We performed a national survey to update hepatocellular carcinoma (HCC) epidemiology in Brazil and determined the clinical and epidemiological profiles of patients with HCC in different Brazilian regions.
METHODS:Data from 29 centers included 1,405 patients diagnosed with HCC from 2004 to 2009.
RESULTS:The median age was 59 (1–92 years old; 78% male). At diagnosis, females were older than males (median age: 62 vs. 59 years old respectively; p<0.0001). Ninety-eight percent of the patients had cirrhosis (1279/1308). Hepatitis C virus was the main etiology (54%), followed by hepatitis B virus (16%) and alcohol (14%). In Southeastern and Southern Brazil, hepatitis C virus accounted for over 55% of cases. In the Northeast and North, hepatitis C virus accounted for less than 50%, and hepatitis B virus accounted for 22–25% of cases; hepatitis B was more prevalent in the Northern than in the Southern regions. Some 43%, 35%, and 22% of patients were in early, intermediate, and advanced stages respectively. Initial therapies for HCC included chemoembolization or embolization (36%), percutaneous ablation (13%), liver resection (7%), and sorafenib (1%). Liver transplantation was performed in 242 patients (19%), but it was the initial therapy for only 56 patients (4%).
CONCLUSION:The epidemiology, classification, and therapy selection for HCC varied among Brazilian regions. Hepatitis C infection was the most common etiology of liver cirrhosis; chemoembolization was the most common therapy employed. Liver cirrhosis was the main risk factor for HCC development in Brazil.
Hepatocellular carcinoma (HCC) is one of the most common cancers in the world. It is responsible for more than 500,000 deaths/year.1 Liver cirrhosis is the major risk factor for HCC development.2 The HCC incidence is widely variable, depending on geographic region and exposure to secondary risk factors. In some regions of Asia and Africa, HCC is the major cause of death among cancers. Regions with the greatest incidence are those highly endemic for hepatitis B virus (HBV), including Sub-Saharan Africa and Southeast Asia. Among developed countries, the incidence of HCC is high in Japan and low in North America.3
In the last decade, the incidence of HCC appears to have changed in several countries. A rising incidence was observed in regions of low prevalence; for instance, in the USA.4 This change was probably associated with the rise in hepatitis C virus (HCV) as a cause of liver cirrhosis in these regions. Few data are available regarding the epidemiology of HCC in areas of low endemism. According to epidemiologic and retrospective studies, Brazil was previously considered to have a low prevalence of HCC.3 In 1997, a Brazilian survey of HCC showed that HBV was the most common cause of liver disease in patients with HCC.5 In this study, we performed a national survey in order to update HCC epidemiology in Brazil. The objective of this study was to determine the clinical and epidemiological profiles of patients with HCC in different Brazilian regions.
METHODS AND MATERIALSIn 2009, we invited members of the Brazilian Society of Hepatology (Sociedade Brasileira de Hepatologia/SBH) to complete a survey regarding patients with HCC diagnosed from January 2004 to October 2009. The questionnaire collected clinical and epidemiology data, including gender, age at HCC diagnosis, presence of cirrhosis, etiology of liver disease, and the Child–Pugh score. We also collected data on the HCC type and treatment, including the tumor characteristics (number, diameter of nodules, and presence of vascular invasion), the alpha-fetoprotein (AFP) level, and the type of HCC therapy. This study was approved by the University of Sao Paulo School of Medicine Ethics Committee, and it was conducted in accordance with the ethical principles described by the Declaration of Helsinki.
Physicians from 29 centers (19 in Southeast, 3 in Southern, 3 in Northeast, and 4 in Northern Brazil) completed the form, which provided data from 1,450 patients. Inclusion criteria were: HCC diagnosed according to the American Association for the Study of Liver Diseases (2005) criteria6 and HCC diagnosed between 2004 and 2009. Forty-five patients were excluded; one because HCC diagnosis could not be confirmed, and 44 because HCC was diagnosed prior to 2004. The remaining patients were categorized according to liver disease etiology, as follows: (1) HCV; (2) HBV; (3) HCV plus alcohol; (4) HBV plus alcohol; (5) HCV plus HBV; (6) HBV plus hepatitis Delta virus; (7) alcohol; (8) nonalcoholic fatty liver disease; (9) hemochromatosis; (10) cryptogenic; (11) other; and (12) non-cirrhotic.
