To evaluate the preoperative assessment of thyroid nodules using ultrasound studies and cytology of nodular aspirates.
SUBJECTS AND METHODS:2,468 patients with thyroid nodules were examined from 1999 to 2005. All patients were clinically examined and underwent ultrasonography followed by fine-needle aspiration biopsy (FNAB) and cytology.
RESULTS:Nodules larger than 10 mm were classified ultrasonographically in a 4-tier system and received a score according to the criterion of possible malignancy. Cytological examinations were conducted independently by 2 cytologists and classified as benign (score 1), indeterminate (score 2), suspicious (score 3), and malignant (score 6). Combining both scores, an index was generated that would indicate a higher probability of malignancy (benign, doubtful, suspicious, and malignant). Thyroid surgery was performed in 274 patients. Of those, 115 patients had a score of 2 to 5 and only 8 had a histological diagnosis of thyroid cancer (6.9%). For patients with a score of 5 (n = 51), 11.5% had a malignant lesion, and 51% of the 61 patients with a score of 6 had confirmed thyroid cancer. Of the 98 patients with a combined score of 7 to 10, 99% had a histological confirmation of malignancy.
CONCLUSIONS:The index score had a sensitivity of 94.1% and specificity of 77.5%. The overall accuracy was 85.8%. Therefore, we concluded that this methodology may improve the preoperative diagnosis of thyroid cancer in nodules larger than 10 mm. Association with other methods such as color Doppler echography, serum TSH concentration, galectin-3 expression analysis, and FDG/PET scan would be useful in avoiding the higher costs of thyroid surgical procedures.
Avaliar a possibilidade de diagnòstico pré-operativo de nódulos da tireóide (de diâmetro superior a 10mm) usando ultra-sonografia da glândula tireóide e citologia de punção aspirativa por agulha fina guiada pela ultra-sonografia.
CASUÍSTICA E MÉTODOS:Nódulos tireóideos (maiores que 10mm) foram classificados ultra-sonograficamente em graus de I a IV e escores numéricos de 1 a 4, de acordo com crescente possibilidade de malignidade. O exame citológico, subseqüentemente, classificou os nódulos como benigno (escore 1) indeterminado (escore 2) suspeito (escore 3) e maligno (escore 6). Somando-se os escores obtidos nas duas metodologias obtém-se um índice considerado benigno (índice combinado 2-4), duvidoso (índice combinado 5) suspeito para malignidade (índice combinado 6) e elevada probabilidade de malignidade (índice combinado 7 a 10). Cirurgia da Tireóide foi realizada em 274 pacientes, dos quais 64 apresentavam índice de 2-4; destes, apenas 2 pacientes (3,1%) apresentaram comprovação histológica de câncer. Em pacientes com índice 5 (n= 51), 11,8% apresentaram câncer de tireóide e, em 61 pacientes com índice 6, (n= 31), 51% tiveram diagnóstico confirmado de malignidade. O índice combinado de 7-10 (n= 98) apresentou 99% de pacientes com câncer de tireóide.
CONCLUSÕES:O índice combinado apresentou sensibilidade de 94,1% e especificidade de 77,5%. A precisão desta metodologia foi de 85,8%. Concluímos que o índice combinado pode ser útil no diagnóstico pré-cirúrgico do nódulo tireóideo, mormente se associado com outras metodologias como a ecografia com Doppler colorido, nível elevado de TSH sérico, análise de expressão de galectina-3 e imagens por FDG/PET.
Thyroid nodules are a common clinical finding, being more frequently found in women, in the elderly population, and in those exposed in the past to a period of iodine deficiency. With the more widespread use of high-resolution ultrasound for relatively low-cost imaging of the thyroid gland, the prevalence of nodules of randomly selected individuals has been estimated to be 19% to 67%.1–4 The clinical importance of thyroid nodules rests with the need to exclude thyroid cancer, which occurs in about 10% of those with nodules, depending on age, gender, radiation exposure history, family incidence of thyroid cancer, and possibly iodine intake.1 Papillary and follicular thyroid cancer (and variants) comprise the vast majority (90%) of all thyroid malignancies,4–6 and due to more efficient and adequate diagnostic tools, the observed yearly incidence is increasing.6,7 Controversy exists regarding the most cost-effective approach in the diagnostic evaluation of a thyroid nodule.5–7 In this paper, we present an approach to pre-surgical evaluation of the thyroid nodule using an index based on ultrasonographic and cytological studies that will enhance the ability of the attending physician to recommend thyroid surgery for selected cases.
