To evaluate the clinical outcomes and identify the predictors of mortality in elderly patients undergoing peritoneal dialysis.
METHODS:We conducted a retrospective study including all incident peritoneal dialysis cases in patients ≥65 years of age treated from 2001 to 2014. Demographic and clinical data on the initiation of peritoneal dialysis and the clinical events during the study period were collected. Infectious complications were recorded. Overall and technique survival rates were analyzed.
RESULTS:Fifty-eight patients who began peritoneal dialysis during the study period were considered for analysis, and 50 of these patients were included in the final analysis. Peritoneal dialysis exchanges were performed by another person for 65% of the patients, whereas 79.9% of patients preferred to perform the peritoneal dialysis themselves. Peritonitis and catheter exit site/tunnel infection incidences were 20.4±16.3 and 24.6±17.4 patient-months, respectively. During the follow-up period, 40 patients were withdrawn from peritoneal dialysis. Causes of death included peritonitis and/or sepsis (50%) and cardiovascular events (30%). The mean patient survival time was 38.9±4.3 months, and the survival rates were 78.8%, 66.8%, 50.9% and 19.5% at 1, 2, 3 and 4 years after peritoneal dialysis initiation, respectively. Advanced age, the presence of additional diseases, increased episodes of peritonitis, the use of continuous ambulatory peritoneal dialysis, and low albumin levels and daily urine volumes (<100 ml) at the initiation of peritoneal dialysis were predictors of mortality. The mean technique survival duration was 61.7±5.2 months. The technique survival rates were 97.9%, 90.6%, 81.5% and 71% at 1, 2, 3 and 4 years, respectively. None of the factors analyzed were predictors of technique survival.
CONCLUSIONS:Mortality was higher in elderly patients. Factors affecting mortality in elderly patients included advanced age, the presence of comorbid diseases, increased episodes of peritonitis, use of continuous ambulatory peritoneal dialysis, and low albumin levels and daily urine volumes (<100 ml) at the initiation of peritoneal dialysis.
The total number of elderly patients initiating dialysis regimens is expected to increase due to rising life expectancies around the world. Data from the US Renal Data System (USRDS) indicate that the number of patients older than 80 who initiated dialysis increased from 7,054 in 1996 to 13,577 in 2003 1. In France, peritoneal dialysis (PD) is commonly used among elderly patients, and more than one-half of all PD patients are >70 years old. In Hong Kong, 80% of all dialysis patients are on PD, and the median age of these patients is 62 years 2. In Canada, the majority of patients starting dialysis are older than 65 years 3.
PD in elderly patients is increasingly important due to the rapid growth of this population. PD has several advantages and disadvantages in the elderly. Elderly patients have a higher incidence of intestinal complications, including diverticulosis, bowel perforations, and constipation. Moreover, many elderly patients have undergone previous abdominal surgeries, which increases the risk of adhesions and abdominal wall leaks. Older patients on dialysis also often have multiple comorbidities, including diabetes mellitus, hypertension and cardiovascular and cerebrovascular diseases 4. The under-utilization of PD in elderly patients is linked to the inability of the patient to perform PD exchanges due to functional impairments or cognitive dysfunction. Older age may frequently be associated with contraindications for peritoneal dialysis 5. Therefore, dialysis decisions in elderly patients must incorporate geriatric principles with an emphasis on an accurate assessment of patient autonomy, disabilities, and comorbidities 6.
There is no clear consensus concerning the optimal form of renal replacement therapy for elderly patients. Furthermore, little is known regarding the results of PD therapy in elderly patients. Thus, the aim of this study is to provide information regarding the clinical outcomes and survival rates of elderly patients treated with PD.
MATERIALS AND METHODSRecords of 58 elderly patients (>65 years and older) in our PD unit who began PD therapy between June 2001 and January 2014 due to end-stage renal disease (ESRD) were evaluated retrospectively. Eight patients were excluded from the study because their PD history was less than 90 days. The data from the remaining 50 patients were collected and evaluated. Neither open-label research nor questionnaires were used in our study. Moreover, ethical committee approval was not sought because of the retrospective nature of the study.