The patients were also classified into three groups according to tumor characteristics (size, number, and presence of vascular invasion), as follows,: (1) early stage – one nodule with a diameter less than 50 mm or three nodules with diameters less than 30 mm and absence of vascular invasion; (2) intermediate stage – any nodule with a diameter larger than 50 mm or over three nodules and absence of vascular invasion; (3) advanced stage – presence of vascular invasion and/or extrahepatic metastasis.
Patients were also classified by the type of therapy used in the initial HCC treatment, as follows: (1) liver resection; (2) liver transplantation; (3) percutaneous ablation, including ethanol injection, or radiofrequency ablation; (4) transarterial therapies, including chemoembolization or embolization; (5) sorafenib; (6) other; and (7) none.
Different Brazilian geographic regions (Southern, Southeast, Northeast, Northern, and Mid-Western) were compared in terms of the etiology, HCC classification, and initial therapy. The Wilcoxon test was used to compare differences between age and sex. Continuous variables, such as the AFP level and tumor diameter, were divided into categories, and differences were compared using the Chi square test. A p value <0.05 was considered statistically significant.
RESULTSThe study population included 1,405 patients: 1,089 males (78%) and 314 females (22%). The median age was 59 years old (range: 1–92 years) for the entire population. On average, females were older than men at HCC diagnosis (62 vs. 59 years old), and this difference was statistically significant (p<0.0001). Cirrhosis was present in 98% of cases (1,279/1,308). The patients included in the study were from the Southeast region (77%), the Southern region (12%), the Northeast region (6%), the Northern region (4%), and the Mid-Western region (1%).
HCC etiologyHepatitis C virus was present in 716 patients (54%), and 200 of these were associated with alcohol. Hepatitis B virus was present in 206 patients (16%), and 47 of these were associated with alcohol. In 37 (3%) patients, HBV was associated with HCV (n = 30) or hepatitis Delta virus (n = 7). In 184 patients (14%), alcohol was the only etiology. In 34 patients (3%), the etiology was nonalcoholic fatty liver disease. In 10 patients (1%), the etiology was hemochromatosis. Cryptogenic cirrhosis was responsible for 41 cases of HCC (3%). Other causes were present in 51 patients (4%); these included autoimmune hepatitis, primary biliary cirrhosis, and fibrolamellar carcinoma. Table 1 shows the clinical and epidemiological data for 1,405 patients.
Clinical and epidemiological data from 1,405 HCC patients.
| Variable | ||
|---|---|---|
| Gender (n, %) | ||
| Male | 1,066 | 78 |
| Female | 297 | 22 |
| Age (median, SD) | ||
| Male | 59 | 11 |
| Female | 62 | 12 |
| Etiology (n, %) | ||
| HCV | 516 | 39 |
| HCV + alcohol | 200 | 15 |
| HBV | 159 | 12 |
| HBV + alcohol | 47 | 4 |
| HCV + HBV | 30 | 2 |
| HBV + hepatitis Delta virus | 17 | 1 |
| Alcohol | 184 | 14 |
| Nonalcoholic steatohepatitis | 34 | 3 |
| Hemochromatosis | 10 | 1 |
| Cryptogenic | 41 | 3 |
| Others | 51 | 4 |
| Noncirrhotic | 29 | 2 |
In the Southeast and Southern regions, HCV was the main etiology of liver disease, accounting for more than 55% of cases. In the Northeast and Northern regions, HCV was the main etiology, but it was present in less than 50% of cases; HBV was the next most common etiology, and the proportion (22–25%) was higher than in the Southern and Southeast regions. In the Mid-Western region, HBV was the most common etiology (40%), followed by HCV (30%) (Figure 1). The difference in liver disease distribution among different Brazilian regions was statistically significant (p<0.0001).
