Ischemia reperfusion injury is partly responsible for the high mortality associated with induced myocardial injury and the reduction in the full benefit of myocardial reperfusion. Remote ischemic preconditioning, perconditioning, and postconditioning have all been shown to be cardioprotective. However, it is still unknown which one is the most beneficial. To examine this issue, we used adult male Wistar rat ischemia reperfusion models to compare the cardioprotective effect of these three approaches applied on double-sided hind limbs.
METHODS:The rats were randomly distributed to the following five groups: sham, ischemia reperfusion, remote preconditioning, remote perconditioning, and remote post-conditioning. The ischemia/reperfusion model was established by sternotomy followed by a 30-min ligation of the left coronary artery and a subsequent 3-h reperfusion. Remote conditioning was induced with three 5-min ischemia/5-min reperfusion cycles of the double-sided hind limbs using a tourniquet.
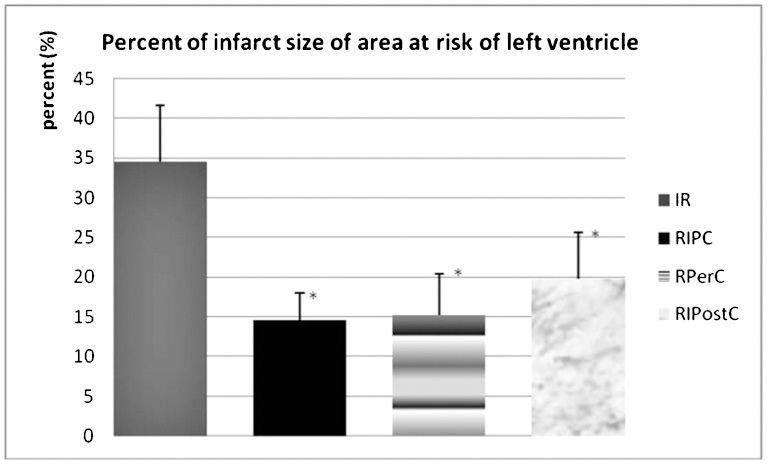
RESULTS:A lower early reperfusion arrhythmia score (1.50±0.97) was found in the rats treated with remote perconditioning compared to those in the ischemia reperfusion group (2.33±0.71). Meanwhile, reduced infarct size was also observed (15.27±5.19% in remote perconditioning, 14.53±3.45% in remote preconditioning, and 19.84±5.85% in remote post-conditioning vs. 34.47±7.13% in ischemia reperfusion, p<0.05), as well as higher expression levels of the apoptosis-relevant protein Bcl-2/Bax following global (ischemia/reperfusion) injury in in vivo rat heart models (1.255±0.053 in remote perconditioning, 1.463±0.290 in remote preconditioning, and 1.461±0.541 in remote post-conditioning vs. 1.003±0.159 in ischemia reperfusion, p<0.05).
CONCLUSION:Three remote conditioning strategies implemented with episodes of double-sided hind limb ischemia/reperfusion have similar therapeutic potential for cardiac ischemia/reperfusion injury, and remote perconditioning has a greater ability to prevent reperfusion arrhythmia.
Currently, coronary artery disease (CAD) is a leading cause of death among adults. The timely induction of coronary reperfusion through thrombolytic therapy or primary percutaneous coronary intervention (PCI) represents the most effective strategy to reduce myocardial infarct size. However, ischemia/reperfusion injury (IRI) (1), which paradoxically induces myocardial injury and reduces the full benefit of myocardial reperfusion, may be partially responsible for the high mortality (2) and incidence of cardiac failure following acute myocardial infarction (AMI) (3), which remain as high as 10% and 25%, respectively, at one year.
Ischemic preconditioning has been recognized as a major cardioprotective phenomenon for many years (4). In recent years, it has been found that transient ischemia of a remote organ or limb, which is termed remote ischemic preconditioning (RIPC), could generate protection for the organ subsequently challenged by lethal ischemia (5). The discovery of this phenomenon may obviate the need to directly intervene in the heart to achieve cardioprotection.
Although RIPC has been clinically successful in attenuating the physiological adverse effects of serial balloon inflations during percutaneous transluminal coronary angioplasty (6), its use as a clinical strategy to attenuate the undesired pathophysiological consequences of IRI is limited by the failure to predict the onset of ischemia. Kerendi et al. (7) demonstrated that transient renal ischemia/reperfusion (IR) at the end of a prolonged episode of myocardial ischemia reduced the resultant myocardial infarction size. Subsequently, Andreka et al. (8) found that using a more practical stimulus of transient limb ischemia, which was applied following the induction of myocardial infarction (remote ischemic postconditioning [RIPostC]), also rendered a protective effect. Moreover, RIPostC can be used in humans and appears to be as effective as preconditioning (9). It was concluded that both methods could provide an equally protective effect to the vascular endothelium.