Age, gender, educational level, socio-demographic characteristics, the availability of someone to administer PD (e.g., themselves, their children or other persons, such as healthcare workers), and the nature of the use of PD (patient preference or a compulsory choice) were investigated in-depth using patient records. We noted whether the patient had previously received hemodialysis, and if so, the history of the hemodialysis treatment was recorded. The etiology of the ESRD and the presence of comorbid systemic diseases, such as hypertension, cardiovascular disease (CVD), cerebrovascular events, and malignancy, were recorded.
Systolic and diastolic blood pressure measurements, daily urine volumes, daily mean ultrafiltration (UF) amounts, and cardiothoracic indices were recorded for all patients at the beginning and at the end of the study.
Serum urea, creatinine, calcium, phosphorus, albumin, intact parathyroid hormone (iPTH), hemoglobin, transferrin saturation and ferritin values were recorded at the beginning of the PD treatment and at the final monitoring appointment. Initiation of PD for continuous ambulatory peritoneal dialysis (CAPD) refers to the time when the patient started to use the PD solutions effectively, which generally refers to performing 2-liter exchanges 4 times per day. Initiation of PD for automated peritoneal dialysis (APD) refers to when the patient started PD at the necessary exchange volumes, which typically takes approximately 2-3 weeks after PD catheter insertion to occur.
Incidences of infectious complications, including peritonitis and exit site/tunnel infections, were determined. Factors associated with mortality as well as patient and technique survival rates were analyzed. Technique failure was defined as the requirement for patient transfer to HD due to peritonitis, inadequate ultrafiltration, exit site and/or tunnel infections, or mechanical problems.
Statistical analyses were performed using the Statistical Package for the Social Sciences software (version 11.0; SPSS Inc., Chicago, IL, USA). χ2 tests were used to assess nonparametric variables. Independent sample t-tests were used to analyze clinical and biochemical parameters. Patient survival rates and technique survival rates were calculated using Kaplan-Meier analysis. Risk factors and calculated hazard ratios (HRs) for patient mortality and PD technique failure were also analyzed using backward logistic regression models based on the Cox proportional hazards method. Differences were considered statistically significant if the p-value was less than 0.05.
RESULTSOf the 367 patients who began PD during the study period, 58 met our inclusion criteria. Eight patients with a PD history of less than 90 days were excluded from our analysis. The mean age of the remaining 50 patients (including 31 females) at the time of the initiation of PD was 71.8±4.9 years. The mean PD duration was 26.5±20.2 months. The patient demographic data are presented in Table 1.
Demographic data of patients.
| Variable | Value |
|---|---|
| Age (years) | 71.8±4.9 |
| Gender (male/female) | 19/31 |
| Peritoneal dialysis duration (months) | 26.5±20.2 |
| Nature of PD decision (self/compulsory choice) | 21/29 |
| HD history (n), duration (months) | (12) 62.3±43.9 |
| Peritonitis incidence (patient-months) | 20.4±16.3 |
| Catheter exit site/tunnel infection incidence (patient-months) | 24.6±17.4 |
| Comorbid diseases | |
| Hypertension | 12% |
| Cerebrovascular accident | 10% |
| Coronary artery disease | 7% |
| Chronic obstructive pulmonary disease | 8% |
| Visual defects due to diabetic retinopathy | 10% |
| Malignancy | 4% |
| Etiology of renal failure | |
| Diabetic nephropathy (n:28) | 56% |
| Chronic glomerulonephritis (n:9) | 18% |
| Polycystic kidney disease (n:4) | 8% |
| Chronic pyelonephritis (n:4) | 8% |
| Amyloidosis (n:1) | 2% |
| Unknown/other (n:4) | 8% |
A total of 64% (n=32) of the patients performed PD with the help of another person, including their child, their spouse or another person, such as a healthcare worker. Fifty-eight percent of patients (n=29) made a compulsory choice to begin PD due to vascular access or social problems. Histories of HD use were present in 24% of the patients, and the mean period of HD therapy prior to PD was 62.3±43.9 (3-144) months.
