The Personal Health Scale is a concise instrument for comprehensive culture-informed and self-rated assessment of general health status and well-being. It is composed of 10 questions that appraise different health dimensions collated from the international literature, including aspects ranging from somatic and psychological domains to social functioning and insight.
PURPOSE:In this investigation, results of a study conducted in Southern Brazil to test and validate the Portuguese version of the Personal Health Scale (PHS-Pt) are presented.
METHOD:This study analyzes data from a sample of 120 Brazilian volunteers (90 patients and 30 health care professionals). All patients completed the Portuguese version of the Personal Health Scale under a minimal guidance by trained examiners, who followed standardized instructional procedures.
RESULTS:The internal consistency of the PHS-Pt attained a Cronbach's a of 0.75 among patients and of 0.69 among health care professionals. The test-retest reliability correlation coefficient yielded a score of 0.82. Furthermore, the PHS-Pt was able to detect a significant discriminating validity between the 2 evaluated samples (P < .001).
CONCLUSIONS:The original English version of the Personal Health Scale was successfully adapted to Portuguese as methodologically demonstrated herein. The PHS-Pt constitutes a reliable and trustworthy research instrument for evaluating health status in Brazil, since it is appropriately designed to distinguish different groups of volunteers regarding their health status.
A Escala de Saúde Pessoal é um instrumento conciso para a avaliação do estado geral de saúde e bem-estar que considera os aspectos culturais e a visão pessoal do entrevistado. Ela é composta por 10 questões que avaliam diferentes dimensões de saúde obtidas a partir da literatura internacional, incluindo aspectos que variam de domínios somáticos e psicológicos até juízo critico e funcionamento social.
OBJETIVO:Nesta investigação, os resultados de um estudo conduzido no Sul do Brasil para testar e validar a versão em português da Escala de Saúde Pessoal são apresentados.
MÉTODO:Este estudo analisa dados de uma amostra de 120 voluntários brasileiros (90 pacientes e 30 profissionais da saúde). Todos pacientes completaram a versão em português da Escala de Saúde Pessoal sob orientação mínima de examinadores treinados que seguiram procedimentos padronizados de instrução.
RESULTADOS:A consistência interna da PHS-Pt atingiu um índice á de Cronbach de 0.75 entre pacientes e de 0.69 entre profissionais da saúde. O coeficiente de correlação da validade teste-reteste indicou um escore de 0.82. Ademais, a PHS-Pt foi capaz de detectar uma significativa validade descriminante entre as duas amostra avaliada (P < .001).
CONCLUSÕES:A versão original em língua inglesa da Escala de Saúde Pessoal foi adaptada com sucesso para o idioma português como demonstrado metodologicamente neste estudo. A PHS-Pt constitui um instrumento de pesquisa confinável e fidedigno para avaliar o estado de saúde no Brasil, já que é apropriadamente estruturada para distinguir diferentes grupos de voluntários de acordo com seus estados de saúde.
During the latter part of the 20th century, there was a heightened appreciation of the subjective expressions of patients.1 The field of health status and quality of life measurement has been evolving as a formal discipline with structured theoretical foundations and specific methodology for more than 30 years.2 The concepts of health status, well-being, and quality of life started to be conceived as researchable topics in the mid-1970s, when these constructs were often encompassed among psychosocial correlates of well-being and physiological factors.3,4 In the late 1980s, some authors adopted health screening procedures for examining the limitations imposed by the disease process on patients’ well-being and social functioning.5–8 It was then understood that general health status is amenable to assessment and measurement, and henceforth, clinicians and researchers started to develop psychometric tools to evaluate the impressions of a given patient about his own health condition. The concept of personal health relates to the perception each individual has of his own health status.