By using a porcine model, Schmidt et al. (10) demonstrated that brief intermittent limb ischemia also delivered significant protection during the evolution of myocardial infarction. The authors then introduced a new cardioprotection strategy called remote ischemic preconditioning (RPerC). In their study, four 5-min ischemia cycles alternated with 5-min reperfusion were applied to the limb during a 40-min period of occlusion of the left anterior descending coronary artery. Consequently, reduced myocardial infarction, well preserved global systolic and diastolic function, and protection against arrhythmias were observed during the phase of myocardial reperfusion. Our study (11) also showed that three 5-min ischemia cycles combined with 5-min of reperfusion applied to the double-sided hind limbs during the 30-min occlusion of the left coronary artery, which was followed by 180 min of reperfusion, was able to induce cardioprotection in rats.
Based on the timing of the transient limb ischemia, protective strategies are classified as remote preconditioning, perconditioning, and postconditioning. To our knowledge, all three strategies have the potential to provide cardioprotection. However, it remains unknown which of the three is the most effective. Therefore, the aim of this study was to compare the cardioprotective effect of the three strategies. In doing so, we established myocardial I/R models in rats and evaluated the protection of RIPC, RPerC, and RIpostC against myocardial injury when applied to double-sided hind limbs.
METHODSAnimals and surgical preparationsAll animals were treated according to the principles stated in relevant Chinese stipulations on animal experiments and in conformity with the Guide for the Care and Use of Laboratory Animals published by the United States National Institutes of Health. Furthermore, the experimental protocol was approved by the Institutional Animal Care Committee and Ethical Review Committee of Wuhan general hospital of Guangzhou command. Adult male Wistar rats (Laboratory Animal Center, Hubei Center for Disease Control and Prevention, PR China) weighing 250-410 g (340±59 g) were used as experimental animals, and surgical preparations were adapted from procedures that we have previously described (12). Specifically, general anesthesia was induced with an intraperitoneal injection of 10% chloral hydrate at a dose of 3 ml.kg-1. Subsequently, intubation of the rats was performed through an incision of the trachea, and ventilation was performed at 3-4 ml.kg-1 per minute with atmospheric air. The chest was opened through a lower sternal incision. Following pericardiotomy, a prolene 6-0 suture (Johnson & Johnson, SanLorenzo, Puerto Rico, USA) was placed under the left coronary artery (LCA), and a slipknot was tied to establish reversible coronary artery occlusion. Successful occlusion and reperfusion were identified as described by Johns and Olson (10). Importantly, the animals were anticoagulated with sodium heparin (150 U/kg-1) prior to the LCA occlusion. A 24-gauge catheter was delivered into the left ventricle (LV) chamber, and the changes in ventricular pressure were monitored continuously. Anesthesia was maintained using chloral hydrate (1 ml.min-1.kg-1). At 180 min post-reperfusion, the area of the left ventricle at risk was analyzed with an injection of 2 ml of 1% Evan’s blue (Sigma, USA) into the LV after the left coronary artery had been ligated. Finally, cardiac arrest was established with an intracardiac injection of 10% KCl, and the hearts were immediately excised followed by the removal of the right ventricular free wall from the ventricular mass. Additionally, the LV was cut into 1-2 mm slices perpendicular to the septum from the apex to the base.
