To determine the range of motion and stability of the human cadaveric cervical spine after the implantation of a novel artificial disc and vertebra system by comparing an intact group and a fusion group.
METHODS:Biomechanical tests were conducted on 18 human cadaveric cervical specimens. The range of motion and the stability index range of motion were measured to study the function and stability of the artificial disc and vertebra system of the intact group compared with the fusion group.
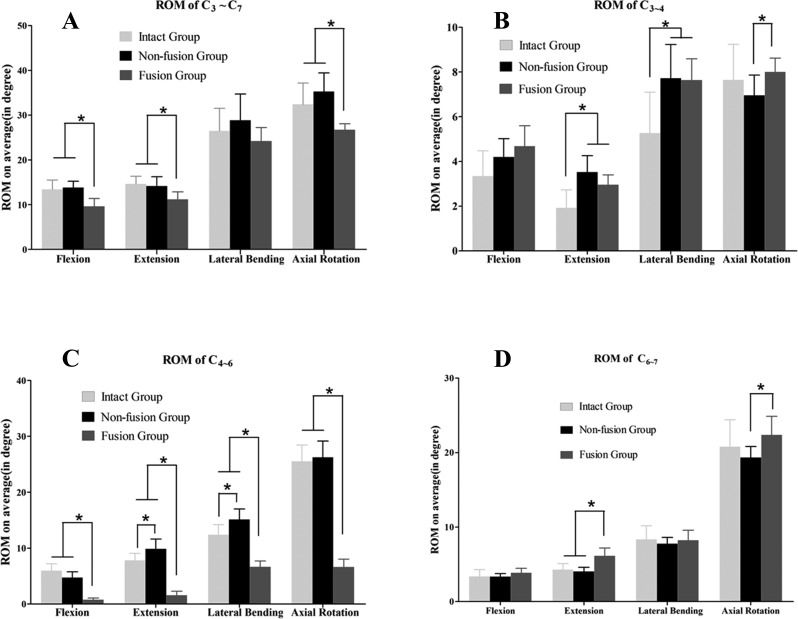
RESULTS:In all cases, the artificial disc and vertebra system maintained intervertebral motion and reestablished vertebral height at the operative level. After its implantation, there was no significant difference in the range of motion (ROM) of C3–7 in all directions in the non-fusion group compared with the intact group (p>0.05), but significant differences were detected in flexion, extension and axial rotation compared with the fusion group (p<0.05). The ROM of adjacent segments (C3−4, C6−7) of the non-fusion group decreased significantly in some directions compared with the fusion group (p<0.05). Significant differences in the C4-6 ROM in some directions were detected between the non-fusion group and the intact group. In the fusion group, the C4−6 ROM in all directions decreased significantly compared with the intact and non-fusion groups (p<0.01). The stability index ROM (SI-ROM) of some directions was negative in the non-fusion group, and a significant difference in SI-ROM was only found in the C4−6 segment of the non-fusion group compared with the fusion group.
CONCLUSION:An artificial disc and vertebra system could restore vertebral height and preserve the dynamic function of the surgical area and could theoretically reduce the risk of adjacent segment degeneration compared with the anterior fusion procedure. However, our results should be considered with caution because of the low power of the study. The use of a larger sample should be considered in future studies.
Anterior cervical fusion has been used as an effective therapy for cervical spine diseases 1,2. However, increasing attention is being paid to the incidence of adjacent segment disease (ASD) after successful fusion 3. The lost motion at the fusion level redistributes into the adjacent segments, increasing the pressure in facet joints and adjacent discs and thus leading to ASD 3–5. Previous studies of cervical artificial discs (CADs) have shown the success of that method 6; in contrast, when anterior cervical corpectomy and fusion (ACCF) is used to treat cervical spinal diseases such as spondylitis, burst fracture, vertebral tumor, and vertebral tuberculosis 7–9, it destroys both the disc and the vertebra. Most clinical experience with CAD focuses on the intervertebral disc, not the vertebra, and CAD use cannot replace ACCF. Consequently, it is necessary to develop a prosthesis that can both preserve intervertebral motion and reconstruct the vertebral height.
We have designed a novel artificial disc and vertebra system (ADVS) that replaces both the disc and the vertebra in a functional spinal unit (FSU). This system can maintain both cervical motion and vertebral height after it is implanted into the anterior defect at the C5 level. In this study, we performed biomechanical experiments to examine the ADVS's function and stability by comparing it with an intact group and a vertebral fusion group.
