The multifactorial nature of falls among elderly people is well-known. Identifying the social-demographic characteristics of elderly people who fall would enable us to define the typical profile of the elderly who are at risk of falling.
OBJECTIVE:We aimed to isolate studies in which the social-demographic risk factors for falls among the elderly have been evaluated and to carry out a meta-analysis by combining the results of all of these selected studies.
METHOD:We did a systematic literature review using the key words “accidental fall / numerical data” and “risk factors.” Inclusion criteria entailed the selection of articles with the following characteristics: population of subjects aged 60 years or over, falls that took place in everyday life, and social-demographic risk factors for falls.
RESULTS:3,747 indexed articles published between 1981 and 2007 were identified, and 177 studies with available data were included, of which 129 had data on social-demographic risk factors for falls. Difficulties in activities of daily living (ADL) or in instrumental activities of daily living (IADL) double the risk of falling: The OR and 95% Cl were 2.26 (2.09, 2.45) for disturbance ADL and 2.10 (1.68, 2.64) for IADL. The OR and 95% Cl for Caucasians were 1.68 (0.98 - 2.88) and 0.64 (0.51 - 0.80) for Hispanics. In the subgroup of patients older than eighty, being married protected people from falling with an OR and 95% Cl = 0.68 (0.53 - 0.87).
CONCLUSION:Defining factors that create a risk of falling and protect elderly people from falls using social-demographic characteristics lets us focus on an “at risk” population for which a specific program could be developed.
Several studies have demonstrated the multifactorial nature of falls among the elderly.1,2 The consequences of such an event, beyond the dangers of morbidity and mortality, are a loss of autonomy and a significant risk of institutionalization.3-5 This loss of autonomy and institutionalization, which were already identified in reviews on this topic, highlight the spiral into which the elderly person who experiences a fall descends, and then there are further factors that increase the risk of more falls.6 During a visit to the emergency department (ED) after a fall, at-risk populations could be identified. However, the medical staff is nearly always reassured by the absence of traumatic consequences, and they propose no medical or environmental changes for those discharged after their ED visit.7
Identifying the social-demographic characteristics of this population would enable us to define the typical profile of the elderly people at risk of falling. These data could be extremely useful to guide at-risk subjects and to develop preventative programs.
The purpose of this study, therefore, was to identify studies where social-demographic risk factors for falls among elderly subjects were evaluated and then to conduct a meta-analysis for each of the identified risk factors to determine the adjusted odds ratios.
MATERIAL AND METHODSSearch strategy and selection of articlesOriginal articles published in English or French between 1996 and 2007 were collected using a computerized search on the MEDLINE and the Cochrane Collaboration databases. A manual search for the articles cited within the previously identified publications completed the compilation. The keywords used were the MeSH terms “accidental fall / numerical data” and “risk factors.” “Numerical data” was used to capture articles focusing on quantitative data.
Articles were selected if they were (i) studies involving a population aged over 60, (ii) pertaining to falls in daily life (excluding falls from ladders, scaffolding, and cliffs and/or those involving a cohort suffering from serious neuro-muscular disease), and (iii) targeting one or more risk factors for falls. Letters to the editor, commentaries, editorials, and meta-analyses were not selected.
Evaluation of articles allowed us to exclude some of them, mainly for technical reasons. Those not selected lacked data on the main evaluation criteria. We also discarded articles about the same study published in different journals.
This article focuses on a systematic research of all articles that include information about social-demographic characteristics in the elderly that are risk factors for falls, namely the age, gender, ethnicity, marital status, place of residency, autonomy, level of education, and income.
Data Extraction and quality assessmentTwo readers (MT & FB) independently selected all the abstracts of articles derived from the search. Each reader gathered information on half of the studies. To detect potential bias in the data abstraction process, data from a randomly selected 25% of articles were independently extracted by each of the two readers in order to evaluate the degree of inter-reader concordance. Discrepancies were resolved by consensus with a third party if necessary (GK). Few discrepancies were observed (6.4% error), and a double extraction on all items was not performed.
The quality of each study chosen was assessed by two readers using a validated scale proposed by the ANAES8 and derived from the recommendations of Cook et al.9 This scale gave a level of proof for function of methodology, study power, randomization, population, data collection, and biases. Level 1 proof is synonymous with established scientific proof, level 2 denotes scientific assumption, and levels 3 and 4 refer to a low degree of scientific proof.