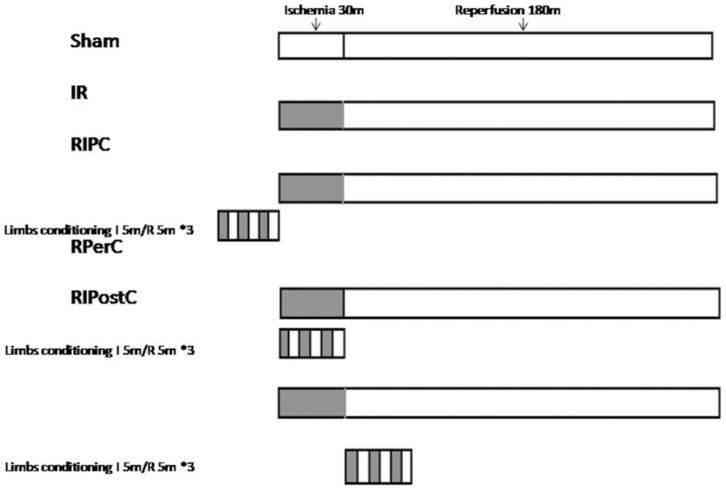
Experimental protocolsThe rats were randomly distributed to the following five groups (Figure 1): 1) the sham group (n = 8) was treated as the control group and did not undergo occlusion of the coronary artery; 2) the IR group (n = 12) underwent 30 min of ischemia by occluding the LCA followed by 180 min of reperfusion by reopening the LCA; 3) the RIPC group (n = 12) was treated in the same manner as the IR group with three 5-min ischemia cycles applied to the limbs by tying the double-sided hind limbs followed by 5-min of reperfusion by untying them ahead of cardiac ischemia; 4) the RPerC group (n = 12) was treated like the RIPC group, but remote conditioning was applied at the start of the cardiac ischemia; and 5) the RIPostC group (n = 12) was treated in the same manner as the RIPC group, but remote conditioning was applied at the beginning of the cardiac reperfusion.
The remote stimulus was delivered via tourniquet blockage of blood flow to the double-sided hind limbs and featured three 5-min cycles of blocked flow followed by 5 min of the resumption of blood flow. Circulatory arrest in the limbs was identified by observing the empurpled limb skin and via vascular Doppler. This method has been developed and standardized in a previous study employing RPerC (13,14); in that study, this method was shown to be reliable and consistent in blocking blood flow in the leg.
Analysis of cardiac rhythmFor the duration of this experiment, no prophylactic antiarrhythmic drugs were administered, and ventricular arrhythmia caused by sustained hemodynamic collapse was treated with interrupted slaps. In addition, every episode was documented, and the arrhythmic scoring system described by Curtis (15) was used for scoring based on the cardiac rhythm for analysis.
Assessment of ventricular functionThe LV chambers of all the rats were cannulated with 24-gauge catheters for measuring the hemodynamic parameters, and the catheters were connected to fluid-filled pressure transducers. Real-time hemodynamic data, including LV peak systolic pressure (LVSP) and end-diastolic pressure (LVEDP), as well as the maximum and minimum first derivative of LVSP (±dP/dtmax), were recorded continuously using chart 4.0 software and a PowerLab physiological recorder (AD Instrument, Australia). The entire time course of the IRI was documented as a digital file.
Determining the at-risk area and infarct sizeLeft ventricle slices were incubated in 1% pH 7.4 triphenyltetrazolium chloride (Sigma, USA) for 30 min at 37 °C and then fixed in 10% formaldehyde solution for 24 h and photographed. This procedure was followed by planimetric quantification using Photoshop software 8.0 in a blind fashion. The area at risk (AAR) represented the viable area, and the necrotic area was quantitatively expressed as a percentage of the left ventricle (AAR/LV), while the area of necrosis (AN) (infarct size) was expressed as a percentage of the AAR (AN/AAR).
Analysis of Myocardial Apoptosis-Relevant ProteinsHeart tissue from the AAR was collected at the end of reperfusion to measure the Bcl-2 and Bax expression ratios. The expression of apoptosis-relevant proteins, Bcl-2 and Bax, were determined using the histochemical immunity method. Staining was performed on heart tissue slices randomly selected from each group by applying a commercially available kit (Roche, Germany) according to the manufacturer’s instructions. The tissue sections were examined microscopically at ×400 magnification, and the images were captured. The positive distribution rate was analyzed using the HPIAS-1000 color graphic analysis system, and based on this result, the ratio of Bcl-2/Bax expression was calculated.
Calculations and StatisticsAll of the data were expressed as means ± SE unless otherwise stated, and statistical analysis was performed with SPSS 13.0 statistics software for the Windows system (SPSS, Chicago, IL, USA). For all of the hemodynamic parameters, comparisons were made by applying a one-way ANOVA for repeated measurements, and individual comparisons were also examined with a paired Student's t-test with the Bonferroni correction when required. The extent of the MI was corrected for the area at risk and is expressed as a percentage. In all cases, p<0.05 was considered statistically significant.
RESULTSMortality and exclusion of animalsFifty-six rats with successful ligation and relaxation of the coronary arteries were initially included in the study. Among these, four died of anesthetic accidents, and five died of ventricular fibrillation during myocardial ischemia. Thus, complete data sets were obtained from the remaining 47 rats.