Etiologies of renal failure included diabetic nephropathy (56%), chronic glomerulonephritis (18%), polycystic kidney disease (8%), chronic pyelonephritis (8%), amyloidosis (2%) and unknown causes (8%). In addition to diabetes, comorbid diseases included hypertension (12%), cerebrovascular accidents (10%), coronary artery disease (7%), chronic obstructive pulmonary disease (8%), malignancies (4%) and visual defects due to diabetic retinopathy (10%).
The clinical and laboratory data at the initiation of PD and at the final visit are presented in Table 2. The incidence of peritonitis was 20.4±16.3 patient-months; the incidence of infections at the catheter exit site/tunnel was 24.6±17.4 patient-months.
Clinical and laboratory data at the initiation of PD and the final visit.
| Parameters | At the beginning of PD | Final visit |
|---|---|---|
| Creatinine (mg/dl) | 7.3±2.9 | 6.2±2.4 |
| Albumin (g/dl) | 3.5±0.5 | 3.6±0.7 |
| Calcium (mg/dl) | 9.1±0.8 | 9.2±0.9 |
| Phosphorus (mg/dl) | 4.5±1.7 | 3.9±1.5 |
| Parathormone (pg/ml) | 255±358 | 290±380 |
| Hemoglobin (g/dl) | 10.7±1.7 | 11.8±2.0 |
| Cardiothoracic index (%) | 50±0.5 | 49±0.5 |
| Systolic blood pressure (mmHg) | 115±26 | 102±28 |
| Diastolic blood pressure (mmHg) | 70±14 | 62±13 |
| Ultrafiltration (ml/day) | 988±511 | 982±457 |
| Urine volume (ml/day) | 562±425 | 502±390 |
The PD modality was CAPD in 74% of patients (n=37); 3 of these patients eventually required a transfer to APD (n=16). The mean following time of APD therapy was 19.8-12.9 months. When compared with patients treated with APD, the hemodialysis duration was longer in patients receiving CAPD treatment (p=0.024). In patients receiving CAPD treatment, initial and final UF amounts were greater and systolic blood pressures and urine volume levels were lower than in patients treated with APD (p=0.014, <0.001, 0.008 and 0.023, respectively). In 80% of the APD group and 50% of the CAPD group, the procedure was performed by someone other than the patient (p=0.04). Factors that similarly affected CAPD and APD patients (p>0.05) included age, gender, etiology, educational status, nature of the PD decision, and incidences of peritonitis and catheter exit site/tunnel infections.
During the follow-up period, only 10 patients continued to receive PD treatments. None of the patients received kidney transplants (Table 3), and 30 patients died. Of the patients who died, 10 were treated with APD and 20 were treated with CAPD. The mortality rate was higher in patients treated with CAPD (p<0.001). Most of these deaths were caused by cardiovascular events (30%) and peritonitis and/or sepsis (50%). The underlying causes of peritonitis and/or sepsis were Gram-negative bacteria (Escherichia Coli, Enterobacter and Pseudomonas species) in 6 patients, Klebsiella and Acinetobacter species in 4 patients, and fungi in 1 patient. The causative microorganisms could not be isolated in 4 patients. In total, 10 patients were transferred to HD because of infectious complications associated with PD (50%), PD insufficiency (30%), and malnutrition (20%). Severe peritonitis with Gram-negative bacteria (Escherichia coli, Enterobacter and Pseudomonas species) in 4 patients and frequent peritonitis in 1 patient warranted mandatory transfers to HD.