Liver functionData regarding liver function evaluations were available for 1,206 patients. Patients were classified as Child–Pugh A (n = 642, 53%), Child–Pugh B (n = 404, 34%), and Child–Pugh C (n = 160, 13%). Data regarding the presence of portal hypertension were available for 542 patients, and it was present in 77% of those cases.
HCC diagnosisData on the HCC diagnosis were available for 1,229 patients. Most patients (n = 779, 63%) were diagnosed based on imaging examinations. In 556 patients, only one imaging examination was necessary, either computed tomography or magnetic resonance imaging. In 223 patients, two imaging examinations were necessary. In 273 cases (22%), HCC was diagnosed based on the elevation of AFP (>200 ng/mL) associated with a liver mass in one imaging examination. In 177 patients (15%), histology was performed on biopsies; this included 21 cases that were diagnosed incidentally based on lesions in the explanted liver.
Tumor characteristicsThe number of HCC nodules was evaluated in 1,227 patients. One nodule was found in 651 patients (53%), two nodules in 201 (16%), three nodules in 96 (8%), and more than three nodules in 279 (23%) patients. The median tumor diameter was 40 mm (SD±34 mm). Macrovascular invasion was present in 231/1,090 (21%) patients. Most patients (n = 658/1,157) had AFP levels below 100 ng/mL. The AFP level was associated with tumor size (p<0.0001). The AFP was ≤100 ng/mL in 70% of patients with an HCC tumor smaller than 30 mm. On the other hand, the AFP was >100 ng/mL in over 60% of patients with an HCC tumor >50 mm.
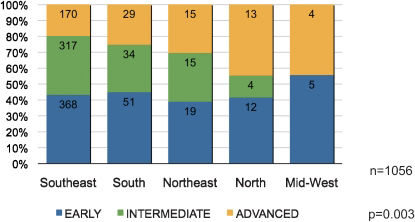
According to the tumor characteristics (size, number of nodules, and vascular invasion), HCC classification was possible in 1,056 patients. Classifications of early, intermediate, and advanced stages were made in 43%, 35%, and 22% of patients respectively. In all regions, the majority of HCC cases were in the early stage (40–55%). In the Southeast and Southern regions, intermediate HCC cases were more common than advanced cases, but in the Northern region, advanced cases were more frequently diagnosed than intermediate cases. There was a statistically significant difference in the distribution of tumor staging between different geographic regions (p = 0.003) (Figure 2).
HCC treatmentThe transarterial procedures, chemoembolization and embolization, were the most common type of initial HCC therapy (n = 456, 36%); percutaneous ablations, including ethanol injection and radiofrequency ablation, were performed in 165 patients (13%); liver resection was the preferred therapy in 87 patients (7%); sorafenib was prescribed for 17 patients (1%); liver transplantation was performed in 242 patients (19%), but it was the initial therapy in only 56 patients (4%). Figure 3 shows the distribution of patients according to the initial HCC therapy and Brazilian region.
Figure 4 shows the distribution of patients according to HCC classification and therapy. Patients in the early stage of HCC predominated in the group that received potentially curative therapies, such as liver resection, liver transplant, and percutaneous ablation. However, an important proportion of patients classified in the intermediate stage (n = 25, 33%) received liver resections. Of the 481 (37%) patients who did not receive any therapy, most had an advanced tumor and/or Child–Pugh C-grade cirrhosis (55%). Some patients were awaiting HCC therapy when the questionnaire was completed.