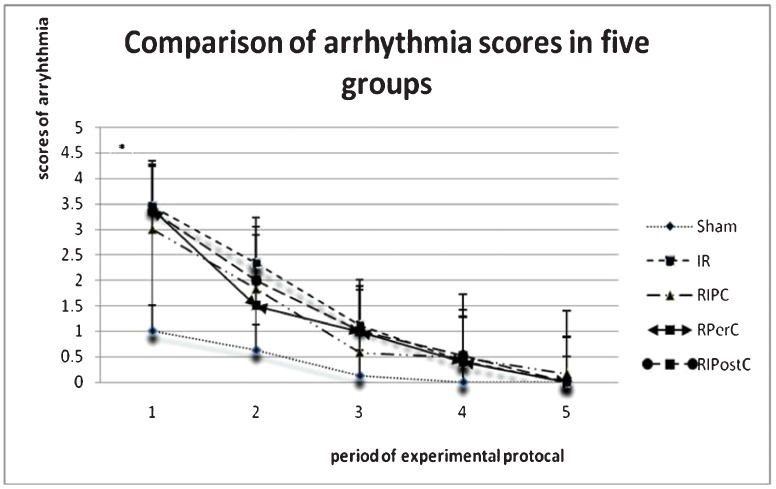
Cardiac rhythm dataIn comparison with the sham group, ventricular arrhythmia occurred much more frequently during both of the periods of cardiac ischemia and reperfusion in all of the other four groups, whereas ventricular tachycardia, ventricular bigeminy, and trigeminy were commonly observed among all the groups. During the early reperfusion period, there was no significant difference between the IR group, the RIPC group or the RIPostC group. However, the arrhythmic score of the RPerC group was significantly lower than that of the IR group (p = 0.043, Figure 2).
Hemodynamic dataDuring both the periods of ischemia and reperfusion, there were significant changes observed in the IR group and the RIPC group compared to the data at baseline. Individual group data are shown in detail in Table 1. The changes reflect significant differences among these groups at some time points.
Hemodynamic data obtained from each group of rat models at different time points.
| Hemodynamic data | Time point | Baseline | 30 min after ischemia | 30 min after reperfusion | 60 min after reperfusion | 120 min after reperfusion | 180 min after reperfusion |
|---|---|---|---|---|---|---|---|
| LVSPmax(mmHg) | Sham | 139.2±18.5 | 133.6±19.8 | 136.4±28.4 | 125.2±24.2 | 115.7±23.2 | 112.7±26.7 |
| IR | 126.4±18.2 | 100.5±19.7∗∗ | 115.9±24.9 | 113.7±26.0 | 103.2±27.4 | 90.2±29.2 | |
| RIPC | 135.5±23.2 | 110.4±44.2 | 101.6±33.8 | 104.1±36.7 | 92.7±40.4 | 86.5±34.6 | |
| RPerC | 148.9±31.4 | 113.7±26.3 | 114.7±27.7 | 109.0±19.4 | 108.8±26.2 | 95.1±30.1 | |
| RIPostC | 148.9±19.9 | 107.3±16.4 | 114.1±11.7 | 113.8±12.7 | 111.9±19.1 | 106.0±19.6 | |
| LVEDPmin(mmHg) | Sham | (-7.5)±7.9 | (-3.1)±8.3 | (-2.1)±9.9 | (-8.5)±10.2 | (-5.1)±8.4 | (-4.0)±6.9 |
| IR | (-6.9)±7.3 | (-5.1)±5.7 | (-3.9)±6.8 | (-5.0)±6.3 | (-3.8)±6.8 | (-1.9)±5.7 | |
| RIPC | (-11.0)±3.7 | (-0.4)±7.5 | 4.6±7.8∗ | 1.7±6.5 | 2.1±3.7 | 3.2±3.7 | |
| RPerC | (-9.3)±9.3 | (-0.8)±9.4 | (-3.1)±7.5 | (-1.9)±7.5 | (-1.0)±6.6 | 0.3±4.8 | |
| RIPostC | (-9.0)±3.1 | (-4.1)±3.6 | (-0.9)±2.3 | (-1.0)±3.4 | 0.2±4.5 | 0.1±4.6 | |
| +dp/dtmax(mmHg/s) | Sham | 5,366.1±1,557.9 | 4,806.4±1,722.6 | 5,383.9±1,988.2 | 5,195.7±1,902.7 | 4,069.3±1,111.9 | 3,808.8±1,237.2 |
| IR | 5,421.1±924.5 | 2,849.9±1,188.8 | 3,963.9±978.7 | 3,998.4±978.7 | 3,477.9±1,210.9 | 2,736.2±1,212.7 | |
| RIPC | 5147.7±1899.5 | 3732.2±2447.7 | 3335.3±1976.4 | 3677.8±2234.4∗∗ | 3338.1±2427.8 | 2815.1±1845.2 | |
| RPerC | 5730.5±1270.0 | 4149.4±1792.2 | 4179.2±1460.1 | 3601.6±1018.3 | 3510.0±1193.7 | 3069.0±1538.5 | |
| RIPostC | 5825.3±1864.3 | 3357.2±1058.9 | 3558.4±1004.5 | 3503.2±1184.0 | 3518.3±1256.2 | 3130.0±1045.8 | |
| -dp/dtmax(mmHg/s) | Sham | 3759.9±694.4 | 3816.9±910.7 | 3818.4±871.2 | 3714.8±786.1 | 2866.4±1075.8 | 2553.3±934.9 |
| IR | 3495.3±692.5 | 2982.1±843.9 | 2740.0±617.5∗∗ | 2638.4±552.6∗∗ | 2292.0±850.5 | 1697.6±733.1 | |
| RIPC | 3943.2±1490.4 | 2678.9±1740.9 | 2419.0±1132.2 | 2578.8±1577.7 | 2088.9±1563.7 | 1958.3±1428.4 | |