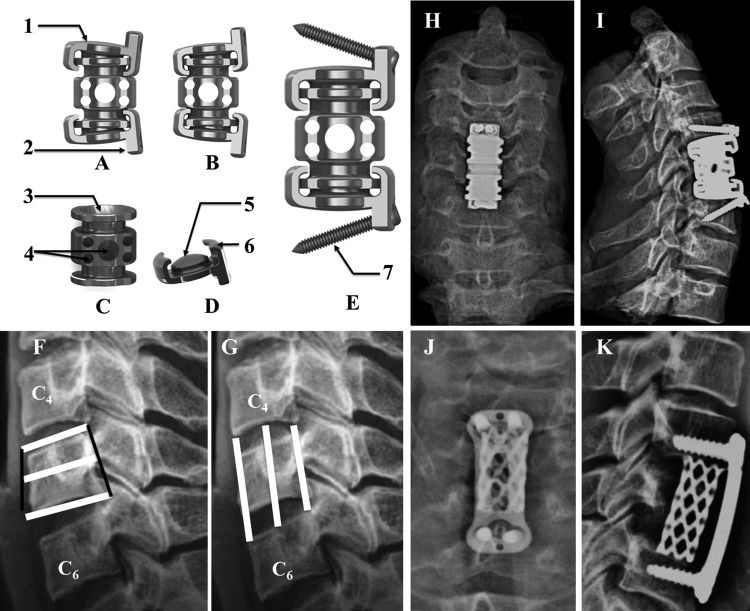
MATERIALS AND METHODSDesign of the ADVSThe ADVS prosthesis (China patent number: 201410072192.7) was designed to mimic the physiological motion of the cervical spine (Bright Laser Rapid Prototyping Technology Co., Ltd, Xi′an, China.). It was made from a titanium alloy (Ti6Al4V) and comprised three major compartments: the upper & lower artificial cervical discs and the middle artificial vertebra (Figure 1). Each disc featured a base and a front wing with a 90° angle between them. The base included an articular head and a spherical surface 8 mm in diameter and 4 mm in depth at the bottom. The front wing featured two cancellous bone screw holes one on each side. There was a unique “L” structure on each side of the disc's base that was designed to prevent the dislocation of the disc and the vertebra. The artificial vertebra had an articular fossa 8 mm in diameter and 4 mm in depth on its upper & lower sides. Several tubes of different diameters were designed for bone grafts and were included on the lateral side of the vertebra. There was a hemispherical socket joint between the disc and the vertebra that theoretically allowed a 12° range of motion (ROM) in flexion, extension and lateral bending and a 360° ROM in rotation. Rotation of the upper & lower components was achieved by allowing the hemisphere of the joint to glide in the socket with metal-on-metal articulating surfaces. The prosthesis was assembled in vitro. The disc was first fixed on the vertebra and then rotated 90° until the wing was facing anteriorly. The ADVS was fixed onto the upper and lower vertebrae using four self-drilling trapping screws. The cancellous screws were 3 mm in diameter and 16 mm to 20 mm in length.
The ADVS is made of a titanium alloy (Ti6Al4V), which has three major parts, two discs and a vertebra. There is a hemisphere socket joint between the disc and vertebra that theoretically allow 12° in flexion, extension and lateral bending, 360° in axial rotation. A) ADVS in flexion; B) ADVS in extension; C) the artificial vertebra part; D) the artificial disc part; E) the lateral view of ADVS. 1) the base part of disc, it has a smooth surface on the top that fits the adjacent vertebra; 2) the front wing part; 3) the articular fossa; 4) bone graft tubes in different diameter; 5) the articular head; 6) the “L” structure, which was designed for dislocation between the disc part and the vertebra part; 7) the self-drilling trapping screw; F) upper, middle and lower sagittal diameters of C5 vertebra; G) anterior, media and posterior height from C4∼5 disc to C5∼6 disc. The ADVS was implanted after corpectomy was performed at C5 level, X-ray films of posteroanterior view H) and lateral I) views. The anterior plate fusion performed after cervical discectomy and vertebral corpectomy of C5 level, X-ray films of posteroanterior view J) and lateral K) views.
