Peripheral arterial disease is a severe manifestation of atherosclerosis that can lead to critical ischemia of the lower limbs and is also associated with high cardiovascular risk. Diagonal lobular and anterior tragal ear creases have been associated with coronary artery disease, but they have not yet been investigated in patients with peripheral arterial disease.
OBJECTIVES:To evaluate the prevalence of ear creases among patients with peripheral arterial disease of the lower limbs, compared with patients without documented atherosclerotic disease.
METHODS:Cross-sectional study including 60 male patients with peripheral arterial disease of the lower limbs and 60 dermatologic outpatients matched for age and gender. The associations were adjusted for other risk factors by conditional logistic regression.
RESULTS:The prevalence of diagonal and anterior tragal ear creases was higher among cases (73% vs. 25% and 80% vs. 43%, respectively) than controls; these associations remained significant even when adjusting for other known risk factors of atherosclerosis (odds ratio = 8.1 and 4.1, respectively).
CONCLUSIONS:Ear creases are independently associated with peripheral arterial disease and may be an external marker for risk identification.
Peripheral arterial disease (PAD) is a severe manifestation of atherosclerosis that may be asymptomatic or lead to critical ischemia of the lower limbs, and is also associated with increased risk of death from cardiovascular disease.1
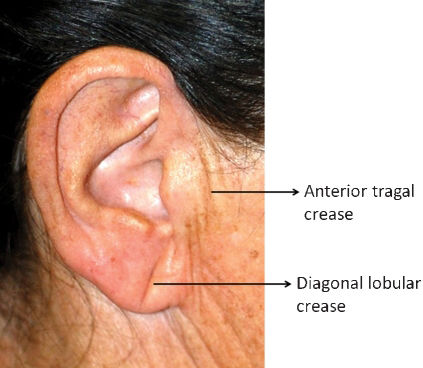
Some known risk factors for PAD include smoking, diabetes mellitus, familial history of atherosclerotic event, hypertension, and hypercholesterolemia.2 The diagonal lobular crease (DLC), described by Frank,3 and anterior tragal crease (ATC), by Miot et al.4 (Figure 1), were identified as factors independently associated with coronary artery disease,5-7 but they have not yet been studied in patients with PAD. Detection of external signs associated with PAD can assist in risk stratification and identification of patients who would benefit from early intervention or modification of risk factors related to disease progression.
We studied the prevalence of ear creases in patients with PAD of the lower limbs, in comparison with patients without documented atherosclerotic disease.
METHODSA cross-sectional study consisted of interviews with adult male patients treated at the University Hospital.
Cases were selected from claudication outpatients, with PAD of the lower limbs confirmed by arteriography. The control group was matched for gender and age and was recruited among dermatologic outpatients, who had not been revascularized (legs or ankle) or who had an ankle-brachial index not <0.9 or >1.3 (arterial noncompliance).
Patients who presented any of the following conditions were excluded from the study: immunosuppression, ear deformity, earring use or arterial obstruction due to other etiologies that could not be attributed to PAD.
The main dependent variable was the presence of PAD in the lower limbs, and the main independent variable was the presence of bilateral auricular creases. Other covariates were diabetes mellitus, previous smoking, age, familial and personal past history of atherosclerotic vascular disease (cerebral or myocardial atherosclerotic event), dyslipidemia, body mass index, and hypertension. Patients who did not know their family history were considered to have a negative history.
Categorical variables are given as frequencies and bivariately compared by the χ2 test or Fisher's exact test. Continuous variables are represented by mean and standard deviation and compared by the Student t-test. The association between variables is expressed as an odds ratio from the bivariate analysis subsequently adjusted by conditional logistic regression, comprising covariates with p<0.2.
Data were analyzed by the software SPSS 17.0. Two-tailed p values <0.05 were considered significant.
Sample size was defined according to the final multiple logistic model with α = 0.05 and power = 85%.8
This study was approved by the institutional ethics committee.
RESULTSSixty patients with PAD and 60 controls were enrolled in the study. The main clinical and demographic characteristics of patients and controls are listed in Table 1. The bivariate analysis disclosed the higher frequencies of known PAD risk factors among patients and also identified their positive association with ear creases. DLC and ATC were also more prevalent among cases than controls in all age groups (data not shown).
Main clinical and epidemiological data.
| Variables | Cases | Controls | Odds ratio¶ | p Values |
|---|---|---|---|---|
| Age, mean (SD)* | 66.0 (11.9) | 64.2 (13.4) | - | |
| BMI, mean (SD)† | 25.1 (4.0) | 24.3 (4.0) | 0,23 | |
| Familial history‡ | 21 (35) | 15 (25) | 1.6 | 0.23 |
| Myocardial infarction | 12 (20) | 3 (5) | 4.8 | 0.02 |
| Cerebral vascular accident | 10 (17) | 6 (10) | 1.8 | 0.28 |
| Diabetes mellitus | 27 (45) | 7 (12) | 6.2 | 0.00 |
| Hypertension | 49 (82) | 22 (37) | 7.7 | 0.00 |
| Dyslipidemia | 19 (32) | 10 (17) | 2.3 | 0.06 |
| Ever a smoker | 53 (88) | 40 (67) | 3.8 | 0.00 |
| DLC | 44 (73) | 15 (25) | 8.3 | 0.00 |
| ATC | 48 (80) | 26 (43) | 5.2 | 0.00 |
| DLC+ATC | 38 (63) | 8 (13) | 11.2 | 0.00 |
Results are shown as number (%) unless stated otherwise.
Significant results are shown in bold.
Multivariate analysis of the frequency of ear creases adjusted for age, diabetes mellitus, hypertension, myocardial infarction, dyslipidemia, and tobacco reinforced the association between PAD and ear creases (Table 2).
DISCUSSIONEarlobe creases were more common in male patients with PAD than in age-matched controls. These creases may represent an external sign of microangiopathic lesions in terminal circulation of the ear that occur at the same time as PAD since atherosclerosis is a systemic disease. In other series of patients, overall mortality and sudden death were significantly higher in the group with DLC.9,10 Male patients were selected to minimize the effect that earrings might have had on the ears, and because men are more affected by PAD and atherosclerosis than women. As the prevalence of both PAD and bilateral ear lobe creases increases over time, age matching was performed to normalize these risks between the groups.
Controls did not undergo arteriography for ethical and logistic reasons. The ankle-brachial index was chosen as the method to select controls owing to its high specificity (99%) and sensitivity (89%) for identification of PAD.11 Moreover, the accidental inclusion of cases among controls would have diluted the association of ear creases and atherosclerosis, rather than strengthened it.
The noninvasive identification of external findings, including DLC and ATC, digital clubbing, cyanosis, and hair loss on extremities provides information additional to epidemiological aspects such as smoking, hypertension, diabetes and dyslipidemia in raising a suspicion of atherosclerosis and risk of cardiovascular events.12
Further investigations should be performed with larger samples, heterogeneously distributed according to age, gender, ethnicity, and PAD severity, to provide a stratified risk analysis and a long-term follow up evaluation of prognostic factors in PAD.
Bilateral DLC and ATC are semiological findings which are quick and easy to evaluate and were independently associated with PAD in this population.