Although the concept of health has been subject to cultural and historical adjustment, according to the World Health Organization, health can be defined as a state of complete physical, mental, and social well-being.9–11 Yet, there is a current tendency to reexamine the conceptual boundaries of health in order to include additional elements such as socio-cultural conditions as well as factors contributing to mental and physical health, which ideally would transcend the rather circumscribed dichotomy of the health-disease process.12 It is currently acknowledged that efforts to investigate and evaluate quality of life, social functioning, health status, and well-being are valid enterprises within clinical and research contexts.13
Clinicians and policymakers now agree on the importance of measuring both general and health-related quality of life.14 The growing interest in assessing health status in the general population has spurred a demand for specific questionnaires to measure this construct within a reliable and valid framework. Among other applications, it has been demonstrated that general health questionnaires are useful tools for identifying episodes of emotional distress in general practice consultations.15 Health questionnaires are divided into 2 distinct domains of analysis, which are related to generic or disease-specific health measures.16 General health instruments inquire about health in a broad sense, whereas disease-specific questionnaires assess narrower aspects of life related to a specific problem, function, or manifestation of an underlying disease process.17
Health status questionnaires provide parameters for monitoring the impact of disease activity as well as the effect of therapeutic interventions. Health assessment tools may also provide important information about the need for medical assistance as well as the degree of disability of a given patient. Various generic health scales and questionnaires have been developed and adapted to an array of languages and cultures, including the Short Form 36-item Health Survey (SF-36), the Nottingham Health Profile (NHP), the Stanford Health Assessment Questionnaire (HAQ), the Modified Health Assessment Questionnaire (MHAQ), the EuroQol (EQ), and the Short Form 12-item Health Survey Questionnaire (SF-12).18–23
Due to the increment in the number of multinational and multicultural research projects, there has been a proportional increase in the number of studies designed to test and adapt a series of health status instruments to different countries and languages.24–26 Most of the questionnaires were originally developed in English-speaking countries. Presently, several health status instruments are available in different languages, and some have been tested and validated in numerous countries.27 Nevertheless, the methodological details of translation and adaptation of questionnaires originally developed in English for future use in other countries have received surprisingly little attention.28 It is now a consensus that, when tested across different cultures, measures must not only be well translated linguistically, but also be well adapted culturally in order to guarantee the content validity of the instrument.24,29–31
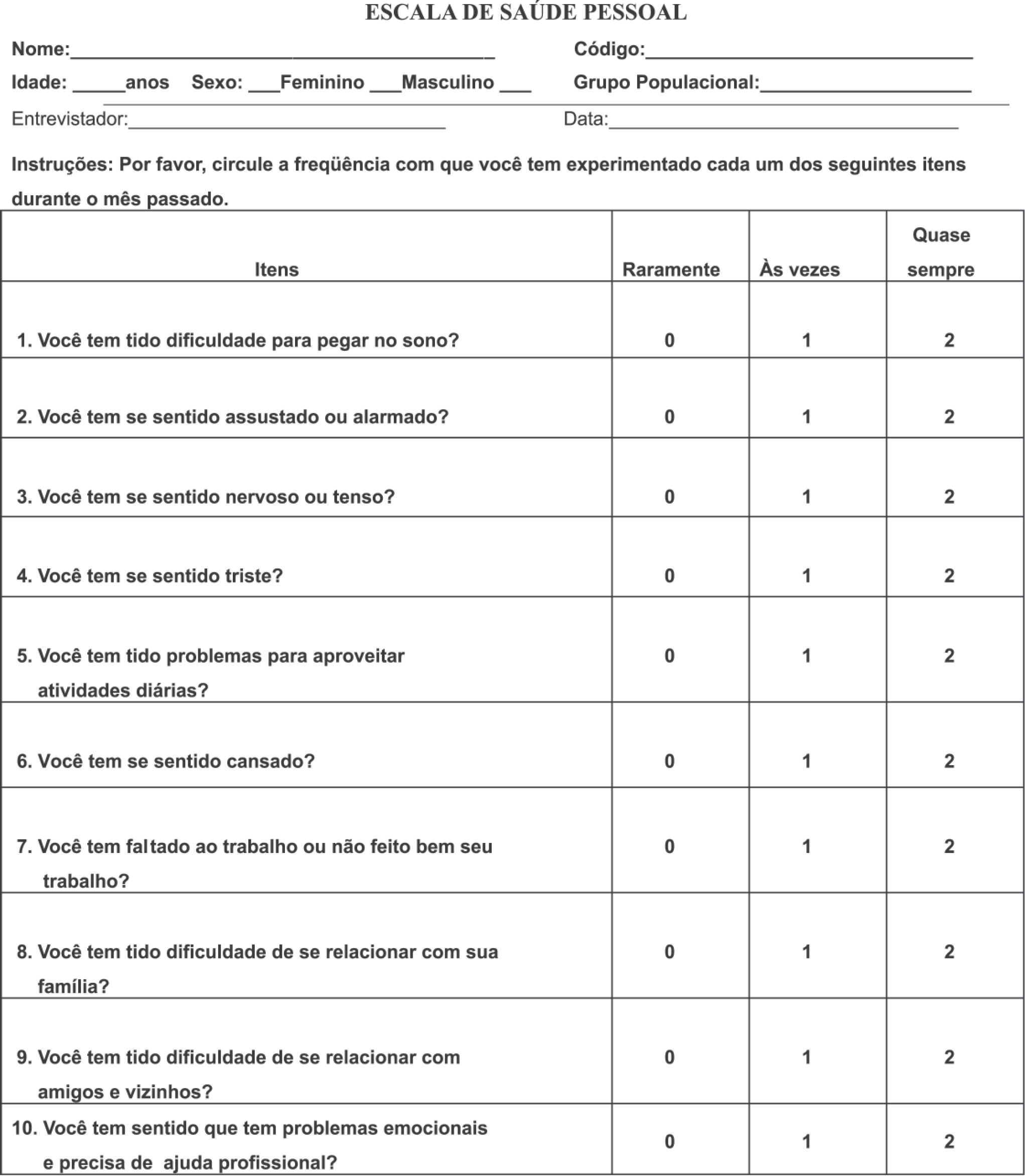
The Personal Health Scale (PHS) is a unidimensional questionnaire designed to measure the construct of personal health status from a user perspective. It contains 10 items that were obtained through a critical review of the international literature. The Personal Health Scale is an ordinal scale that measures the frequency of 10 dimensions and rates each one numerically from 0 to 3. The score magnitude of each domain parallels the frequency of each correlated dysfunction or symptom, so that the higher the overall score of the instrument, the lower the personal health status.