| RPerC | 4159.0±969.8 | 3194.1±1236.4 | 2993.2±1007.6 | 2899.1±844.8 | 2544.9±917.4 | 2110.9±969.7 | |
| RIPostC | 3916.4±1543.0 | 2333.6±627.8 | 2725.5±729.3 | 2631.2±652.2 | 2522.6±913.2 | 2149.1±940.2 |
Notes: Data are represented as means±SD. IR, ischemia/reperfusion; RIPC, remote ischemic preconditioning; RPerC, remote ischemic perconditioning; RPostC, remote ischemic postconditioning; LVSP, left ventricle peak systolic pressure; LVEDP, left ventricular end-diastolic pressure; +dP/dtmax, maximal rate of increase in intraventricular pressure; -dP/dtmax, maximal rate of decrease in intraventricular pressure. ∗∗p<0.05 vs. sham group; ∗p<0.05 vs. IR group.
It was shown that the AAR was comparable among the five different groups (data not shown). Specifically, there was no visible ischemic or necrotic area in the hearts of the rats in the sham group, and additionally no significant differences were observed in the AAR/LV (p = 0.698) of the other groups. However, the infarct size in the IR group (34.74±5.85) was found to be significantly larger than those of the RPerC, RIPC, and RIPostC groups (15.27±5.19, 14.53±3.45, and 19.84±5.85, respectively; p<0.05) (Figure 3).
Analysis of myocardial apoptosis-relevant proteinsIt was shown that the expression of Bcl-2 in all three of the remote limb conditioning groups was higher than that in the IR group, while the expression of Bax in the three conditioning groups was lower. Moreover, the differences of these two apoptosis-relevant proteins between the RIPC group and the IR group were significant, as were the differences between the RIPostC and IR groups. Based on the staining analysis, the ratio of Bcl-2/Bax protein expression was found to be higher in rats from all three remote limb conditioning groups compared to those from the IR group (p = 0.035, 0.048, 0), but with regard to the Bcl-2/Bax ratio, there was no significant difference among the three remote limb conditioning groups (Table 2).
Data on Bcl-2 and Bax expression obtained from each group of rats.
| Groups | Bcl-2 (PU) | Bax (PU) | Bcl-2/Bax (PU) |
|---|---|---|---|
| IR group | 51.3±3.9 | 51.8±5.3 | 1.003±0.159 |
| RIPC group | 56.9±2.6 | 40.3±6.4 | 1.463±0.290∗ |
| RPerC group | 54.3±1.4∗ | 43.6±2.1∗ | 1.255±0.053∗ |
| RIPostC group | 56.9±1.4∗ | 42.9±13.5∗ | 1.461±0.541∗ |
Data are expressed as means±SD. Positive unit is abbreviated as PU. ∗p<0.05 vs. IR group.
Using evidence from a rat myocardial IRI model, this study indicated that all three remote techniques of transient IR in double-sided hind limbs (i.e., preconditioning, perconditioning, and post-conditioning) can induce definitive cardiac protection characterized by reducing the reperfusion ventricular arrhythmia and the infarct size in the myocardial areas subject to sustained occlusion of the LCA followed by reperfusion. RPerC (1.50±0.97) was shown to inhibit reperfusion ventricular arrhythmia more significantly than RIPC and RIPostC (1.83±1.27 and 2.00±0.89, respectively).