Final status of the patients.
| Cause | % |
|---|---|
| Death (n:30) | |
| Sepsis/peritonitis (n:15) | 50 |
| Cardiovascular events (n:9) | 30 |
| Malnutrition/PD insufficiency (n:3) | 10 |
| Unknown (n:3) | 10 |
| Transfer to hemodialysis (n:10) | |
| Sepsis/peritonitis (n:5) | 50 |
| PD insufficiency (n:3) | 30 |
| Malnutrition (n:2) | 20 |
| Continued PD treatment (n:10) |
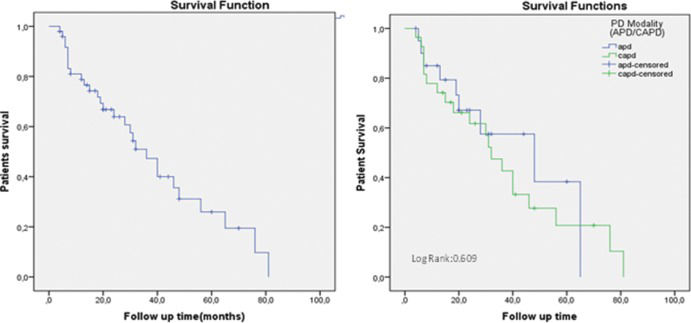
The mean survival time for all patients was 38.9±4.3 months based on the Kaplan-Meier analysis. The survival rates were 78.8%, 66.8%, 50.9% and 19.5% at 1, 2, 3, and 4 years, respectively. No significant difference was observed in the survival rates between the two PD groups (log rank: 0.609) (Figures 1A and 1B). Patient age, nature of the PD decision (self vs. mandatory), administration form (self vs. by someone else), HD history status, history of additional systemic diseases, PD treatment modality (CAPD and APD), pretreatment urine volume (>100 ml/day vs. <100 ml/day), incidence of peritonitis and catheter exit site/tunnel infections, pretreatment serum albumin levels, systolic (SBP) and diastolic (DBP) blood pressures, and UF volumes were analyzed using Cox proportional hazard models and backward stepwise likelihood ratios (LRs) to identify independent risk factors for patient mortality. Predictors of increased mortality included advanced age, the presence of additional systemic diseases, increased episodes of peritonitis, CAPD modality, and low serum albumin levels and daily urine volumes (<100 ml) at the initiation of PD (Table 4).
Multivariate Cox proportional hazards model for patient survival
| RR | 95% Cl | p-value | |
|---|---|---|---|
| Age | 0.748 | 0.595-0.940 | 0.013 |
| Presence of comorbid disease | 8.326 | 3.34-18.416 | 0.02 |
| Incidence of peritonitis | 0.238 | 0.085-0.664 | 0.006 |
| Pretreatment low serum albumin | 0.170 | 0.042-0.831 | 0.025 |
| Pretreatment urine volume | 1.004 | 1.001-1.008 | 0.021 |
| PD modality (CAPD) | 2.861 | 1.281-17.879 | 0.018 |
The mean technique survival duration was 61.7±5.2 months based on Kaplan-Meier analysis. The technique survival rates were 97.9%, 90.6%, 81.5%, and 71% at 1, 2, 3, and 4 years, respectively. Technique survival rates were similar between the two PD modalities (log rank: 0.788) (Figures 2A and 2B). Patient age, nature of the PD decision, administration form (self vs. by someone else), HD history, history of additional systemic diseases, pretreatment urine volume, incidence of peritonitis and catheter exit site/tunnel infections, PD treatment modality (CAPD and APD), pretreatment serum albumin levels, SBP, DBP, and UF volumes were analyzed using Cox proportional hazard models and backward stepwise LRs to identify independent risk factors affecting the technique survival rates. None of the factors, including PD modality, were significant predictors of technique survival.
DISCUSSIONIn this study, advanced age, presence of comorbid systemic diseases, increased episodes of peritonitis, CAPD modality, low serum albumin levels and low daily urine volumes at the initiation of PD were poor predictors of patient survival in elderly PD patients. Infectious complications and cardiovascular events were the main causes of death, whereas the most significant factor in warranting patient transfer to HD was the presence of peritonitis and/or sepsis.