In the development of the PHS, particular attention has been paid to multicultural issues, so that specific conditions presented by immigration groups are surveyed in the instrument.30 Different versions of the PHS have been already validated in an array of languages.32–34 In this investigation, results of a study conducted in Brazil to test and validate the Portuguese version of the Personal Health Scale (PHS-Pt) are presented.
The main objective of this report was to present details of the application of the PHS-Pt in a sample of Brazilian volunteers in the city of Caxias do Sul, Southern Brazil. Furthermore, the aim of this study was to evaluate empirically the feasibility, internal structure consistency, reliability, and discriminant validity of the PHS-Pt in order to establish the validation of this instrument for investigational purposes in Brazil. It is concluded that the PHS-Pt was well understood by research volunteers and was effective for significantly differentiating between 2 discordant samples according to their purported health conditions. Figure 1 shows the PHS-Pt.
METHODSSubjectsThe study investigated 2 samples of adult volunteers: one included 90 patients (30 from inpatient psychiatric units, 30 from outpatient facilities, and 30 from general hospital units), and the other comprised 30 health care professionals from the same general hospital. The psychiatric units are located at Paulo Guedes Clinic, which is a 350-bed tertiary care psychiatric hospital. Both the general hospital and the outpatient clinics are located on the main campus of the University of Caxias do Sul. All 3 health care services are also graduate training facilities associated with UCS and located in the city of Caxias do Sul in Southern Brazil.
All patients who volunteered to participate in this investigation were assisted via the Brazilian public health system (SUS). Health care professionals who voluntarily participated in this investigation were actively working nurses and nurse assistants who denied having major health problems during a clinical interview prior to their enrollment in the study. All professionals were employed under conventional working conditions and professional agreements at the UCS general hospital. Portuguese was the native language of all volunteers.
INFORMED CONSENTThis study was endorsed by institutional Ethics and Research Committee of the University of Caxias do Sul. All volunteers signed a consent form to declare a voluntary agreement with all procedures implicated in this project. Taking into account that a substantial fraction of the sample population was illiterate or semi-illiterate, all patients completed the PHS-Pt under minimal guidance by trained examiners, who followed standardized instructional procedures.
ProceduresThe PHS was translated into Portuguese taking into account semantic, idiomatic, experiential, cultural, and conceptual equivalence between the source and the target instruments.31 Two investigators proficient in both Portuguese and English developed the final Portuguese version of the PHS. Each investigator conducted the translation and adaptation in one direction, from one language to the other (translation and back-translation). The final adapted version of the instrument was established by a committee of specialists, by taking into comparison both the translation and back-translation of the instrument. This committee consisted of professionals fully cognizant of the subject under investigation. Many of them were versed in both languages. The various drafts of the PHS, in each language, were progressively improved by using relevant information obtained from a series of applications of the questionnaire to various samples of patients and professionals.32–35
ANALYSISEvaluation parameters and statistical analysis included the following factors: feasibility (time of completion and ease of use); internal structure (internal consistency and factorial structure); test-retest reliability (an interval of 3-7 days apart), and discriminant validity, as determined by comparing the mean scores of 2 samples with presumably different levels of health status. Analysis of variance (ANOVA) followed by post hoc analysis (Tukey B) were applied exclusively to compare different subgroups separately.