The abstracted data included the study characteristics (including quality criteria), the patient characteristics, and fall definitions (one or more falls, more than one fall, and traumatic falls). For qualitative variables, the following frequencies were collected: number of fallers with a risk factor for falls, number of fallers without a risk factor for falls, number of non-fallers with a risk factor for falls, number of non-fallers without a risk factor for falls. For quantitative variables, the mean and standard deviation for the groups of fallers and non-fallers were collected.
Statistical analysisA meta-analysis was performed for each social-demographic characteristic. The odds ratio (OR) and confidence interval of 95% were estimated for each study and overall to assess the risk of falls associated with these characteristics. The fixed-effects method proposed by Mantel-Haenszel10 was used. Heterogeneity between studies was assessed using standard methods, in particular the Chi-square test11 and the I2 statistic.12 A value of I2 less than 25% indicates low heterogeneity, and a value between 25 to 50% indicates moderate heterogeneity. Regardless of the statistical significance of the Q test,13 we applied a random effects model that allows meta-analysis to consider between-study variations. In cases of significant heterogeneity, some features that might be potential sources of heterogeneity received special attention (population, intervention endpoint). We conducted stratified analysis of these characteristics or analyses of sensitivity based on the methodological quality of the studies. We also used Begg's funnel plots14 and Egger's test15 to detect possible publication bias. All statistical tests were conducted with the Review Manager software suite RevMan Version 5.0 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008). We defined a statistical test with a p value of less than 0.05 as significant.
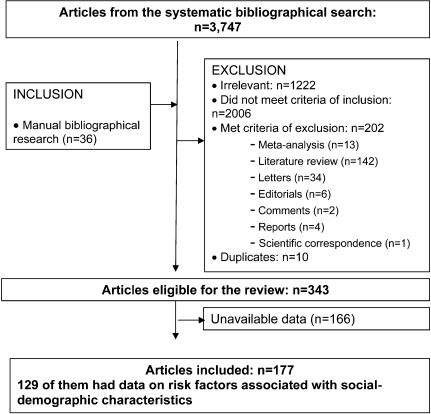
RESULTSTrial FlowThe flow chart of our study is shown in Figure 1. The computerized search strategy identified 3,747 articles published from 1981 to 2007. We excluded 3,219 articles, retaining only 326 articles, then added 36 references from the manual search to obtain 362 studies. After verifying the data and removing duplicates, we included 177 studies, 129 of which specifically presented data on social-demographic characteristics as risk factors for a fall.16-141 The “funnel plots” of each meta-analysis, representing the estimated values of the OR according to the size of the population, were distributed symmetrically.
Study CharacteristicsTwenty-four social-demographic conditions were identified as a risk factor for falls: age, gender, ethnicity (5 conditions), marital status (3 conditions), lifestyle (6 conditions), autonomy (5 conditions), level of education, and income (2 conditions). The 129 articles were published between 1981 and 2007. Eighty-two studies had as a main outcome the occurrence of one or more falls, 9 studies included the occurrence of more than one fall, and 5 studies included the occurrence of traumatic falls. The number of elderly subjects participating in these studies was between 33 and 1,1390 reporting between 13 and 2,278 falls; this represents a prevalence ranging from less than 5% falls to more than 65% (i.e., an average prevalence of 35.5% in these studies). The mean age was 78.6 years (68.1 to 88.5). Sixty percent of studies (n = 57) included follow-up periods of 7 to 12 months, 19% were under or equal to 6 months, 11% from 13 to 24 months, and 2% over 24 months.
Study qualityBased on the methodological characteristics selected, only 2% of the studies selected were ranked as containing level 1 evidence (i.e., randomized controlled trials of high power). All except one were observational studies, 37 studies were cohort studies (39%) with level 2 evidence, and 16 studies were case-control studies with level 3 evidence (17%). Forty-one were cross-sectional (44%) and were considered to have a low level of scientific evidence (level 4).
