfer to the host bone because of its lower elastic modulus relative to a cobalt-based alloy. This supposed mechanical advantage of a titanium-based alloy component motivated this comparative study.
METHODS:Two uncemented acetabular components, a porous-coated acetabulum and a Plasmacup®, were compared with a focus on long-term prosthesis survivorship and the development of acetabular osseointegration. Five radiographic signs of osseointegration were evaluated at the last follow-up appointment: (1) absence of radiolucent lines, (2) presence of a superolateral buttress, (3) medial stress-shielding, (4) radial trabeculae, and (5) an inferomedial buttress. We considered the presence of any three of these radiographic signs, in the absence of acetabular dislocation or symptoms, to be indicative of successful acetabular osseointegration.
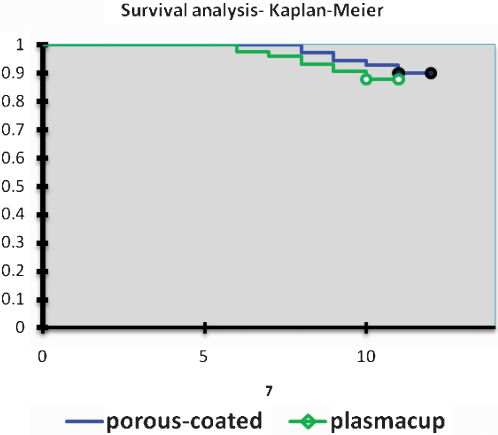
RESULTS:Among 70 patients implanted with the porous-coated acetabulum, 80% achieved osseointegration over a mean follow-up time of 11.9 years versus 75.3% of the 73 patients who received a Plasmacup insert over a mean of 10.7 years. Prosthesis survivorship rates were not different between the two groups. Revision surgery due to mild or severe acetabular osteolysis, polyethylene wear, and aseptic loosening occurred in eight patients (11.4%) with a PCA versus nine (12.3%) with a Plasmacup.
CONCLUSIONS:We conclude that, during the first ten years after surgery, there is no significant difference between these two types of uncemented cups with regard to either prosthesis survivorship or successful osseointegration.
The use of cemented acetabular components during total hip replacement procedures has yielded high ten-year post-operative failure rates.1,2 Acetabular reconstruction with human and bovine freeze-dried bone grafts and a reinforcement device has been described.3 On the other hand, the success of uncemented acetabular components is highly dependent upon the initial degree of mechanical stability and the rate and extent of subsequent osseointegration, a process that usually occurs within about three months after the procedure. Failures in either of these processes are the primary reasons for the high rates of acetabular loosening that were observed with the initial smooth-surface, non-porous acetabular designs.4-7
Two alloys have primarily been used for the manufacture of these components: one is titanium-based and the other is cobalt-based. The titanium-based alloy has been more effective in terms of interface stress transfer to host bone because of its lower elastic modulus relative to the cobalt-based alloy.8 Nevertheless, polyethylene wear and subsequent acetabular osteolysis occur with both types of acetabular components. The use of new, hard-bearing surfaces like metal-on-metal has led hip replacement surgeons to once again question the risks and advantages of cobalt-based acetabular cups.
Our primary aim was to compare the long-term survivorship rates and the rates of successful osseointegration of these two different types of uncemented acetabular components: (1) a cobalt-based alloy component with a porous-coated surface (PCA; Howmedica®) and (2) a titanium-based alloy component with a plasma spray surface (Plasmacup; Aesculap®).
METHODSWe performed a comparative retrospective study of 177 patients (34 patients were excluded) who had undergone a total hip arthroplasty (THA) for either primary or secondary osteoarthritis. All surgeries were performed by the same two surgeons in a single practice between 1997 and 1999.
The porous-coated acetabular component with a PCA femoral stem (Howmedica®) was used in 70 of the 143 patients, and the plasmacup acetabular component with two screws and a bicontact femoral stem (Aesculap®) was used in 73 patients. A 26-mm-diameter metal head was inserted in all patients in the PCA group, and a 28-mm-diameter metal head was used in all patients in the other group. A non-cross-linked polyethylene insert was used with all acetabular components. A direct lateral approach with the patient positioned in the lateral decubitus position was utilized during all procedures, and all patients received the same preventative measures against infection and deep vein thrombosis. After discharge, which generally occurred on the fifth day following surgery, the patients were assessed weekly in the outpatient orthopedics clinic for four weeks, monthly through the third month postoperatively, and annually thereafter. The patients' last evaluations were performed by a senior surgeon who had not been directly involved in the initial surgery.