RESULTSIn the sample of patients, 45% of the volunteers were men, and ages ranged from 20 to 70 years, with a mean of 47.7 years. In the sample of health professionals, 5% were men, and ages ranged from 20 to 59 years, with a mean of 37 years. All health professionals were actively working during the investigational period.
Feasibility ResultsThe average time that volunteers from the sample of patients took to complete the questionnaire was 3.8 minutes, while volunteers from the sample of health professionals completed the questionnaire in 2.8 minutes. Table 1 presents the distribution of the variable “ease of use” for the 2 samples, as perceived by volunteers and interviewers. The large majority of patients and their respective interviewers considered the questionnaire as “somewhat easy” or “very easy” to complete. All of the health professionals and their respective interviewers considered PHS-Pt as “somewhat easy” or “very easy” to complete.
Ease of use of the Portuguese version of the Personal Health Scale, according to the perceptions of volunteers and interviewers in groups of patients and health professionals.
| As Perceived by Volunteer | As Perceived by Interviewer | |||
|---|---|---|---|---|
| Degrees of Ease of Use | Patients | Professionals | Patients | Professionals |
| Very easy | 51,2% | 43,3% | 43,3% | 86,6% |
| Somewhat easy | 36,6% | 56,7% | 46,6% | 13,3% |
| Somewhat difficult | 11,1% | 0% | 8,8% | 0% |
| Very difficult | 1,1% | 0% | 1,1% | 0% |
The internal consistency of the PHS-Pt (correlation of the items to the total score) attained a Cronbach's a of 0.75, when administered to the sample of patients, and of 0.69, when administered to the sample of professionals (out of a maximum of 1.00 in each case). The factor analysis (main components) of the 10 items of the PHS-Pt, on the combined sample of 120 patients and health professionals, yielded 1 factor, which accounts for a substantial 32.66% of item variance. The results of the factor analysis are represented in Table 2. These results demonstrate adequate homogeneity and coherence of all items included in the scale, which represents an integrated concept of health status.
Factorial structure of the Portuguese version of the Personal Health Scale in a combined sample of patients and of health professionals.
| Items | Factor |
|---|---|
| 1. Have you had difficulty in falling asleep? | 0,73 |
| 2. Have you felt frightened or alarmed? | 0,73 |
| 3. Have you felt nervous or tense? | 0,71 |
| 4. Have you felt sad? | 0,70 |
| 5. Have you had trouble enjoying your daily activities? | 0,73 |
| 6. Have you felt tired? | 0,76 |
| 7. Have you failed to do or mismanaged your work? | 0,75 |
| 8. Have you had difficulty in relating to your family? | 0,74 |
| 9. Have you had difficulty in relating to friends and neighbors? | 0,74 |
| 10. Have you perceived that you have emotional problems and that you need professional help? | 0,73 |
The test-retest reliability analysis was conducted for each item separately. Most of items yielded results of 0.80 or higher. The average score of the test-retest reliability analysis, considering the totality of items, yielded a score of 0.82.
Discriminant Validity ResultsDiscriminant validity analysis of the PHS-Pt was conducted for distinct groups of volunteers in the sample. A significant difference between the sample of patients and the sample of health professionals was demonstrated for most of the items in the scale when analyzed separately. A significant difference (P < .001) between the means of the instrument's final scores in the groups of patients (7.38) and health professionals (4.90) was observed, which attests to the substantial discriminant validity of the PHS-Pt.
The means of questions 1, 4, 5 and 9 were not significantly different between patients and health workers. These questions are related to sleep, mood, daily tasks, and interpersonal relationships. Analysis of variance (ANOVA) followed by post hoc analysis (Tukey B) also did not reveal any significant difference between the means when these specific questions were compared among the 4 subgroups.
According to a Relative Operating Characteristic (ROC) analysis, which considers both sensitivity and specificity factors, the best cut-off value was a score of 6 (AUC = 0.686; SD = 0.51; 95% CI = 0.585-0.786), which accounts a sensitivity of 73.3% and a specificity of 70%. A ROC curve is obtained by plotting sensitivity against the false-positive rate for all possible cut-off points of the screening instrument. The curve represents the performance of the instrument in discriminating between ‘cases’ and ‘noncases’ across the total spectrum of morbidity, and the area under the ROC curve (AUC) can be used as an index of the discriminating ability of a screening instrument.36
Table 3 shows a 2 X 2 table for a variety of values for case/noncase threshold. Sensitivity and specificity figures as well as positive and negative predictive values according to the above-mentioned cut-off score are also presented on Table 3. The limitrophe scores of 5 and 7 were also tested but presented unfavorable outcomes compared to the proposed cut-off of 6.