Results of meta-analysisAn OR with 95% CI could be calculated for the female subjects in 88 studies. Its value was 1.52 (1.45 - 1.59) but with a high heterogeneity. Stratified analyses (Table 1) were used to calculate the OR depending on the type of fall and age or living environment. Only the institutionalized group of patients gave homogeneous results for an OR of 1.15 (95% CI 1.02 - 1.29). Data on age were present in 57 articles, allowing us to calculate an average age difference for the fall. The results are presented in Table 1. Two meta-analyses were carried out for ethnicity. The OR and 95% Cl for Caucasians were 1.68 (0.98 - 2.88); the corresponding value for Hispanics was 0.64 (0.51 - 0.80). These two results were homogenous. It was not possible to perform a meta-analysis for Australians, Asians, and African-Americans because there was an insufficient number of good-quality studies.
Pooled Odds Ratios (OR) and subgroup sensitivity analysis for gender and age.
| Study Characteristic | n | Gender OR (95% CI) | n | Age Mean Difference (Fixed, 95% CI) |
|---|---|---|---|---|
| No. of studies | 88 | 57 | ||
| No. of subjets | 92 025 | 50 431 | ||
| Population | 49 | 1.52 [1.45, 1.59] | 30 | 2.65 [2.69, 2.60] |
| Living | ||||
| Institution | 17 | 1.15 [1.02, 1.29]∗ | 10 | 1.12 [1.57, 0.67] |
| Ambulatory | 28 | 1.69 [1.61, 1.79] | 20 | 2.66 [2.71, 2.62] |
| Both | 4 | 0.76 [0.63, 0.92] | 0 | na |
| Evaluation criteria | ||||
| One or more falls | 37 | 1.53 [1.44, 1.62] | 25 | 2.65 [2.70, 2.61] |
| More than one fall | 8 | 1.35 [1.14, 1.60] | 5 | 1.69 [2.35, 1.03]∗ |
| Traumatic falls | 4 | 1.53 [1.41, 1.67] | 0 | na |
| Mean age of study subjects | ||||
| > 80 years | 21 | 1.02 [0.92, 1.14] | 12 | 1.19 [1.62, 0.76]∗∗ |
| ≤ 80 years | 19 | 1.75 [1.65, 1.85] | 18 | 2.66 [2.71, 2.62] |
| Unknown | 9 | 1.25 [1.10, 1.42] | 0 | na |
Cl = confidence interval;
The OR and 95% Cl were 2.26 (2.09, 2.45) (Figure 2a) for disturbance of one or more activities of daily living (ADL), 2.10 (1.68, 2.64) for disturbance of one or more instrumental activities of daily living (IADL), 2.18 (1.74, 2.73) for motor autonomy limited to the neighbourhood, and 1.73 (1.44, 2.08) for institutionalized patients. These results were homogenous except for those on ADL (Table 2), but for this group, data became homogenous in the subgroup of ambulatory patients.
Pooled Odds Ratios (OR) and subgroup sensitivity analysis for elements of autonomy.
| Study Characteristic | n | disturbance of one or more ADL OR (95% CI) | n | disturbance of one or more IADL OR (95% CI) | n | Autonomy limited to the neighbourhood OR (95% CI) | n | In stitution alised OR (95% CI) |
|---|---|---|---|---|---|---|---|---|
| No. of studies | 16 | 5 | 8 | 10 | ||||
| No. of subjets | 19 232 | 2 957 | 2 316 | 5 925 | ||||
| Population | 13 | 2.26 [2.09, 2.45] | 4 | 2.10 [1.68, 2.64]∗ | 7 | 2.18 [1.74, 2.73]∗ | 7 | 1.73 [1.44, 2.08]∗ |
| Living | ||||||||
| Institution | 5 | 2.23 [1.75, 2.86] | 0 | na | 1 | 1.31 [0.67, 2.55] | na | - |
| Ambulatory | 8 | 2.29 [2.09, 2.51]∗ | 4 | 2.10 [1.68, 2.64]∗ | 6 | 2.34 [1.83, 2.98]∗ | na | - |
