To evaluate the results of the treatment of patients with isolated meniscal injuries of different etiologies.
MATERIALS AND METHODS435 patients of both sexes and different age groups underwent meniscectomy after their isolated meniscal injuries were clinically diagnosed and confirmed by nuclear magnetic resonance imaging.
RESULTSMost patients achieved good results and were able to return to the activities they had practiced prior to surgery without major limitations.
CONCLUSIONSMeniscectomy for the treatment of traumatic meniscal injury provides better results than meniscectomy for the treatment of degenerative meniscal injury. The results of meniscectomy for the treatment of meniscal injury due to fatigue are similar to those of meniscectomy for the treatment of traumatic meniscal injury, although the risk of osteonecrosis development is higher.
Avaliar os resultados do tratamento de pacientes com lesão meniscal isolada de diversas etiologias.
MATERIAIS E MÉTODOS435 pacientes de ambos os sexos, de diferentes faixas etárias, foram submetidos a meniscectomia depois que a lesão meniscal isolada foi diagnosticada clinicamente e confirmada por ressonância nuclear magnética.
RESULTADOSA maioria dos pacientes obteve bom resultado, retornando às atividades que exerciam antes da cirurgia, sem limitações relevantes.
CONCLUSÕESNo tratamento da lesão meniscal traumática, a meniscectomia dá melhores resultados do que no tratamento da lesão meniscal degenerativa. No tratamento da lesão meniscal por fadiga, a meniscectomia dá resultados semelhantes aos obtidos no tratamento da lesão meniscal traumática, apesar de haver maior risco de ocorrência de osteonecrose.
Meniscal injuries often occur in knee pathology, although with different etiologies. Such injuries may occur (i) as part of a rotational trauma, (ii) due to bending, as a result of progression of a degenerative process, or (iii) as a spontaneous injury caused by fatigue.
The different etiologies converge into the same symptomatology, with similar clinical manifestations and treatments, although different therapeutic results are expected. When associated with the instability of the knee or with arthrosis at an advanced stage, meniscal injury is analyzed as a function of the major pathology.
The objective of this study was to verify the natural history of a group of patients with isolated meniscal injuries and relate the different etiologies with the results of the treatment.