PATIENTS AND METHODSWe examined 2,468 consecutive patients with thyroid nodular disease from 1999 to 2005. All patients underwent ultrasonographic examination (with an ALOKA SSD 500, Aloka Co, Tokyo, Japan) equipped with a 7.5 MHz linear probe. Ultrasound-guided fine-needle aspiration biopsy (USG-FNAB) was performed in all nodules with a diameter larger than 10 mm.
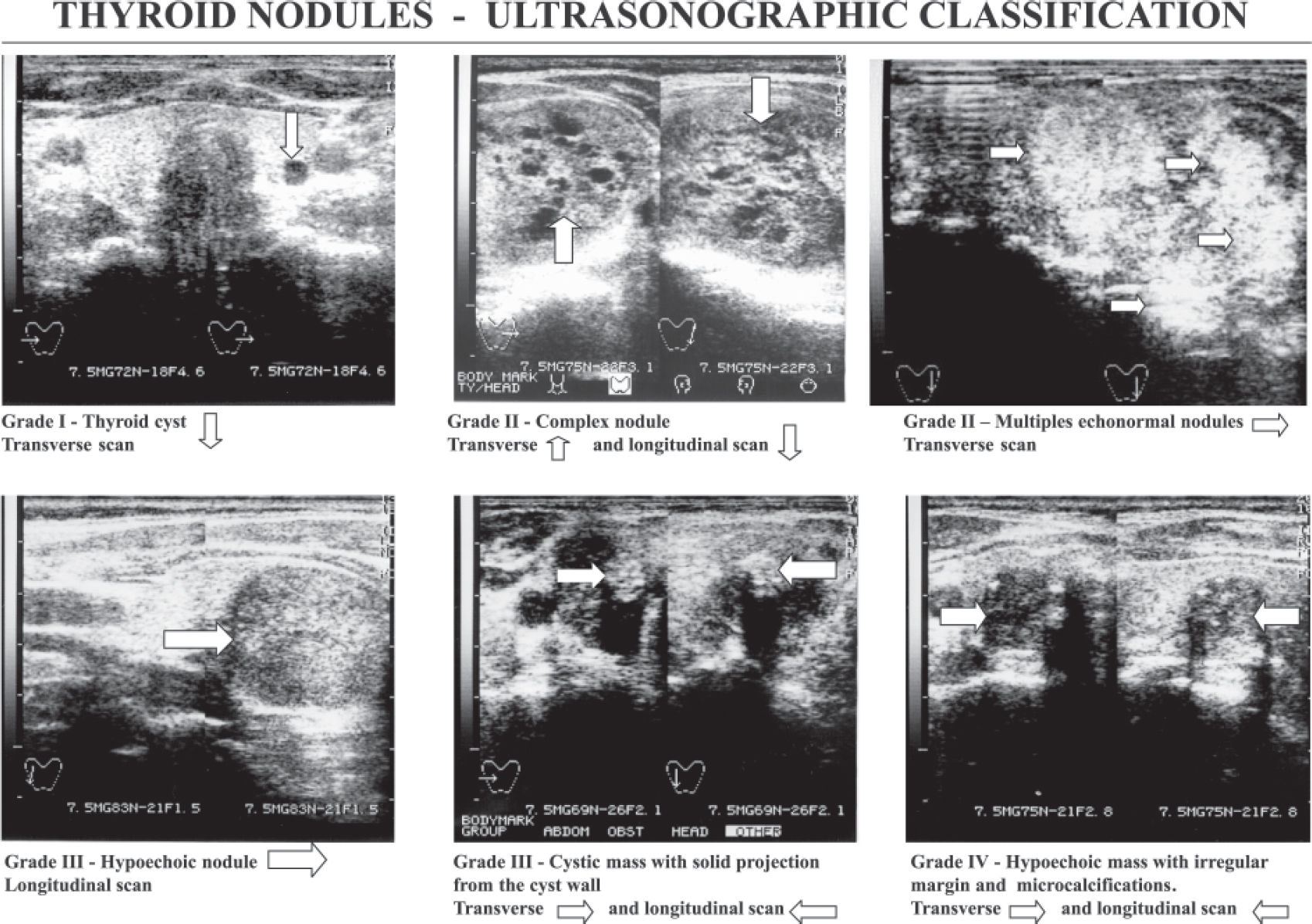
Ultrasonographic classification of the nodules (Figure 1).Each nodule was classified using a 4-tier system (grades I, II, III, and IV), and each grade received a score 1-4 according to criteria previously reported.8
Grade I (score = 1) small round and anechoic image, suggestive of a thyroid cyst.