| Both | 0 | na | 0 | na | 0 | na | na | - |
| Evaluation criteria | ||||||||
| One or more falls | 7 | 2.25 [2.05, 2.48] | na | - | 6 | 2.14 [1.68, 2.73]∗ | 5 | 1.65 [1.35, 2.02]∗∗ |
| More than one fall | 4 | 2.46 [1.86, 3.26] | na | - | 1 | 2.48 [1.33, 4.63] | 2 | 2.19 [1.41, 3.40]∗ |
| Traumatic falls | 2 | 2.37 [1.85, 3.03]∗ | na | - | 0 | na | 0 | na |
| Mean age of study subjects | ||||||||
| > 80 years | 6 | 2.11 [1.69, 2.65] | 2 | 2.27 [1.69, 3.06]∗ | 3 | 3.29 [1.68, 6.43]∗ | 4 | 1.59 [1.28, 1.98]∗∗ |
| ? 80 years | 5 | 2.31 [2.09, 2.54]∗∗ | 2 | 1.89 [1.33, 2.70] | 3 | 1.72 [1.24, 2.39]∗ | 3 | 2.17 [1.54, 3.04]∗ |
| Unknown | 2 | 2.37 [1.85, 3.03] | 0 | na | 1 | 2.48 [1.33, 4.63] | 0 | na |
Cl = confidence interval;
The OR and 95% Cl were not significant for the condition of low education level (0.97 (0.83 - 1.13)), married status (1.04 (0.94 - 1.15)); Fig. 2b), confined to bed (0.92 (0.70 - 1.20)), presence of a caregiver (1.26 (0.99 - 1.60)), and in the limit of significance for “living alone” (1.16 (1.02 - 1.32); Fig. 2c (Table 3)). However, in the subgroup of patients older than eighty, being married was protective against falling with an OR and 95% Cl = 0.68 (0.53 - 0.87) with a moderate homogeneity.
Pooled Odds Ratios (OR) and subgroup sensitivity analysis.
| Study Characteristic | n | Low level of education OR (95% CI) | n | Married OR (95% CI) | n | Living alone OR (95% CI) | n | Presence of a caregiver OR (95% CI) | n | Confined to bed OR (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| No. of studies | 8 | 15 | 18 | 12 | 5 | |||||
| No. of subjets | 8 557 | 25 021 | 12 743 | 15 557 | 3 627 | |||||
| Population | 4 | 0.97 [0.83, 1.13]∗ | 8 | 1.04 [0.94, 1.15] | 12 | 1.16 [1.02, 1.32]∗ | 5 | 1.26 [0.99, 1.60] | 3 | 0.92 [0.70, 1.20] |
| Living | ||||||||||
| Institution | 0 | na | 1 | 0.51 [0.19, 1.35] | 1 | 1.87 [0.81, 4.32] | 3 | 1.15 [0.85, 1.57] | 2 | 0.81 [0.60, 1.07] |
| Ambulatory | 4 | 0.97 [0.83, 1.13]∗ | 7 | 1.05 [0.94, 1.16] | 8 | 1.12 [0.97, 1.31]∗ | 2 | 1.44 [0.99, 2.09]∗ | 1 | 3.89 [1.58, 9.56] |
| Both | 0 | na | 0 | na | 3 | 1.22 [0.93, 1.60]∗ | 0 | na | 0 | na |
| Evaluation criteria | ||||||||||
| One or more falls | 1 | 1.14 [0.89, 1.48] | 5 | 1.15 [1.03, 1.28] | 5 | 1.14 [0.91, 1.44]∗ | 5 | 1.26 [0.99, 1.60] | na | - |
| More than one fall | 0 | na | 2 | 0.45 [0.29, 0.68]∗ | 5 | 1.15 [0.95, 1.38]∗ | 0 | na | na | - |
| Traumatic falls | 3 | 0.88 [0.73, 1.07]∗ | 1 | 0.46 [0.28, 0.77] | 2 | 1.07 [0.72, 1.59]∗ | 0 | na | na | - |
| Mean age of study subjects | ||||||||||
| > 80 years | 1 | 1.06 [0.69, 1.62] | 4 | 0.68 [0.53, 0.87]∗∗ | 5 | 1.25 [1.01, 1.54]∗ | 5 | 1.26 [0.99, 1.60] | na | - |
| ≤ 80 years | 1 | 1.14 [0.89, 1.48] | 3 | 1.14 [1.02, 1.28] | 5 | 1.12 [0.93, 1.34]∗ | 0 | na | na | - |
| Unknown | 2 | 0.84 [0.68, 1.04] | 1 | 0.69 [0.22, 2.16] | 2 | 1.22 [0.93, 1.60]∗ | 0 | na | na | - |
Cl = confidence interval;
Because there were an insufficient number of studies of good quality, we were not able to perform a meta-analysis on conditions such as widowed or divorced, help for transfers, income less than $25,000, non driving, and mean Barthel index.