Dialysis for older patients with ESRD is a significant challenge for healthcare providers. These individuals are often referred to nephrologists during the later stages of the disease. Moreover, these patients tend to have more comorbidities such as cardiovascular diseases, malnutrition, and hearing and visual impairments 7,8. All of these factors are problematic for any dialysis modality. The prevalence of elderly patients requiring renal replacement therapy has also been increasing in recent years. Genestier et al. reported that 15% of the PD population was elderly and projected that this proportion would increase to 40-41% in the future 9. The elderly PD population in our study accounted for 15.8% of all PD patients at our facility.
As the proportion of the older population increases, the number of older PD patients will also increase. Mortality rates in elderly PD patients are not favorable. In our study, the mean survival time was 38.9 months, and the mean survival rates were 78.8%, 66.8%, and 50.9% at 1, 2, and 3 years, respectively. Mortality rates in the present study were higher than observed in a previous study of ours that evaluated all of our PD patients between 2001 and 2010 10. Different results are observed in other centers and other countries. One of the reasons for some of the discrepancies in the reports is the lack of a standard definition of “elderly patient.” Some authors, including us, consider patients over 65 years of age as elderly, but heterogeneity regarding this definition exists between studies.
Elderly patients on PD can attain favorable outcomes: the 2- and 5-year survival rates of patients over 65 years of age in Hong Kong were reported to be 88% and 56%, respectively 11. A study evaluating patients over 80 years of age reported a 12-month survival rate of 83% and a 24-month survival rate of 41%. These numbers are higher than those of other similar studies, which is most likely due to the presence of fewer comorbid conditions in the patients included in their study.
Most reports of dialysis outcomes in elderly patients are retrospective and use varying definitions of elderly. The North Thames Dialysis Study 13 was a large prospective study that defined elderly as 70 years of age or older when starting dialysis. In this study, survival was assessed in 125 patients (age 70-86 years), and the overall 1-year survival rate was 71%. De Vecchi et al. 14 compared the outcomes of 63 consecutive non-diabetic patients older than 70 years who were treated with CAPD with the outcomes of 86 non-diabetic patients aged 40-60 years who were treated over the same period. The 2-year patient survival rate was, not surprisingly, lower in the older group (68% vs. 82%, p < 0.001). Kadambi et al. 15 compared the outcomes of three groups of patients of different ages (<50 years, 50-64 years, and >65 years); over 90% of the patients were receiving APD. This was a large retrospective study of 493 patients, 192 of whom were older than 65 years. The authors found that patients over 65 years of age had a higher mortality rate than the group of younger patients.
The reasons underlying the different survival rates may be multifactorial in elderly patients. Recent data indicate that age and the presence of comorbid conditions play a significant role in dialysis mortality 16-20. Demographic characteristics of patients (age, presence of diabetes, number of comorbid diseases, presence of malnutrition, low residual renal function, presence of hemodialysis history) were generally different in all of these study populations 16,21-23. In the Cox proportional hazard model used in our study, advanced age, the presence of comorbid systemic diseases, increased episodes of peritonitis, CAPD modality, and low serum albumin levels and low daily urine volumes at the initiation of PD were predictors of poor patient survival. Weinhandle et al. also observed increased survival of PD in patients less than 65 years of age without comorbid conditions 20. Kurella et al. observed a decreasing mean survival rate after dialysis initiation in the older dialysis population, with a result of 24.9 months in patients aged 65 to 79 years, 15.6 months in patients aged 80 to 84 years, 11.6 months in patients aged 85 to 89 years and 8.4 months in patients aged 90 years and older 1. The authors also showed that the dialysis population had a substantially lower average life expectancy of 48 to 89 months compared with the age-matched general population 1.