From July 2008 to July 2009, we conducted a cross-sectional transverse analysis of these patients. We excluded patients who: (1) had undergone a bilateral procedure; (2) had septic loosening of the acetabular component over the observation period; (3) had cemented stems; (4) had dysplastic hip types 2, 3 and 4 in accordance with Crowe's classification9 or (5) were lost to follow-up, for any reason, prior to July 2009.
Acetabular loosening was defined as the presence of either one of the following radiographic signs: (1) any change in the acetabular abduction angle equal to or greater than 5 degrees; or (2) a vertical or horizontal displacement from the inferior or medial acetabular edges of greater than 3 mm, when considering both baselines in the anteroposterior radiographic view (Kohler's vertical line and horizontal axis; see Figure 1).10
Five radiographic signs of osseointegration were evaluated at the last follow-up appointment: (1) absence of radiolucent lines, (2) presence of a superolateral buttress, (3) medial stress-shielding, (4) radial trabeculae, and (5) an inferomedial buttress.11 We considered the presence of any three of these radiographic signs, in the absence of an acetabular dislocation or symptoms, to be indicative of successful acetabular osseointegration. With the exception of the absence of pain in the hip, only patients with a Harris hip score greater than 80 were considered asymptomatic.
We also looked for signs of acetabular osteolysis and measured linear polyethylene wear and the acetabular abduction angle. We considered good acetabular positioning to be shown by an abduction angle between 35 and 50 degrees, and we accepted up to 2 mm of polyethylene wear as 'normal’ (Figure 2).
A senior hip replacement surgeon not directly responsible for the surgeries evaluated the polyethylene linear wear based on an anteroposterior standard radiographic view of the pelvis (100 cm of distance and centered on the pubic synphisis). The difference between the thickness of the polyethylene on the radiograph and head migration was measured with a 0.1-mm ruler.
All statistical analyses were two-tailed. Continuous data demonstrating a normal distribution were evaluated by parametric tests, and comparisons between the two types of prostheses were conducted using Student's t-tests. Continuous data that did not follow a normal distribution were evaluated by non-parametric tests, such as the Mann-Whitney U test. Nominal data were summarized in 2×2 contingency tables and analyzed via a Pearson χ2 analysis or by Fisher's exact test when necessary. The a priori threshold for statistical significance was set at p = 0.05.
RESULTSSixteen patients (18.6%) from the PCA group and 18 patients (19.8%) from the Plasmacup group (p = 0.99) were excluded from further analysis; four of the 34 were excluded because of an infection followed by component loosening, and 30 were excluded because they had been lost to follow-up prior to their final 10-year follow-up evaluation.
Among the 143 subjects who remained in the study, 70 had a PCA insert, and 73 had a Plasmacup insert. No significant differences in demographic or baseline clinical data were evident between the two groups (Table 1).
The mean follow-up duration was 11.9 years (range 11.1-12.5 years) in patients who received a PCA insert versus 10.7 years (range 10.5-11.4 years) in the Plasmacup group. We observed an unacceptable abduction angle of the acetabular component in five patients (7.1%) with a PCA insert versus nine patients (12.3%) with a Plasmacup insert (p = 0.44). More than 2 mm of linear polyethylene wear was observed in 32 patients (45.7%) in the PCA group versus 38 patients (52.1%) in the Plasmacup group (p = 0.55). Acetabular components without screws (press-fit type) were used in seven and nine patients in the PCA and Plasmacup groups, respectively (p = 0.86) (Table 2).