Values for cases and non-case of the Portuguese Version of the Personal Health Scale according to the cutoff score of 6.
| Test | Patients | Controls | Total |
|---|---|---|---|
| PHS-Pt e 6 | 66 | 9 | 75 |
| PHS-Pt < 6 | 24 | 21 | 45 |
| Total | 90 | 30 |
Sensitivity = 0,733; Acuracy = 0,725; Positive Preditive Value = 0,888; Specifity = 0,7; Negative Preditive Value = 0,466
The PHS-Pt was well accepted by patients and health professionals alike. The questions were answered with relative ease and rapidity (less than 4 minutes to complete), which demonstrates the ease of use of the instrument. As observed elsewhere, questionnaires that investigate health status and quality of life in multiple domains and with a larger number of questions tend to take longer than the PHS-Pt to be completed.37–38
The internal consistency of the PHS-Pt, as indicated by the results of the coefficients of Cronbach, was satisfactory for patients and health professionals alike, which demonstrates that the instrument coherently investigates the construct of health status as measured uniformly by its items. The validation study of the Latino version of the PHS found similar results. The test-retest reliability of PHS-Pt is demonstrated by a substantial correlation (r = 0.82) between questionnaires completed from 3 to 7 days after the initial interview. In order to prevent a major influence caused by the natural course of a given disease and/or the symptomatic fluctuation of the clinical state of patients on our results, we aimed at minimal test-retest intervals.
The discriminant validity was demonstrated by a significant difference between the means of the final scores in the 2 different groups. Health workers were actively working during the investigational period and therefore were not subject to any frank disability. Compared to volunteers from the inpatient units (psychiatric and general hospital) and to volunteers from outpatient facilities, health workers presumably presented a lesser level of disability due to mental or other clinical and surgical disorders. This hypothesized difference was properly detected by the PHS-Pt, which confirms the adequacy of the instrument to reliably differentiate distinct populations according to a significant difference in their health statuses.
Some questions (1, 4, 5 and 9) did not reveal a significant difference between health workers and patients. Sleep and mood may not be impaired in outpatient volunteers without known psychiatric disorders; health workers may complain of time constraints to fully complete the requirements of their daily activities; and poor interpersonal aptitude may convey a personality trait, which may occur regardless of any physical ailment. These areas, though, may contribute to the homogeneity of the Personal Health Scale altogether.
In a series of studies conducted in New York City, the proposed cut-off score to determine the likelihood of having a mental disorder was found to be a total score of 9 or more in the validation study of the English version of PHS, whereas the proposed cut-off scores among Spanish-speaking and Chinese-speaking people in New York City were 7 and 6 respectively. Therefore, our results indicate that the cut-off point attained in the sample of Portuguese-speaking volunteers in Southern Brazil (6 or more) is within reasonable boundaries.
This study might have identifiable limitations. There is a gender disparity between patients and health professionals, in that the latter group had a smaller proportion of men. This might be related to the fact that female registered nurses and nurse assistants still outnumber their male counterparts in this region of Brazil. No gender-specific recruitment strategy was conducted in any of the research samples. Although this approach could prevent gender disproportions, it could also artificially affect voluntary entry to the research protocol. There was a 10-year difference in the mean age of the 2 groups. Plausibly, the subsample of professionals had a lower mean age due to the retirement cap after 25 years of professional activity, a limit that obviously does not apply to patients. Additional studies encompassing different areas in the country might be necessary to generate a more representative picture of both regional and nationwide health standards among distinct samples of patients and the general population.
This study demonstrates that the original English version of the Personal Health Scale was successfully adapted to Portuguese as methodologically demonstrated herein. PHS-Pt constitutes a reliable and trustworthy research instrument for evaluating health status in Brazil, since it is appropriately designed to distinguish different groups of volunteers according to their health status. Furthermore, PHS-Pt can be conveniently used to assess health status, since it is completed both easily and quickly.
We kindly thank Prof. Carlos Pinnent, Prof. Juliana Favero Constanzi, Prof. Celso Piccoli Coelho, Dr. Katia Foresti and Dr. Gloria Johnson for their valuable assistance during distinct phases of this study. This study was partially supported by grant # 000605-25.00/03-8 from the Secretaria de Ciência e Tecnologia do Estado do Rio Grande do Sul and by grant # 200498/00-2 from the Conselho Nacional de Desenvolvimento Científico e Tecnológico, Brazil.