Dialysis may not confer a survival benefit in elderly patients with significant comorbidities. As expected, the survival of patients receiving PD was affected by comorbidities. In addition, comorbidities were associated with the mortality risk of patients receiving PD in an age-independent manner 24,25. A study conducted in London by Murtagh et al. also demonstrated a survival benefit for dialysis treatment in the elderly (>75 years) 26. However, in patients with ischemic heart disease or significant comorbidities (score=2 in the comorbidity scoring system by Davies et al.) 27, no survival benefit was observed for dialysis treatment. In our study, we found that the presence of comorbid conditions negatively affected patient survival.
Malnutrition is common in ESRD patients and is a powerful predictor of morbidity and mortality. In general, elderly patients on any type of dialysis have poor nutritional status. Studies comparing nutritional statuses of PD and HD patients are scant, but there is no clear evidence that nutritional status is worse in elderly PD patients despite the potential for protein loss in the effluent 28. PD patients may be severely hypoalbuminemic at the initiation of dialysis 29 and may remain at higher risk of malnutrition due to constant protein loss in the effluent. Moreover, malnutrition may be significantly higher among high peritoneal transporter patients and in patients experiencing peritonitis. We suspect that this effect accounts for the decreased survival rate in patients with lower serum albumin levels at the initiation of PD.
Peritonitis is a major complication in patients receiving PD. Peritonitis is the major cause of technique failure and represents a significant cause of morbidity and mortality 30. The reported rates of peritonitis in elderly patients have varied in the literature. Rates have been reported to be higher than, similar to, or lower than the rates observed in younger patients 14,15,31-36. Elderly patients could be more susceptible to peritonitis because of functional impairments, immunodeficiency and diverticulitis. Our results showed that the incidence of peritonitis was similar to the ISPD Guidelines target 37. The higher peritonitis incidence in our patients was probably due to the high rate of administration of PD by someone other than the patient.
Cardiovascular disease is prevalent in CKD patients. In fact, it is the most frequent cause of death in CKD patients, accounting for approximately 50% of all deaths 38. A report from a Far-Eastern country suggested that the most significant causes of death in CKD patients were infections (61%) and cardiovascular events (39%) 39. These data correlate well with our study, as we also found that the most frequent causes of death were infections (peritonitis and/or sepsis) and cardiovascular events.
Inter-study variability exists regarding the definition of technique failure. Many studies, including the present study, define technique failure as a requirement for transfer to HD 40,41. However, some authors define technique failure as death or a requirement for transfer to HD 42. In addition to the differences between definitions, technique survival rates may differ between countries or even between clinics in the same country 39,40,43. The most common causes of transfers from PD to HD were PD-related infections and inadequate dialysis 39. Similarly, infections (peritonitis and/or sepsis) and inadequate dialysis were the most important causes of technique failure in our study. The mean technique survival duration was 61.7±5.2 months, and the technique survival rates were 97.9%, 90.6%, 81.5% and 71% at 1, 2, 3 and 4 years, respectively. These data are consistent with similar studies from the literature 14. We could not find any significant risk factors with effects on technique survival, which was probably because of the small size of the study population that was transferred to HD.
In conclusion, although different survival rates in PD patients have been reported in different studies, mortality was high in elderly PD patients in our study. The factors affecting mortality and survival rates in our elderly patients are advanced age, the presence of comorbid systemic diseases, increased episodes of peritonitis, and low serum albumin levels and diastolic blood pressures at initiation of PD. Transfers to HD and death were the most common causes of withdrawal from PD. Infectious complications and cardiovascular events were the main causes of death, whereas peritonitis and/or sepsis and inadequate dialysis were the most prevalent reasons for transferring to HD.
AUTHOR CONTRIBUTIONSSakaci T, Koc E and Basturk T designed the study, collected and analyzed the data, and wrote the paper. Ahbap E was involved in designing the study and collecting the data. Sevinc M and Kara E performed the data collection and statistical analysis. Caglayan FB and Sahutoglu T performed language corrections. Ucar A, Sinangil A, Akgol C, and Kayalar AO collected the data. Ünsal A performed the final editing of the manuscript.
No potential conflict of interest was reported.