All of the specimens were obtained via informed donation from cadaveric materials in accordance with federal and state regulations. The specimens comprised 18 sets of cervical spines with multiple levels (C2-T1; average donor age: 42.4±2.4 years; 11 male, 7 female) from the Anatomy and Pathology Department of the Medical College of Xi′an Jiaotong University. Subjective examinations confirmed the absence of skeletal abnormalities. Digital X-ray films (QDR–2000; Hologic, Waltham, MA.) were obtained to ensure that none of the specimens had osteoporosis. In our previous study, we obtained measurements of human cervical spines from 50 volunteers. The obtained parameters are shown in Figure 1. All of the specimens were stored at –20° C in double-sealed plastic bags until preparation. The muscle tissue was removed, but all ligaments and bony structures were preserved.
Biomechanical TestsBiomechanical ModelThe 18 specimens were tested as normal cervical spines (intact group), and their ROM was recorded. All of the specimens were then randomly assigned to one of 2 groups, a fusion group and a non-fusion group (ADVS implantation at C5), with 9 specimens in each group. Before testing, the specimens were thawed, and the muscle tissue was carefully removed; all ligaments, bony structures and discs were preserved. Corpectomy was performed at the C5 level using a high-speed spherical drill bit, and discectomy was performed at C4–5 and C5−6 using nucleus pulposus forceps and curettes (Figure 1). In the fusion group, a plate was fixed anteriorly from C4 to C6. To allow comparisons with the fusion group, the artificial prosthesis was implanted at the C5 level in the non-fusion group. After the screw length was measured, two superior and two inferior self-drilled trapping cancellous bone screws (3.0 mm in diameter) were fixed superoposteriorly and inferoposteriorly, respectively. The screws were inserted at a 20° angle in the cranial and caudal directions, respectively (Figure 1).
Three-Dimensional Flexibility TestAn MTS rotating machine (MTS–858/2.5, MTS System Inc., Minneapolis, MN, USA) was used for the biomechanical tests. The C3-T1 vertebrae of the test model were embedded in a special metal mould containing polymethylmethacrylate to keep the specimens in a set position with the C3 vertebra parallel to the horizontal plane. To determine the stability of the specimens, a multidirectional flexibility test was used. Our research was concerned with developing a kinematic model to establish the axes of rotation and the mutual positioning of the vertebrae with regard to flexion, extension, lateral bending and axial rotation in 4 equal steps to a maximum of 2.0 N·m 10,11. The ROM of the C3-7, C3−4, C4−6 and C6−7 segments was recorded; then, the traction arm of the MTS testing machine was stretched at a speed of 5 mm/s. A laser 3D scanning system (RealScan USB Scanner 200, 3-dimensional; Digital Corp., Danbury, CT) was used to record the under-zero load and to obtain maximum-load motion images of the cervical spine. Markers were attached to different segments of the specimen and were not in contact with each other to ensure that they could be readily distinguished. The digitized positions of the markers along the spine under different loading conditions were recorded, and the data were stored in the computer. The system then analyzed and converted the image data using the corresponding software system. Special care was taken throughout the tests to keep the specimens moist using a saline solution.
Stability Index Flexibility TestZhang et al. 11 introduced the stability index ROM (SI-ROM) to quantify the stability that instrumentation provided to the spine. The SI-ROM was defined using the following equations: SI-ROM=(ROMintact-ROMinstrumented)/ROMintact. An SI-ROM value of zero indicates that the spinal contruct is as stable as the intact spine, while a positive or negative value indicates that the spinal construct is more stable or less stable, respectively, than the intact spine.
Statistical AnalysisThe data were analyzed using SPSS software (version 19.0; SPSS Inc., Chicago, IL, USA). The results were presented as the mean±SD. GraphPad Prism 5.01 (GraphPad Software, Inc.) was used to create the histogram. The ROM and SI-ROM data were analyzed using two-tailed Student's t-tests. P-values less than 0.05 were considered statistically significant.
EthicsThis study followed the ethics guidelines of the Medical College of Xian Jiaotong University. All of the co-authors participated sufficiently in the work to assume public responsibility for appropriate portions of the content.