The potential of reducing the myocardial infarct size using these three approaches is almost equivalent. These results were similar to the results reported by Basalay et al. (16), in which a similar degree of cardioprotection could be achieved with IR of the remote tissue applied prior to, during or as late as 10 min after the onset of myocardial reperfusion. However, this cardioprotective phenomenon, which results from remote ischemic conditioning, is not always accompanied by the recovery of the maximum and minimum first derivative of the left ventricular peak systolic pressure.
Based on the evidence mentioned above, RPerC is believed to potentially offer an adjunctive alternative to maximize the protective effects of RIPostC, and both of them are clinically applicable. We purposefully delivered the RPerC therapy at the end of the index ischemia period to mimic the clinical scenarios, as the therapy is usually carried out in the late phase of an ischemic episode (17). Nevertheless, it remains unclear whether more cycles of remote conditioning would lead to greater protection either alone or in combination. Unfortunately, the time limitation of our ischemic duration and the need for early intervention during reperfusion rendered additional limb conditioning unachievable in this protocol or most likely clinically irrelevant.
In contrast, there is much less data on the effect of remote conditioning on reperfusion arrhythmia. Galagudza et al. (18) found that Langendorff-perfused rat hearts that demonstrated persistent ventricular fibrillation following 15 min of reperfusion and a subsequent 30 min of regional ischemia benefited from postconditioning induced by 2 min of global ischemia followed by reperfusion. Many studies have suggested that transient Ca2+ overload could be one cause of this phenomenon. A proposed mechanism for the potential of remote conditioning to reduce reperfusion arrhythmia and myocardial infarct size involves the actions of adenosine, opening of the mitochondrial KATP channel and closing of the mitochondrial permeability transition pore, which are pathways that may also affect the benefits of preconditioning. Here, we demonstrated that RPerC has the potential to be an antiarrhythmic therapy for reperfusion-related arrhythmia.
Cardiac myocytes undergo apoptosis in response to a myriad of stimuli, including hypoxia, reoxygenation, acidosis, oxidative stress, glucose deprivation, and metabolic inhibition. Despite the fact that pharmacological studies have been less consistent, caspase inhibitors were reported to reduce infarct size by 21%-52% (19). The intrinsic pathway of myocyte apoptosis is regulated by members of the Bcl-2 family. Antiapoptotic protein Bcl-2 and Bcl-XL promote cell survival by suppressing the function of the proapoptotic Bcl-2 proteins, such as Bax. Bcl-2 has been reported to play an important role in preconditioning, and exposing the hearts to a short period of ischemia/reperfusion could lead to the significant induction of Bcl-2 expression (20). In addition, Bax has also been reported to be activated in cardiac cells in response to oxidative stress (21) and during ischemia (22). Thus, it could be inferred that the cardioprotective effect of RPerC is related to the Bcl-2 family and could be improved through higher Bcl-2 expression and lower Bax expression.
Although the actual mechanism through which an episode of transient IR in an organ or tissue can deliver protection against a subsequent sustained insult of IRI in a remote organ or tissue is currently unknown, we demonstrated here that three remote conditioning strategies are all potential therapeutic alternatives for cardiac IRI and that RPerC is thought to have the greatest ability to prevent reperfusion arrhythmia.
Biologically, RPerC characterized in animal experiments remains a healthy heart phenomenon, and its translation to clinical practice cannot be taken for granted. In fact, a number of co-morbidities that are frequently present in patients suffering from AMI are related to the loss of protection from different ischemic conditionings (23). Recognizing the potential of RPerC and understanding its underlying signal transduction may provide an important cardioprotection paradigm and lead to clinical interventions (24).
The authors wish to thank Xiao-Kun Wang for her excellent technical assistance. This work was supported by grants from the Wuhan General Hospital of Guangzhou Command (grant number 2008011).
No potential conflict of interest was reported.
Liu Y participated in the experimental design, analyzed the data, prepared the figures and performed the experiments. Zhu SB performed the experiments and the statistical analysis, reviewed the manuscript and approved the manuscript final version. Zhu Y was responsible for the manuscript first draft. Zhu J was responsible for the manuscript English version, conducted the literature search and chose Clinics journal for submission. Yin GL and Zhang Y revised the manuscript. Yin GL, Wang RP, Zhang Y, Zhu J and Jiang W performed part of the experiments.