MATERIALS AND METHODSThe natural history of 435 patients with isolated meniscal injuries was monitored for 4 years. Of these, 261 (p=0,6) were men and 174 (p=0,4) women. The 50 to 59 year age group prevailed (average 57,01). The most frequently affected side was the right side (p=0,543), and the most frequently injured meniscus was the medial meniscus (p=455) (Table 1).
Distribution of patients with meniscal injury according to sex, age, side affected, and injured meniscus
| Patients | n | P |
|---|---|---|
| Sex | ||
| Male | 261 | 0,6 |
| Female | 174 | 0,4 |
| Total | 435 | 100 |
| Side | ||
| Right | 232 | 0,543 |
| Left | 186 | 0,455 |
| Bilateral | 17 | 0,002 |
| Total | 435 | 100 |
| Meniscus | ||
| Medial | 359 | 0,83 |
| Lateral | 50 | 0,11 |
| Duplicated | 26 | 0,06 |
| Total | 435 | 100 |
n = number of patients. p = relative frequency
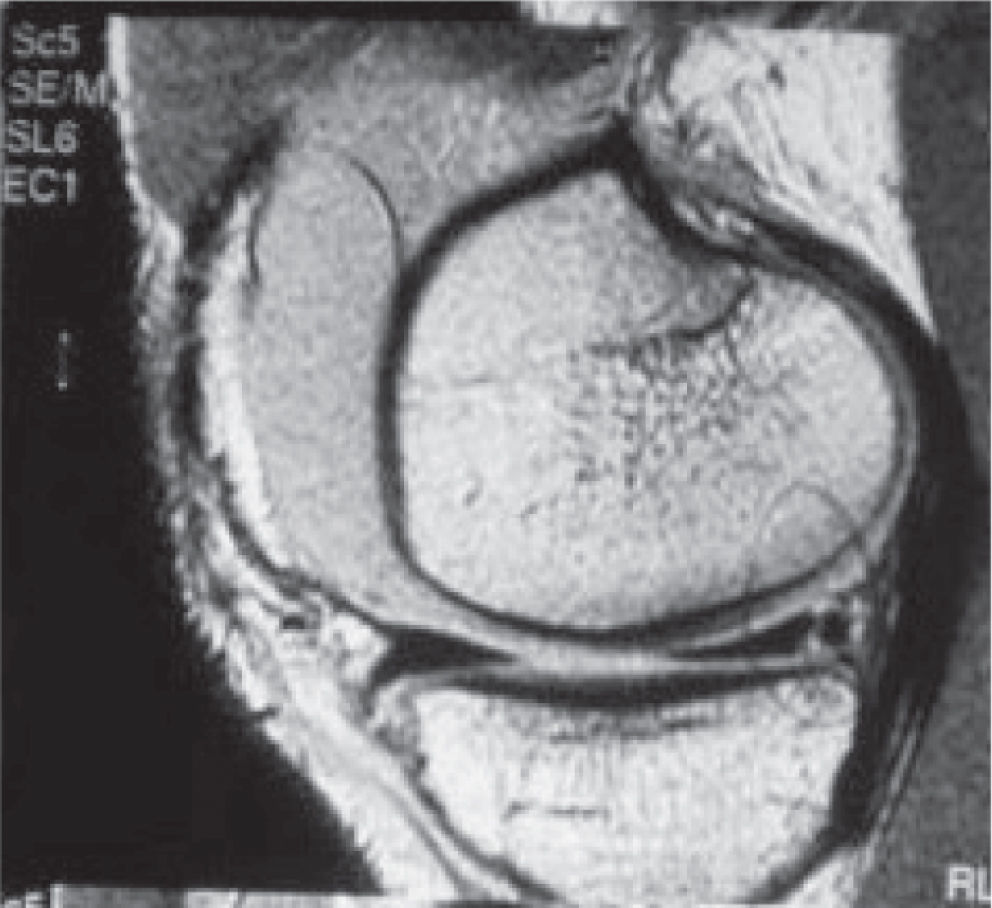
The diagnosis of meniscal injury was obtained clinically, and confirmed by nuclear magnetic resonance (NMR) imaging in all patients (Figure 1).
The clinical evaluation was based on palpation maneuvers of the articular femur-tibia interline, first with the knee bent to 90 degrees and later associated with bending-extension movements.
All patients underwent X rays of their affected knees (frontal and side views). Patients with radiographic signs of osteoarthritis, such as articular pinch and deviation of the axis, were excluded from this study.
Chondral injuries observed by NMR imaging were not considered as an exclusion criterion. Ninety-two patients presented chondral injuries shown in the NMR image.
Based on the clinical history of the meniscal injury, we divided the patients into 3 groups, according to the etiology (Table 2):
I - Traumatic injury group, formed by 194 patients with clear clinical history of trauma reported at a given time.
II - Degenerative injury group, formed by 101 patients whose history did not have a precise time of symptom onset. In the beginning, the complaint was insidious and progressive.
III - Injury due to fatigue group, formed by 140 patients who reported the onset of symptoms in an acute manner, without any occurrence of trauma or any other explanation to account for the injury (Table 2).
Based on their clinical histories, patients with meniscal injury were analyzed for distribution of the 3 etiologies according to gender and age group. A similar analysis was performed for the distribution of outcome.
All patients had a 4-year follow-up period, after which the evaluation time was considered terminated.
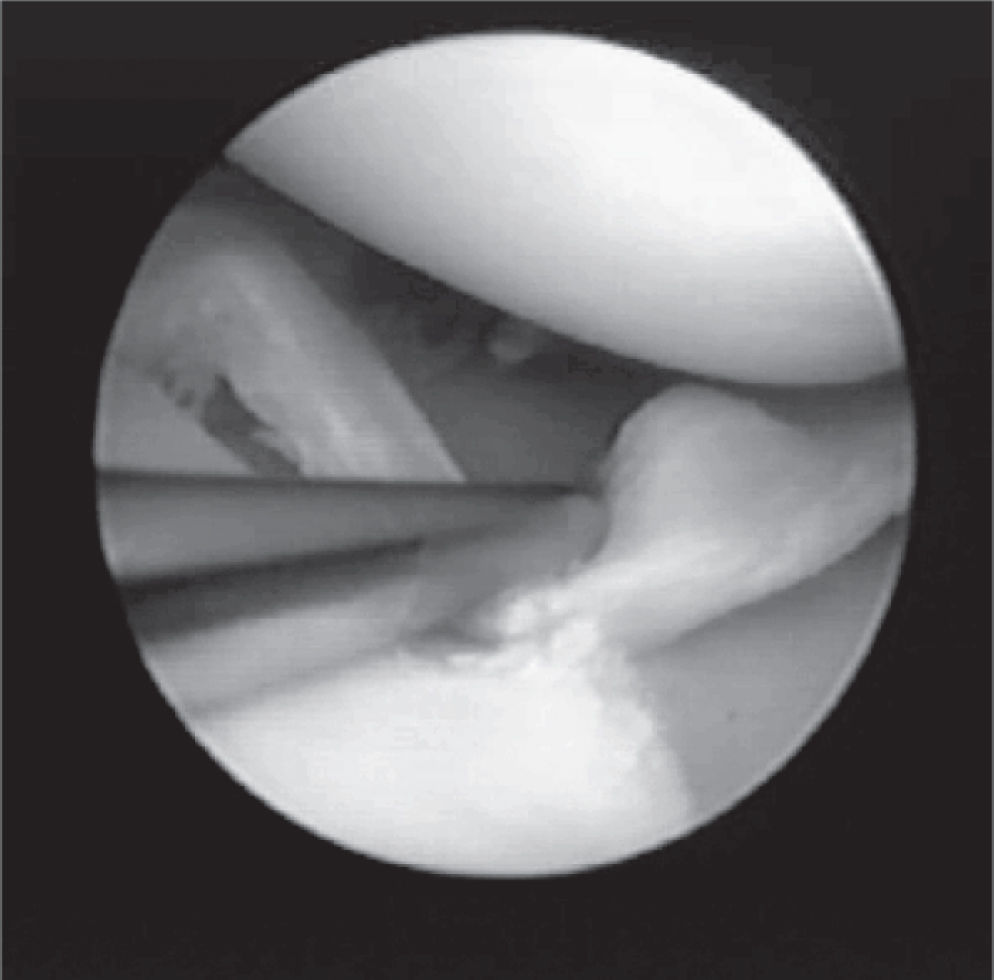
Surgery was performed arthroscopically in all patients (Figure 2).