RESULTSThe height and sagittal diameter of the C5 vertebra and the C4−5 and C5−6 disc height were measured (Figure 1); the results are shown in Table 1. In all cases, the ADVS maintained intervertebral motion at the operative levels while reestablishing vertebral height. Figure 2 and Table 2 show the ROM of different segments of the cervical spine. Compared with the intact group, the non-fusion group showed no significant difference in the ROM of the C3-7 segment in any direction (p>0.05), and the fusion group showed significantly decreased flexion, extension and axial rotation (p<0.05; Figure 2A). The ROM of the C3−4 segment in the non-fusion and fusion groups increased significantly in extension and lateral bending compared with that of the intact group (p<0.05). Moreover, the ROM for axial rotation at the C3−4 segment differed significantly between the non-fusion and fusion groups (p<0.05; Figure 2B). The C4−6 segment ROM was compared among the groups. In the fusion group, the ROM of the C4−6 segment decreased significantly in all directions compared with that of the intact and non-fusion groups (p<0.001), and significant differences in extension and lateral bending were detected between the intact and fusion groups (Figure 2C). No significant differences in the ROM of the C−7 segment were observed between the intact and non-fusion groups. In addition, the extension and axial rotation of this segment differed significantly between the non-fusion and fusion groups, and the ROM in extension differed significantly between the fusion and intact groups (Figure 2D). Table 3 shows the SI-ROM of the non-fusion and fusion groups. At the C3-7 segment, the SI-ROM of the non-fusion group was positive in flexion and extension and negative in lateral bending and axial rotation; in contrast, the SI-ROM of the fusion group was positive in all directions. No difference was detected between the two groups at this segment. At the C3−4 segment, the SI-ROM of the non-fusion group was positive in axial rotation and negative in the other three directions; the SI-ROM of the fusion group was negative in all directions. At the C4−6 segment, the SI-ROM of the non-fusion group was negative in all directions except in axial rotation, and the SI-ROM of the fusion group was positive in all directions and was significantly increased compared with the non-fusion group (p<0.05). At the C6−7 segment, the SI-ROM of the non-fusion group was negative in flexion and positive in the other three directions, and the SI-ROM of the fusion group was negative in all directions. There was a significant difference in extension between the two groups at this segment.
C5 Vertebrae and C4−5 and C5−6 Disc Measurements (mm).
| Variable | Measured Values | x¯±s |
|---|---|---|
| Sagittal diameter of C5 vertebrae | ||
| Upper | 11.6−17.1 | 14.24±1.21 |
| Middle | 13.1−18.9 | 15.6±1.34 |
| Lower | 14.2−19.4 | 16.63±1.22 |
| Height between C4−5 and C5−6 discs | ||
| Anterior | 21.4–23.7 | 22.73±0.51 |
| Middle | 23.2–25.4 | 24.45±0.54 |
| Posterior | 18.8–20.6 | 19.98±0.58 |
ROM of C3∼C7, C3∼4, C4∼6, C6∼7. The ROM were measured under 2 N·m torque loading pressure. A) the fusion group showed a significantly restricted ROM of C3∼C7 regarding flexion, extension and axial rotation ROM of C3∼C7 compared to the intact group and non-fusion group. No significant difference of ROM in any direction was detected when compared the intact group and non-fusion group. B) the fusion group and non-fusion group showed a significantly increased ROM of C3∼4 regarding extension and lateral bending ROM of C3∼4 compared to the intact group. Significant difference of ROM of C3∼4 in axial rotation was detected when compared the intact group and non-fusion group. C) the fusion group showed a significantly restricted ROM of C4∼6 in all directions compared to the intact group and non-fusion group. Comparing with the intact group, the extension and lateral bending ROM of C4∼6 in non-fusion group increased significantly. D) the fusion group showed a significantly restricted ROM of C6∼7 in extension compared to the intact group and non-fusion group. The axial rotation ROM of C6∼7 in non-fusion group decreased significantly comparing with the fusion group. No significant difference of ROM of C6∼7 in any direction was detected when compared the intact group and non-fusion group. *p<0.05
Average Range of Motion of the Specimens in the Intact, Non-Fusion and Fusion Groups in Response to the Maximum Applied Moment of 2 N·m (in degrees).