Grade II (score = 2) multiple isoechoic or hyperechoic solid nodules with or without cystic change and coarse calcification, suggestive of adenomatous goiter. A single complex nodule (with cystic areas like a sponge) with the remainder of the gland with normal echographic texture could be a follicular adenoma.
Grade III (score = 3) a single isoechoic nodule or a hypoechoic solid nodule with a regular border, suggestive of a thyroid neoplasm. A cystic nodule with a solid projection from the cyst wall may represent a papillary carcinoma.
Grade IV (score = 4) hypoechoic solid nodule with an irregular border with microcalcifications is considered suspicious for papillary carcinoma.
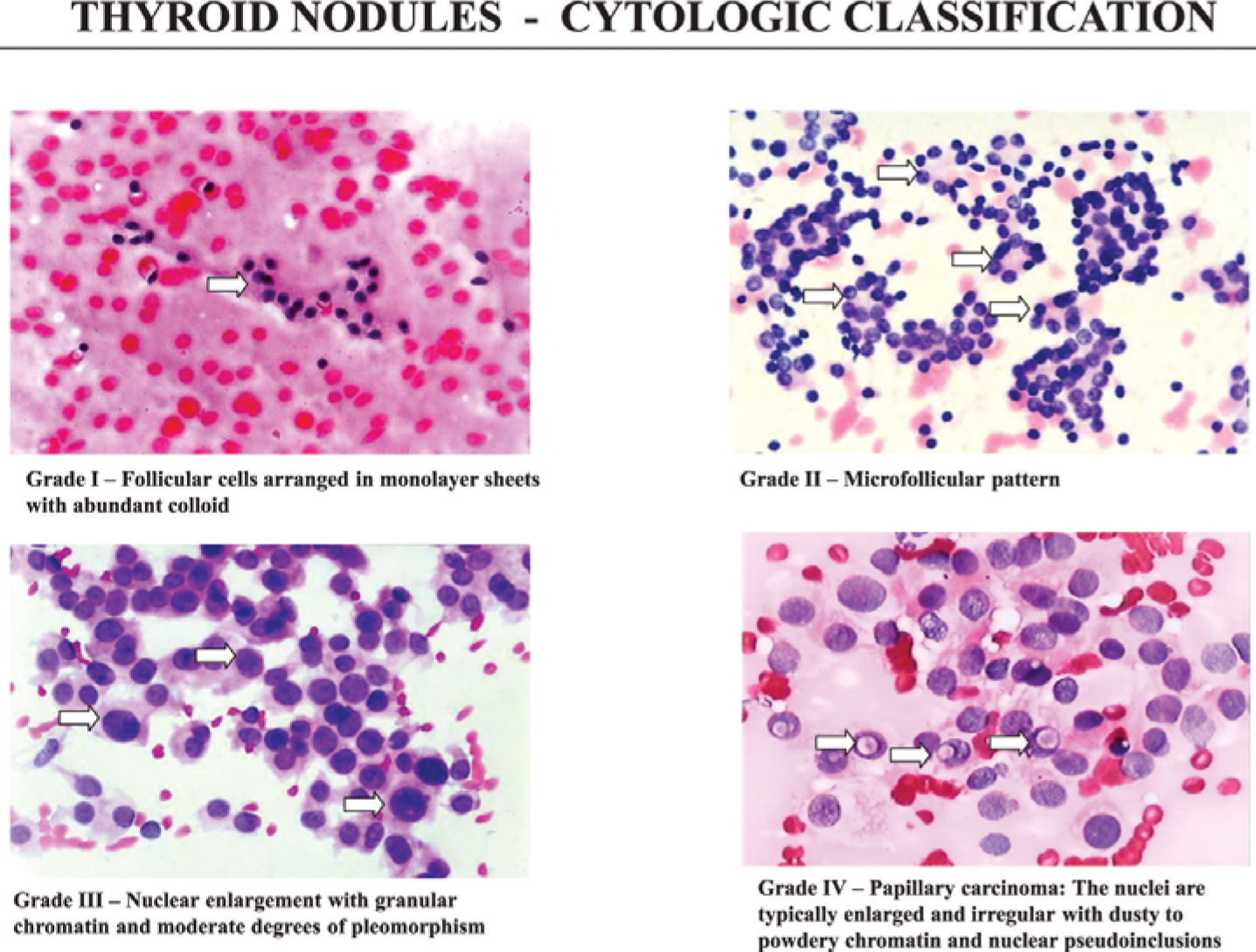
Cytological classification of USG-FNAB (Figure 2)Ultrasound-guided fine-needle aspiration biopsy (USG-FNAB) was performed using a 22 G needle and a 10 mL syringe. The aspirates were fixed in 96% alcohol and stained with hematoxylin-eosin. Cytological examinations were conducted independently by 2 experienced cytologists and classified as follows.8
Cytological classification of aspirates of thyroid nodules. From top left, clockwise: grade I, follicular cells with dense and homogeneous chromatin and abundant colloid; grade II, microfollicular pattern with nuclei with homogenous chromatin and scanty colloid; grade III, suspicious pattern with nuclear enlargement, prominent nucleoli, granular chromatin and absent colloid; and grade IV, malignant pattern represented by papillary carcinoma with enlarged and irregular nuclei, powdery chromatin and pseudoinclusions.