During the 6 months of follow-up, patients were evaluated through regular office visits; after this period, they were evaluated through telephone calls, up to the fourth year of progression.
Statistical anaysis. The etiology of traumatic the lesions was analyzed across gender and age groups, as well as for outcome through chi-sqared tests. Statistical significance was accepted for p values < 05.
RESULTSThe distribution of injury etiology, according to gender is showen in Table 3. It can be seen that traumatic injuries prevailed in the male group, where trauma was the cause of 51.0% of the injuries. In females distribution was even for traumatic, degenerative and fatigue injuries. The differences were highly significant (p < 0,001). Table 4 displays the distribution of etiology through the age groups: again, a highly significant difference (p < 0,001) was found, with traumatic injuries prevailing in the 40 to 49 year and 50 to 59 year groups; fatigue injuries prevailed in the 60 to 70 year age group, while degenerative injuries prevailed the group of 70 year olds and over.
In table 5 we classified results into 2 categories: Good patients who were able to return to the activities they practiced before undergoing surgery, without major limitations; and Poor patients whose symptoms persisted after 6 months of evolution or who had any major complication secondary to the surgery.
Outcomes according to etiology are displayed in Table 6. Taken as a whole, outcomes of meniscectomy for the treatment of isolated meniscal injuries provided good results in most patients (363 patients). However, in 71 patients, the result of the treatment was rated as poor. Of these patients, 15 (out of 194 patients) were in the traumatic group, 43 (out of 101 patients) were in the degenerative group, and 13 (out of 140 patients) were in the fatigue group, a highly significant (p <.001) difference, which derives from the higher incidence of poor results in the degenerative group. Six patients progressed to idiopathic osteonecrosis of the knee.
All injuries affected the medial femoral condylus. All patients with clinically diagnosed injury due to fatigue were females.
Fourteen patients presented synovitis that persisted for 3 to 6 months and resolved in all cases. However, it was not possible to correlate the synovitis with the data of identification or diagnosis.
An NMR image evaluation showed chondral injury of different levels of severity in 92 patients. Chondral injury was confirmed by arthroscopy in these 92 patients, and osteochondral injury was discovered by arthroscopy in another 10 patients. These results were related to the presence of osteochondral injury with loss of consciousness (LOC) diagnosed by arthroscopy according to the etiology of the injury.
DISCUSSIONThe reasons that led us to analyze this group were the distinct, easily determined clinical features and their relationship with the result of the meniscectomy.
We believe that from a fairly simple clinical evaluation it is possible to project the prospective results of meniscectomy.
Based on archival data, we identified 3 clinical forms (traumatic, degenerative, and fatigue etiology), and we could fit all patients into 1 of these 3 groups.
Isolated meniscal injuries are much more frequent in patients over 50 years of age. In this series, such patients represent 72.6% of all cases. The distribution among patients with traumatic injuries, degenerative injuries, and injuries due to fatigue varied widely according to age.
On the average, fatigue injuries represented 140 patients with all injuries, with uniform distribution among the different age groups considered.
The names assigned to each type of injury are not based on the literature. Rather, they are based on etiologies, except for the fatigue injury that appears spontaneously, presenting acute symptoms and occurring almost exclusively in the cornu posterius of the medial meniscus as a radial injury, suggesting that it is rather a meniscal injury due to fatigue than a traumatic or degenerative injury. Due to the absence of an etiology-based diagnosis and due to the similarity with the clinical condition of injuries due to fatigue, we named this type of injury ‘fatigue injury.’