| Motion (mean±SD) | ROM of C3−C7 | ROM of C3−4 | ROM of C4−6 | ROM of C6−7 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| INT | NF | FU | INT | NF | FU | INT | NF | FU | INT | NF | FU | |
| FLE | 13.41±2.09 | 13.84±1.40b | 9.63±1.74a | 3.34±1.13 | 4.20±0.82 | 4.68±0.92 | 5.99±1.22 | 4.72±1.04b | 0.79±0.29a | 3.39±0.90 | 3.36±0.41 | 3.88±0.58 |
| EXT | 14.66±1.69 | 14.16±2.07b | 11.21±1.68a | 1.92±0.80 | 3.52±0.73a | 2.96±0.44a | 7.83±1.22 | 9.88±1.74a b | 1.57±0.73a | 4.29±0.81 | 4.05±0.56b | 6.14±1.06a |
| LB | 26.47±5.06 | 28.87±5.85 | 24.20±3.00 | 5.27±1.83 | 7.72±1.51a | 7.64±0.95a | 12.40±1.79 | 15.12±1.9a b | 6.67±1.03a | 8.35±1.84 | 7.78±0.84 | 8.24±1.35 |
| AR | 32.40±4.78 | 35.26±4.16b | 26.75±1.30a | 7.65±1.58 | 6.95±0.91b | 8.00±0.61 | 25.51±2.91 | 26.23±2.91b | 6.63±1.39a | 20.80±3.61 | 19.34±1.47b | 22.37±2.49 |
ROM (range of motion), INT (intact), NF (non-fusion), FU (fusion), FLE (flexion), EXT (extension), LB (lateral bending), AR (axial rotation).
The values for axial rotation and lateral bending are the sums of both the right and left sides.
Stability Index of the Flexibility Test.
| Motion | Average SI-ROM of C3−7 | Average SI-ROM of C3−4 | Average SI-ROM of C4−6 | Average SI-ROM of C6−7 | ||||
|---|---|---|---|---|---|---|---|---|
| NF | FU | NF | FU | NF | FU | NF | FU | |
| FLE | 0.020±0.16 | 0.20±0.22 | −0.40±0.57 | −0.52±0.57 | 0.17±0.33a | 0.86±0.068 | −0.040±0.24 | −0.23±0.45 |
| EXT | 0.077±0.17 | 0.18±0.18 | −1.13±0.98 | −0.81±0.79 | −0.31±0.43a | 0.80±0.088 | 0.039±0.17a | −0.45±0.23 |
| LB | −0.031±0.14 | 0.0022±0.18 | −0.63±0.64 | −0.60±0.60 | −0.25±0.30a | 0.45±0.11 | 0.035±0.22 | −0.020±0.23 |
| AR | −0.0081±0.10 | 0.087±0.11 | 0.064±0.21 | −0.073±0.16 | −0.03±0.074a | 0.74±0.063 | 0.047±0.17 | −0.12±0.32 |
SI-ROM (stability index range of motion), INT (intact), NF (non-fusion), FU (fusion), FLE (flexion), EXT (extension), LB (lateral bending), AR (axial rotation).
The values for axial rotation and lateral bending are the sums of both the right and left sides.
Anterior cervical fusion has been widely used to treat cervical disc and vertebral diseases 1,2. The procedure fuses two or more cervical vertebrae and removes the disc; consequently, the dynamic function of the fusion segment is changed considerably, which can lead to long-term complications 3. For example, the loss of motion is believd to result in high pressure in adjacent discs and facet joints, and ASD has been detected after long-term follow-up 5,12. In recent years, CAD use has been proposed to replace the degenerated disc to preserve the dynamic function of the intervertebral space. Several CAD methods have yielded superior results compared with anterior cervical discectomy and fusion (ACDF) in the treatment of cervical disease 6, 12. However, in some methods, vertebral resection leads to the loss of intervertebral motion and vertebral height. Both problems can result from ACCF, and CAD use cannot reestablish vertebral height. Thus, the development of a prosthesis that could preserve intervertebral motion and reconstruct the vertebral height is necessary.