The FNAB was indeterminate. Note the intense FDG uptake with a SUV max. of 8.8. The histopathological diagnosis was a well differentiated, minimally invasive follicular cancer. Another lesion was found in the right lobe (papillary microcarcinoma of 4 mm is not identified in the FDG-PET16).
Benign pattern grade I (score = 1): epithelial cells distributed in cohesive clusters. The nuclei are round or oval with dense and homogeneous chromatin. The cytoplasm is scanty and slightly eosinophilic, but some oncocytic cell change may be present. Abundant colloid may be seen. This pattern is suggestive of nodular goiter.
Indeterminate grade II (score = 2): epithelial cells distributed in solid clusters or in microfollicular arrangements. The nuclei are round or oval with homogeneous chromatin. The cytoplasm is scanty or slightly eosinophilic. Colloid is absent or scanty. This pattern can be found in adenomatous goiter or in follicular neoplasm.
Suspicious pattern grade III (score = 3): epithelial cells distributed in solid clusters or in follicular arrangements. The nuclei are round or oval with nuclear enlargement, granular chromatin, and prominent nucleoli. The cytoplasm is slightly eosinophilic or may be large, deeply eosinophilic, and granular, characteristic of oncocytic cell change. Colloid is absent or scanty. This pattern is suggestive of neoplasm.
Malignant pattern grade IV (score = 6):
- a)
Papillary pattern—the epithelial cells are seen in a papillary arrangement. Round or oval nuclei are seen with nuclear pseudoinclusions and/or nuclear grooves.
- b)
Medullar pattern— the aspirates are typically hypercellular with noncohesive cells. The cells are variable in shape with round, oval, or spindle shapes. The nuclei are often eccentric with a plasmocytoid appearance. Amyloid is rarely seen.
- c)
Anaplastic pattern—small, giant multinucleated, and spindle cells are the predominant types in this pattern. The nuclei are usually large, bizarre, single or multiple, and coarsely clumped with prominent nucleoli. Atypical mitosis may be present.
- d)
Malignant lymphoma—monomorphic lymphoid cells (frequently associated with Hashimoto's thyroiditis).
Combining the scores of both ultrasonographic and cytological classification, we propose an index that would indicate, progressively, a higher probability of the presence of malignancy. Thus, an index of 2 to 4 is suggestive of a benign lesion, an index of 5 is doubtful, an index of 6 is suggestive of malignancy, and an index of 7 to 10 indicates a high probability for thyroid cancer.8
RESULTSPrevalence of thyroid cancer in the study population.Echographic studies and USG-FNAB (cytology)A total of 2,468 patients were referred from 1999 to 2005 to the Thyroid Unit for diagnostic ultrasound and possible USG-FNAB. All patients had a nodule larger than 10 mm in diameter. There were 198 (8.02%) men and 2270 (91.98%) women. No patient reported exposure to childhood head or neck irradiation, and no patients had a familial history of medullar carcinoma or multiple endocrine neoplasia.