DISCUSSIONThis study presented the largest series of patients with HCC studied in Brazil to date. Compared with a national survey published in 1997,5 this survey indicated a greater proportion of patients with liver cirrhosis and that HCV was the main etiology. We also found differences in the prevalence of HCC etiologies and in HCC classifications among different geographic regions. In the Southern and Southeast regions, HCV and HBV were responsible for nearly 60% and less than 20% of HCC cases respectively. In the Northern and Northeast regions, HCV and HBV were responsible for less than 50% and more than 20% of HCC in cases respectively. In the Mid-Western region, only 10 cases were included, but HBV was the main cause of HCC. This different distribution of HCC etiology probably reflected the differences in HBV prevalence in Brazil. Previous studies found that the Northern and Mid-Western regions had the highest prevalence of the HBV surface antigen in Brazil.7,8
This study was not designed to evaluate the change in HCC incidence in Brazil. However, in several countries, a rising incidence of HCC has been related to an increasing prevalence of HCV infection.9,10 As in other studies conducted in countries with a low prevalence of HCC, our study confirmed that HCV infection was more frequently involved in HCC etiology than HBV infection.11,12 Apart from HCV, other factors may be associated with an increased prevalence of HCC in these areas of low prevalence; for example, an increase in the incidence of risk factors for nonalcoholic fatty liver disease.13 Currently, HCC is the main cause of death among patients with compensated cirrhosis.14 This fact may be associated with the widespread use of screening programs for early detection of HCC in patients with cirrhosis and better management of other cirrhotic complications.
In this study, liver cirrhosis was present in 98% of cases. In the last national survey, liver cirrhosis was present in 71% of cases.5 The majority of the questionnaire respondents in this study were hepatologists; this may explain the high proportion of liver cirrhosis observed in the HCC patients in this cohort. However, it does not explain the increase in liver cirrhosis compared with the 1997 survey.5
We observed a very important modification regarding the HCC diagnosis. In 1997, most patients were diagnosed with HCC based on histology (91%).5 In the present study, most patients (63%) were diagnosed with HCC based on imaging examinations; only 15% underwent a liver biopsy to confirm the HCC diagnosis. In 2005, the American Association for the Study of Liver Diseases updated a guideline published in 2000 by the European Association for the Study of Liver Diseases regarding the diagnosis and therapy of HCC.6 In the new guideline, a diagnosis of HCC could be confirmed with the presence of a focal hepatic lesion with typical vascularization in a patient with cirrhosis (arterial enhancement followed by washout in late phase) in one imaging examination for nodules >20 mm, or two imaging examinations for nodules <20 mm. We can assume that most of the questionnaire respondents in this study were aware of the non-invasive method for diagnosing HCC and attempted to follow international guidelines.
In patients with liver cirrhosis, surveillance with abdominal ultrasound is recommended for an early diagnosis of HCC.6 Our data supported the notion that AFP should not be used as a screening tool;15 most patients in the early stage of HCC had AFP levels ≤100 ng/mL. Unfortunately, we did not have the data to distinguish whether patients were following a regular surveillance program. Despite efforts to diagnose HCC early, only 43% of our cases were diagnosed in the early stage. Currently, a large number of patients are not diagnosed until the advanced stages. We found significant differences in the distribution of HCC stages among the different Brazilian regions. The Southern and Southeast regions showed a high prevalence of intermediate HCC; in the Mid-Western region, half the patients were in the early stage, but this should be interpreted with caution on account of the small number of patients included from that region. In the Northern region, nearly half the cases were in the advanced stage. In those patients, HCC therapy was very limited; our data indicated that over half of the patients in the advanced stage received no therapy because of tumor aggressiveness or cirrhosis.
We also found significant differences in the types of HCC therapy in different Brazilian regions. In the Southern region, percutaneous ablation for early HCC was performed more frequently than in other regions. In the Mid-Western region, the small number of cases did not allow a determination of the most frequent type of therapy. Chemoembolization predominated in all regions, and was the major type of treatment in the early and intermediate stages. This probably reflected the greater accessibility of transarterial therapy in all Brazilian regions. Also, our data showed that the selection of patients for liver resection was not very restrictive. Nearly half of the cases that underwent liver resection were not classified in the early stage. These data indicated that the recommendation guidelines for HCC therapy6 are not strictly followed in many centers.