To maintain the dynamic function of the intervertebral space and reconstruct the vertebral height, we designed an artificial cervical vertebra and intervertebral complex (ACVC), and in 2012, we established a goat model to analyze the biomechanics of the prosthesis 16. Recently, other motion-preserved prostheses have been developed 17,18. However, the ball-in-trough articulation of these prostheses was the high-friction surface, and the centers of rotation of these prostheses were not in the intervertebral space. Thus, we designed a new ADVS that contained three parts: two discs and a vertebra. This new system had a larger articular surface between the disc and vertebra that confined the motion within the intervertebral space. Moreover, it had a unique L-shaped structure (Figure 1) to prevent dislocation of the two parts. The assembly processes of the system were also unique; the disc and vertebra parts were fixed at a 90° angle, and the disc part was then rotated until the wing faced anteriorly. This device allowed a 12° range of motion in flexion, extension and lateral bending and a 360° range of motion in axial rotation. Based on a cervical prosthesis classification system presented by the Cervical Spine Study Group, most cervical implants comprise metallic or polymeric components or both 19,20. Metals provide the necessary strength, ductility, and toughness required for load bearing, whereas some polymers provide low-friction surfaces for articulation and shock absorption 20. Some artificial discs, such as Prestige and CerviCore, have articulating metal-on-metal surfaces, and long-term follow-up has indicated their safety 5. Because of manufacturing limitations, we preliminary designed the ADVS using titanium alloy.
Theoretically, spinal fusion leads to a loss of motion of the fusion segment and increased motion of the adjacent upper and lower segments. In contrast, the motion of the segment is restored after ADVC implantation. In this study, we found that the non-fusion group did not show any difference in the ROM of C3−7 compared with the intact group, but it showed significant differences compared with the fusion group in all directions except lateral bending. After ADVS implantation, the ROM of C4−6 increased significantly. These results suggest that the ADVS could preserve motion in the surgical area. However, the ROM of adjacent segments (C3−4, C6−7) in the non-fusion group decreased significantly only in some directions compared with the fusion group. There are two possible explanations for this finding. First, the movement of the cervical vertebra from C3 to C7 is a coupled motion that is closely related to the facet joint 21, and the cervical ROM of each direction after ADVS implantation is unequal to that of the intact cervical spine. Because there is a 45° angle between the sagittal and horizontal planes of the facet joint, cervical lateral bending is often accompanied by axial rotation 22,2316. When the cervical spine bends to the left, for example, the lower left zygopophysis of the upper vertebra will move down along the upper left zygopophysis of the lower vertebra, shifting the right side of the upper vertebra forward. Thus, the comprehensive movement is left-axial rotation, and the spinous process moves to the right. In our study, the facet joint of the C5 vertebra was still intact after ADVS implantation; thus, the ROM of the non-fusion group could not be maintained at 12° in flexion/extension and lateral bending. Second, the instant center of rotation (ICR) should also be considered, as it has been proposed for evaluating the quality of spine movement 24. The path of the ICR during dynamic motion has been reported as moving superiorly with each successive motion segment from C2−3 to C6−724. The ADVS does not have a dynamic ICR, which contributes to the increased ROM in extension and lateral bending. The SI-ROM indicated the stability that the instrumentation to the spine 11. The motion of C4−6 was redistributed into the adjacent level because the fusion procedure causes the ROM of this area to disappear. ADVS implantation increased the ROM of lateral bending and axial rotation, resulting in a negative SI-ROM in most directions. However, no significant difference was found between the SI-ROMs of the non-fusion and fusion groups, except at C4−6. This result suggests that ADVS implantation could provide a stable biomechanical environment for the cervical spine.
The limitations of this study must be acknowledged. Although our results suggest that the ADVS preserves the dynamic function of the intervertebral space and reconstructs the vertebral height, the results should be cautiously accepted because of the study's low power. The use of larger samples should be considered in future studies. Endurance tests such as the fatigue test, the tensile test, the compression test, the shear test and the pull-out test were not performed. Titanium-on-titanium has historically been a poor bearing surface, and in vitro biomechanical testing is necessary to pre-clinically evaluate new surgical procedures and implants 25. The prosthesis has a high profile, which may cause such complications as dysphagia and esophageal perforation. We will establish an animal model to test the biomechanics of a low-profile prosthesis made of cobalt-chromium alloy and high molecular weight polyethylene (HMWPE) in future experiments.
AUTHOR CONTRIBUTIONSHe X conceived the study. Dong J, Lu M, Liang B and Xu J performed the study and the statistical analysis. Lu T, Qin J and Cai X provided the material and analysis tools. Huang S, Wang D and Li H participated in checking and analyzing the data. Dong J, Lu M, He X and Wang D participated in drafting the manuscript.
We thank Ms. Yang and her colleagues from the surgical laboratory of the Second Affiliated Hospital of Xian Jiaotong University for their help with preparing the instruments.
This work was supported by funding from the Ph.D. Programs Foundation of the Ministry of Education of China (No.: 20120201130009). No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.