From the total cohort of 2,468 patients, 274 underwent thyroid surgery. Of those, 115 patients with lower combined scores 2 to 5−5 underwent thyroidectomy by recommendation of their private physicians. Only 8 patients had a thyroid cancer confirmed in subsequent histological examination. As seen in Table 2, in patients with scores 2 to 4 (n = 64), a benign lesion was present in about 97% of the examined nodules.
Thyroid cancer prevalence in patients with thyroid nodules who underwent thyroid surgery (n = 274).
| Combined echographic and cytological scores (index score) | Number of patients | Malignancy confirmed (%) | |
|---|---|---|---|
| Total | Thyroid Cancer | ||
| 2-4 | 64 | 2 | 3.1 |
| 5 | 51 | 6 | 11.8 |
| 6 | 61 | 31 | 50.8 |
| 7-10 | 98 | 97 | 99.0 |
Sensitivity 94.1%; Specificity 77.5%; Positive predictive value 80.5%; Negative predictive value 93.0%; Accuracy 85.8%
For patients with a score of 5 (n = 51), 11.7% had a malignant lesion (Table 2). Malignant nodules were found in nearly 51% of patients with score 6 (n = 61). For patients with a combined score of 7 to 10 (n = 98), histologically confirmed thyroid cancer was present in 99%.
Thus, the index score had a sensitivity of 94.1% and a specificity of 77.5% for the preoperative prediction of thyroid cancer. Furthermore, the positive predictive value of the combined score was 80.5%, and the negative predictive value was 93.0%. Thus, accuracy of this numeric score for presurgical diagnosis was 85.8%.
As mentioned before, from the 2,468 studied patients, 274 underwent surgery, and 136 had a confirmed diagnosis of thyroid cancer after surgery (5.6%). The mean age of patients with thyroid cancer was 46.2 ± 6.9 yr (mean ± SD) compared with 40.1 ± 10.3 yr in those without cancer (NS). The types of thyroid cancer included 101 cases of papillary carcinoma, 22 of follicular carcinoma, and 13 of medullar carcinoma.
An association with thyroid cancer was detected for certain sonographic characteristics. In particular, the more cystic a nodule was (score 1), the lower the likelihood of malignancy. Hypoechoic nodules had a higher rate of thyroid cancer (score 3) than nodules that were isoechoic or hyperechoic. The presence of coarse or rim calcifications increased the risk of cancer, and punctate microcalcifications resulted in a 3-fold increase in the incidence of malignancy (score 4).
DISCUSSIONThe aim of this paper was to evaluate the capacity of preoperative analysis of thyroid nodules using echographic studies associated with cytological evaluation to predict the presence of thyroid malignancy.
Population studies suggest that about 3% to 8% of asymptomatic adults have thyroid nodules,1,5–7 and this prevalence increases substantially with age.1 As determined by ultrasound examination, more than half of adults over the age of 50 may have a thyroid nodule.1,17 Ultrasound-guided fine-needle aspiration biopsy is the method of choice for determining the risk of malignancy.2,4 Also, a number of studies have also assessed various sonographic characteristics as predictors of thyroid cancer, including hypoechogenicity, solid composition, and absence of halo, irregular margins, and the presence of microcalcifications.17 In our institution, we perform a large number of USG-FNAB procedures for nodules larger than 10 mm, and the cytological results are expressed by a score, which, when in association with the sonographic score, results in an index score that might be helpful for the preoperative prediction of thyroid cancer.
As indicated in Figure 1, sonographic features alone do not reliably separate benign from malignant thyroid nodules. As recently reported by Frates et al,17 the more cystic a nodule is, the lower the likelihood of cancer. Hypoechoic nodules had a higher rate of malignancy than isoechoic or hyperechoic nodules. The presence of coarse or rim calcifications increased the likelihood of cancer almost 2-fold, when compared with the malignancy rate for nodules without calcification. Punctate microcalcifications increased the likelihood almost 3-fold. Well-defined or poorly defined nodule margins were not significantly associated with presence of thyroid cancer.17
Ultrasonographic classification of nodules. From top left, clockwise: grade I, a small round anechoic image (thyroid cyst); grade II, a complex nodule (like a sponge); grade II, multiple echonormal nodules; grade III, a hypoechoic solid nodule with regular border; grade III, cystic mass with solid projection from the cyst wall; and grade IV, a hypoechoic solid nodule with irregular border and microcalcifications.