Liver transplants were performed in 242 patients, but it was the initial therapy in only 56 of these patients. Most patients who underwent a liver transplant were given a bridge therapy to slow tumor progression. Although there is currently no consensus regarding the best therapy,6 most patients were treated with chemoembolization. In 2006, the policy for cadaveric liver distributions was modified, and liver transplantation became a more accessible therapy option for patients with HCC in the early stages. No data are available regarding the number of Brazilian patients who dropped off the liver transplant list, but the proportion of HCC patients that received transplants increased. Future studies must be performed to evaluate the efficacy of HCC therapies in Brazil.
One of the main limitations of this retrospective study was the fact that many of the forms were incomplete, and it did not include all the consecutive cases of HCC that were treated during the study period at each center. Furthermore, questions regarding survival and more information on liver transplants were on the questionnaire, but those questions were not properly completed. A prospective study should be performed to evaluate the impact of HCC treatment on patient survival.
CONCLUSIONSLiver cirrhosis was the main risk factor for the development of HCC in Brazil. HCC epidemiology, classification, and therapy selection varied among different Brazilian regions. HCV infection was the most common etiology of liver cirrhosis in patients with HCC. Efforts to increase surveillance programs in patients at risk for HCC development should be stimulated, because they are cost-effective in patients suitable for curative therapy. National efforts to stimulate organ donation should be encouraged to increase the number of liver transplantations. However, there remain some discrepancies in treatment indications. Chemoembolization was the most common therapy used for patients with HCC, including those in the early stages. Liver resection was sometimes indicated in patients with a high risk of recurrence. The majority of patients with advanced HCC did not have access to new molecular target therapies, such as sorafenib. Further studies must be performed to evaluate the impact of HCC treatment in Brazil.
We thank João Ítalo Dias França for performing the statistical analysis in this study and Ednalva Moraes for performing the data tabulation.
Brazilian HCC Study Group: Adávio de Oliveira e Silva, Aecio Flávio Meireles Souza, Agnaldo Soares Lima, Ajith Kumar Sankarankutty, Aline Lopes Chagas, Ana de Lourdes Candollo Martinelli, André Castro Lyra, Andreza Correa Teixeira, Arnaldo de Jesus Dominici, Ben-Hur Ferraz Neto, Carla Adriana Loureiro de Matos, Carlos A. Rodrigues Terra Filho, Carlos Eduardo Brandão Melo, Claudia Ivantes, Cristiane Valle Tovo, Danielle Brito, Denise Cerqueira Paranaguá-Vezozzo, Dominique Muzzillo, Enio Mente, Evandro de Oliveira e Sousa, Fabio da Silva Yamashiro, Fernanda Fernandes Souza, Fernando Gomes Romeiro, Francisco Carlos Souza, Giovanni Faria Silva, Helma Pinchemel Cotrim, Humberto Oliva Galizzi, Ivanete do Socorro Abraçado Amaral, Janaina Jabur, Jazon Almeida, Joao Galizzi Filho, Jorge M. Padilha Mancero, Lizomar de Jesus Maués P. Moia, Luiz Augusto Carneiro D'Albuquerque, Marcelo Abrahão Costa, Marcelo Bruno de Rezende, Marcelo Dias Sanches, Marcus Trippia, Maria da Penha Zago Gomes, Orlando Castro e Silva Jr, Pedro Duarte Gaburri, Raul Carlos Wahle, Raymundo Parana Filho, Regiane Saraiva de Souza Melo Alencar, Renato Ferreira da Silva, Renato Letrinta, Rita de Cássia Martins Alves Silva, Rogério Alves, Rosamar Eulira Fontes Rezende, Sérgio Ioshii, Simone Regina Souza da Silva Conde, Veronica Cardozo, Zulane da Silva Tavares Veiga.