DISCUSSIONOur results confirm that loss of autonomy is a major risk factor for falls: difficulties in at least one activity of daily living or instrumental activities of daily living double the risk of falling. Similarly, a decrease of motor autonomy limited to the neighborhood and an institutionalization, where subjects witnessed the loss of functional or motor autonomy, increases the risk of falling in similar ratios.
These results are coherent with other studies showing that fall risk is closely related to ADL capability and that the maintenance of a high frequency of activity external to the house is very important for reducing fall risk.142 One explanation given was that there is a possible link between bone loss in elderly subjects and reduction of ADL. Oka et al. analysed the association between decreased ADL and annual bone changes after adjustment for age and concomitant disease and showed that annual rates of change in bone mineral density were significantly correlated with decreased ability to bend down from a seated position and to pick up small objects by the side of the chair for men and in reaching objects on a high shelf or cupboard and lifting heavy objects for women.143
The interaction of loss of autonomy, fear of falling, and risk of falls could be another explanation. Compared with those with a high score on the falls efficacy scale (FES), a 10-item rating scale to assess confidence in performing daily activities without falling,144 those with a low fall-related self-efficacy score had an increased risk of falling and had a greater decline in their ability to perform ADLS (p < .001): the total ADL score decreased by 0.69 activities among persons with low FES scores (≤75) but decreased by only 0.04 activities among persons with FES scores of 100. Furthermore, non-fallers who said they were afraid of falling had an increased risk of admission to an institution.145
Caucasian women seem also to be the ethnic group with the highest risk of falling. Moreover, having Hispanic origin and living in the United States seemed to protect against falls. This result is similar to findings made by Stevens et al. in 1998 showing that the fall-related death rate for non-Hispanic women was 1.9 times the rate for Hispanic women. These results suggested that the subgroup analyses revealed what overall fall-related death rates for men and women did not reveal: the increasing death rates among whites and non-Hispanics.146 The longitudinal Study of Elderly Mexican American Health (H-EPESE) found a similar prevalence of falls among older Mexican Americans and non-Hispanic Caucasians, indicating that potential modifiable conditions, such as functional deficits, arthritis, diabetes, and depressive symptoms, were independent risk factors for falls in this population. Finally, these different medical conditions for Hispanics and non Hispanics representing the independent risk factors for falls can explain the possible ORs differences.
Our study also pointed out the protective effect of marriage against falling, even though it was only in the subgroup of patients over eighty, and we were not able to perform a meta-analysis on conditions such as widowed or divorced. Recent scientific work has already established a causal impact of social relationships on health,147 and researchers have recognized a relationship between marital status and mortality. This higher risk of death for both men and women has also been illustrated by a study showing that a spouse's admission to an institution was deleterious for the partner even when adjusted for underlying disorders.148 A meta-analysis of cohort studies was conducted by Manzoli et al. to produce an overall estimate of the excess mortality associated with being unmarried in elderly individuals and showed that marriage had a protective influence that remained significant, although the effect size was reduced (RR = 0.94; 0.92-0.95).149 A possible mechanism for this association was that illness or death of the spouse may impose stress on a partner that may deprive the partner of social, emotional, economic, or other practical support.150
To define protective factors and risk factors of falls from social-demographic characteristics lets us focus on the population at risk of falling for which a specific targeted program could be developed. Evidence for reducing the number of fallers or the number of falls with one of these programs, even under the very favorable conditions of randomized trials, has always been very modest. However, a recent study showed that a physical activity program can slow cognitive decline and improve quality of walking in elderly persons suffering from dementia.151 This is a good reason to specifically target those most at risk of falling for whom interventions will be most beneficial.152 The interventions proposed would thus be multifactorial and correspond to exercise programs, medication, and living-space modifications, as appropriate.153