To assess the likelihood of malignancy as indicated by sonographic characteristics, we combined both the results of ultrasonographic appearance with the cytological diagnosis after USG-FNAB. As shown in Table 1, in our cohort of 2468 nodules, grade III and IV sonographic patterns were detected in 1429 nodules. Of these, 261/1276 grade III nodules (20.4%) were cytologically classified as suspicious (13.7%) or malignant (6.7%), whereas 88/153 sonographically grade IV nodules (70.5%) were cytologically diagnosed as malignant, and 20/153 as suspicious (13.1%). The combined echographic and cytological score (index score) for patients who subsequently underwent total thyroidectomy is shown in Table 2.
Comparative studies of the echographic 4-tier system and the cytological findings
| Echographic | CYTOLOGY (USG-FNAB)* | |||
|---|---|---|---|---|
| Classification (n) | Benign | Indeterminated | Suspicious | Malignant |
| Grade I & II (1039) | 902 (87.0) | 96 (9.2) | 37 (3.6) | 4 (0.4) |
| Grade III (1276) | 743 (59.0) | 272 (21.3) | 176 (13.8) | 85 (6.7) |
| Grade IV (153) | 38 (24.8) | 7 (4.6) | 20 (13.1) | 88 (57.0) |
| 2,468 | 1,683 | 375 | 233 | 177 |
A total of 274 patients underwent thyroid surgery. Usually, patients with low scores2–4 are not routinely indicated for surgery unless compressive symptoms and recent growth are present. However, 64/274 patients (23.3%) were operated on the advice of their respective family-practice doctors, and malignancy was confirmed histologically in only 2 patients (3.1%). Patients with a combined score of 5 could be advised to follow a period of observation with or without L-T4 suppressive therapy. However, 51/279 (18.4%) of the patients with a score of 5 underwent surgery, and 11.7% (6/51) harbored thyroid malignancy. For patients with higher scores such as index 6, malignancy in the nodules was found in 50.8% (31/61), whereas nodules with index scores of over 7 had a 99% (97/98) incidence of thyroid cancer. Thus, sensitivity of the combined sonographic features and cytological results index scores was 94.1% and specificity was 77.5%, with a positive predictive value of 80.5% and a negative predictive value of 93.0%. The accuracy of this numeric scoring was 85.9%.
We conclude that the sonographic studies of nodules larger than 10 mm associated with USG-FNAB resulting in a cytological diagnosis comprise a better preoperative diagnosis tool for thyroid nodules as compared to each method individually. However, we were not able to secure a firm indication for score 5 nodules, although about 11% of those could be thyroid cancer. Moreover, nodules with an index score of 6 had a 50% percent chance of being associated with thyroid cancer; in this particular group, our tendency is to indicate thyroid surgery. Finally, a nodule score of 7 or more indicates mandatory thyroid surgery.
As seen in Table 1, about 15% of cytological results were classified as indeterminate and therefore not conclusive. The decision for indicating thyroid surgery is thus difficult unless sonographic characteristics suggestive of malignancy are present. However, recent data17 confirm that sonography cannot be used to confidently exclude malignancy, based on its negative predictive value. Thus, other methods and procedures may be helpful for a preoperative diagnosis.
Several studies have identified a role for color Doppler in the evaluation of thyroid nodules. Nodules with prominent central flow have an increased risk of malignancy.18–20 Thus, color Doppler sonographic studies may be helpful in identifying nodules that indicate thyroid surgery.
Another predictor of malignancy in thyroid nodules may be the presence of increasing serum levels of TSH at presentation. Regression analysis of TSH and the presence of malignancy has revealed significantly increased adjusted odds ratios for serum TSH greater than 5.5 mU/L as compared with TSH < 0.4 mU/L, principally in males, younger patients, and those with clinically solitary nodules.21 Thus, serum TSH levels may serve as an adjunct to USG-FNAB in predicting risk of malignancy in solitary nodules.
An alternative to the diagnosis of thyroid malignancy in selected thyroid nodules with indeterminate FNA cytology was proposed by Carpi et al.22 They introduced a strategy for improving the diagnosis of follicular lesions that is based on large-needle aspiration biopsy and galectin-3 expression analysis. Eighty-five thyroid specimens were obtained by large-needle (20-gauge needles) aspiration biopsy from thyroid nodules with indeterminate follicular cytology. Aspirate material was processed as a tissue microbiopsy to obtain cell blocks for morphological evaluation and galectin-3 expression analysis (purified monoclonal antibody to galectin-3). Among the 85 nodules tested, 14 galectin-3–positive tissues were discovered preoperatively (final histology after surgery, 11 thyroid cancers and 3 follicular adenomas). The final histology of the 71 galectin-3–negative cases revealed 70 benign proliferations and 1 follicular carcinoma. Sensitivity, specificity, and diagnostic accuracy of these integrated morphologic and phenotypic diagnostic approaches were 91.6%, 97.2%, and 95.3%, respectively. This methodology could potentially reduce unnecessary thyroid surgery even more so when associated with the results of echographic studies with color Doppler.