Drosos and Pozo1 studied 392 patients who underwent meniscectomy because of meniscal injury, and they were not able to identify the cause of the injury in 28.8% of them.
Ours was a clinical diagnosis supplemented by NMR imaging in all cases. NMR is increasingly proving itself to be a gold standard for a number of different pathological conditions. 2 Surgical arthroscopy allowed us to definitely confirm our diagnosis. Based on this information, we found that the accuracy of the clinical diagnosis based on the patient's history and on the classical stress maneuvers of the meniscus, such as knee bending and rotation, was adequate for diagnosing the majority of patients concerning their meniscal injuries. In 96% of cases of meniscal injury, the NMR imaging merely confirmed the clinical diagnosis. Similarly, Rose and Gold2 compared the accuracy of clinical diagnosis with that of NMR diagnosis and found no significant differences concerning meniscal injuries. Conversely, very seldom were osteochondral injuries diagnosed by clinical evaluations; however, the evaluation of NMR images allowed diagnosis of 90% of the chondral injuries.
Rose and Gold3 compared the accuracy of clinical diagnosis with that of NMR diagnosis and observed no significant differences concerning meniscal injuries.
The study of the results showed that chondral injuries promote major worsening of results.
It is worth emphasizing that patients with radiologic alterations showing arthritis did not undergo meniscectomy. We had previously observed that patients with radiographic signs of arthritis evolve poorly when subjected to isolated meniscectomy.4
Regarding outcomes for meniscectomy not complicated with chondral damage, results have been found to be largely good. Similarly to our results, a previous study showed that of 119 patients who did not have chondral injury and underwent meniscectomy, the results achieved by 91.7% were deemed good after 4 years, and after 12 years, results were deemed good in 94.8% of these patients.5
The benefit that meniscectomy may bring to patients with chondral injury is controversial. In the study mentioned above, the results of only 62% of patients presenting chondral injuries and analyzed 12 years after the meniscetomy were deemed good. In our study, 48% of the patients with chondral injury diagnosed by NMR imaging had poor results; this proved to be a much worse clinical picture when compared to those in the general group, 16.5% of whom had poor results.
Dervin et al6 studied the evolution of 126 patients subjected to arthroscopic debridement, 79 (63%) of whom had unstable meniscal injuries. The authors evaluated the results by analyzing the quality of life of patients according to 2 methods SF36 and WOMAC, which is specific for osteoarthritis and observed that most patients showed significant improvements in their quality of life. Pearse and Craig7 studied the evolution of 126 patients with severe osteoarthritis who underwent to meniscectomy, and found that although meniscectomy did not change the evolution of osteoarthritis, the surgery promoted improvement in the symptoms of osteoarthritis. Although these are basically clinical evaluations of the evolution of a complex pathology, just a little over half of our patients had their symptoms improved. Menetrey et al8 studied the evolution of meniscectomy in patients over 50 years of age and found that 90% of patients with traumatic injuries had good results, while only 20% of patients with degenerative alterations had good results. Both groups were very similar in age, showing that age is not a factor responsible for poor results. Degenerative alterations increased with age in our group of patients; however, we fully agree that the cause of poor results is not the age, but the degenerative alterations. Higuchi et al9 studied the factors responsible for poor results of meniscectomy after a 12.2-year follow-up period and found that age and sex did not influence the evolution of meniscectomy.
We had few complications secondary to meniscectomy; however, 6 patients evolved to idiopathic knee osteonecrosis. It is very difficult to correlate osteonecrosis with meniscectomy, since there are many cases of osteonecrosis without meniscectomy. Johnson et al,10 while studying idiopathic osteonecrosis in patients subjected to arthroscopy because of meniscal injuries, could not correlate NMR images and meniscal injuries to osteonecrosis and suggested that further studies should be performed on this subject. We believe that idiopathic osteonecrosis is in fact the result of a fracture caused by femoral or tibial condyle stress.11 Therefore, the occurrence of this injury in patients with meniscal injury (which we call fatigue injury) is probably part of a complex of injuries caused by knee fatigue. Possibly NMR imaging or scintigraphy may be of help when diagnosing this fatigue condition before meniscectomy.
CONCLUSION1 - Meniscectomy for the treatment of traumatic meniscal injury gives better results than meniscectomy for the treatment of degenerative meniscal injury.
2 - Meniscectomy for the treatment of meniscal injury caused by fatigue gives results similar to those of meniscectomy for the treatmentof traumatic meniscal injury, although the risk of osteonecrosis is higher.
3 - Meniscectomy for the treatment of degenerative meniscal injury gave unsatisfactory results in 42.5% (43 patients) during the follow-up period.