Results.
| Parameter | “PCA group” | “Plasmacup group” | P value |
|---|---|---|---|
| Number of patients | 70 | 73 | - |
| Abduction angle (acceptable/unacceptable) | 65/5 | 64/9 | 0.44 |
| Polyethylene wear (more than 2 mm/less than 2 mm) | 32/38 | 38/35 | 0.55 |
| Press-fit cup | 7/63 | 9/64 | 0.86 |
| Osseointegration | 56/14 | 55/18 | 0.64 |
| Harris hip score (post-pre difference) | 48 | 46 | 0.74 |
Successful osseointegration without osteolysis was present in 56 patients (80%) with a PCA insert after a mean follow-up time of 11.9 years versus osseointegration in 55 patients (75.3%) in the Plasmacup group after a mean follow-up time of 10.7 years (p = 0.64).
Revision surgery due to mild or severe acetabular osteolysis, polyethylene wear, and aseptic loosening occurred in eight patients (11.4%) with a PCA versus nine (12.3%) with a Plasmacup insert (p = 0.86) (Figure 3).
In total, fifteen patients failed to exhibit radiographic evidence of acetabular osseointegration, but all remained asymptomatic through their last follow-up appointment, and none had any radiographic signs of acetabular loosening. Five patients from this group presented with signs of impending acetabular failure as suggested by head migration of more than 25% of the acetabular diameter and some degree of osteolysis.
DISCUSSIONNotwithstanding the lack of any difference between the two groups, with regard to the loss to follow-up, we believe that our drop-out rates were significant but still acceptable, considering the high mean follow-up duration. The average ages of subjects in both groups were lower than have been reported in other series.12-16 This observation might be ascribed to the higher prevalence of secondary osteoarthritis in our study, which, in turn, might be due to the study location at a public university hospital that generally serves a more disabled population. The relative youth of our sample group might also be attributed to the generally younger age distribution that exists in our country, with the majority of residents within their second to fifth decades of life.
Our acetabular revision rates were close to 12% in both groups, and there was no significant inter-group difference between rates. The acetabular revision rates reported by other authors who have used a porous-coated acetabular component vary between 3.3% and 26.5%, depending upon the duration of post-operative follow-up.12,17 This large variation might be attributed to several factors. For instance, surgeons may vary significantly in their criteria for revision surgery. Sometimes, it is difficult to identify patients who require repeat surgery if they exhibit minimal functional loss or mild to no pain in their hip. If one considers countries with a public health system, revision surgery is sometimes delayed due to high demand or other priority criteria, such as patients on the waiting list with more severe health issues being preferentially treated. This might explain the low revision rates observed in both of our patient groups; patients requiring a revision may have had to wait beyond the observational period of our study.
Patients from both groups presented with a high incidence of increased linear polyethylene wear (more than 2 mm). Several factors are associated with increased insert wear: insufficient polyethylene thickness, failure of the locking mechanism inside the metal-backed shell, and the presence of holes for supplementary screw fixation.18-20 As stated earlier, our patients tended to be younger than those in other reported studies, and younger patients are generally more active than more elderly patients. This, too, is a risk factor for increased wear. In fact, excessive activity is a behavior often observed in our patients, despite orientation and educational measures that we undertook at each annual post-operative appointment to discourage harmful activities.
Acetabular osteolysis has been described by numerous authors with incidence rates varying between 3% and 56%.17,21 It has been conjectured to be more frequent with cobalt- versus titanium-based acetabular components.22,23 However, in our comparative study, there was no significant difference between the two alloy-based prostheses.
Satisfactory acetabular osseointegration and prosthesis survivorship rates were identified in both of our surgical groups. Nonetheless, osseointegration rates of only 80% ten years after surgery prompted us to carefully observe the next ten years. In our opinion, when considering these first generation cementless acetabular cups, early conclusions about the superiority of uncemented over cemented acetabular components might be presumptuous given that longer follow-up studies have already been published for cemented acetabular cups.24 Osteolysis, especially in stable components, can be a difficult obstacle for hip surgeons to overcome, and it becomes even worse when a modularity change occurs, despite this observation in cemented acetabular sockets.
We hope that the recent development of higher quality cross-linked polyethylene components, as well as the use of alternative bearing surfaces, will improve the long-term survivorship of uncemented acetabular components by decreasing acetabular osteolysis.
We conclude that, during the first ten years after surgery, there is no significant difference between these two types of uncemented cups concerning both prosthesis survivorship and successful osseointegration.