Lee and co-workers23 used a thallium-201 scan in evaluating thyroid nodules with indeterminate cytological diagnosis. Of the 51 nodules examined, 40 were benign and 11 harbored thyroid malignancy. Papillary carcinoma was diagnosed histologically in 6 patients, and follicular carcinoma in 5 patients. All malignant lesions had a grade 3 thallium uptake, whereas only 1 patient with a benign nodule exhibited a grade 3 uptake. Thus, sensitivity was 100%, specificity 75%, and accuracy 80%. They concluded that the dual-phase thallium-201 scan may be useful for detecting malignancy in the preoperative stage.
Recently, the value of FDG-PET was investigated not only for the follow-up of thyroid cancer patients but also for preoperative assessment of hypoechogenic/hypofunctioning nodules. An early study of 5 patients by Joensuu et al11 indicated a clearly increased FDG-PET uptake in 1 patient with anaplastic thyroid cancer and 1 with Hürthle cell carcinoma. In contrast with this study, Uematsu and et al12 demonstrated in 11 patients that all malignant nodules could be separated from benign ones using a standardized uptake value of FDG-PET higher than 5. Kresnik et al13 studied 43 patients (11 papillary TC, 3 follicular TC, 2 anaplastic cancer, 11 microfollicular adenomas, 10 oxyphillic adenomas, 2 macrofollicular adenomas, and 4 goiters). All patients with TC and oncocytic adenomas had increased FDG uptake. Using a standardized uptake value (SUV) threshold of 2 for differentiating benign from malignant nodules, sensitivity and specificity were 100% and 63%, respectively. More recently, Mitchell et al14 used FNAB and FDG-PET before surgery and documented that 9 of 15 malignant lesions were FDG positive (sensitivity 60%) and 30 of 33 benign lesions were FDG negative (specificity 91%). The authors concluded that FDG-PET has a relatively high negative predictive value (83%) for malignancy.
In a recent review, Lind and Kohlfurst15 reported that in a subgroup of 24 patients with a cytological diagnosis of follicular proliferation, FDG-PET was able to differentiate between follicular adenoma and follicular carcinoma. Thus, in case of indeterminate cytology, FDG-PET seems to be the method of choice for deciding whether to go ahead with thyroid surgery or, alternatively, whether a wait and watch strategy should be recommended. Similar results were obtained by Sebastianes et al16 in patients with nodules larger than 20 mm and indeterminate cytology results. Recently, Stabenow et al 24 suggested that angiogenesis is also a potential indicator for papillary thyroid carcinoma, but this has not been investigated in this study.
In conclusion, the use of an index score based on echographic studies of thyroid nodules and the results of USG-FNAB cytology may improve our preoperative diagnosis of thyroid cancer in nodules larger than 10 mm. Color Doppler echography may add to the sensitivity of the index score. Elevated serum TSH concentrations (> 5.5 µU/mL) have been shown to be an independent predictor of thyroid malignancy. Large-needle aspiration biopsy derived cell blocks and galectin-3 expression analysis have led to a better preoperative selection of patients with a cytological diagnosis of follicular thyroid proliferation. Finally, FDG-PET scan is a promising methodology for deciding on the need for thyroid surgery for nodules with indeterminate cytology. Most of the unnecessary surgery for benign thyroid nodules may be avoided when those methods are employed, with a consistent reduction of hospitalization and social costs to the health systems of many countries.
This study was partially funded by grants from the State of Sao Paulo Research Foundation (FAPESP) and Instituto da Tiróide (Sao Paulo, Brazil). We gratefully acknowledge the continuous help of the Thyroid Unit staff Maria Silvia Cardia and Jacyra M. Lima. We also thank Andrea G. Fernandes and Margarida Lemos for impeccable secretarial services. We are grateful to Fernando Sebastianes and Maria Adelaide Albergaria Pereira for the FDG-PET scans information.