To evaluate the use of subconjunctival bevacizumab on corneal neovascularization in an experimental rabbit model for its effect on vessel extension, inflammation, and corneal epithelialization.
METHODS:In this prospective, randomized, blinded, experimental study, 20 rabbits were submitted to a chemical trauma with sodium hydroxide and subsequently divided into two groups. The experimental group received a subconjunctival injection of bevacizumab (0.15 m; 3.75 mg), and the control group received an injection of 0.15 ml saline solution. After 14 days, two blinded digital photograph analyses were conducted to evaluate the inflammation/diameter of the vessels according to pre-established criteria. A histopathological analysis of the cornea evaluated the state of the epithelium and the number of polymorphonuclear cells.
RESULTS:A concordance analysis using Kappa's statistic showed a satisfactory level of agreement between the two blinded digital photography analyses. The neovascular vessel length was greater in the control group (p<0.01) than in the study group. However, the histopathological examination revealed no statistically significant differences between the groups in terms of the state of the epithelium and the number of polymorphonuclear cells.
CONCLUSIONS:Subconjunctival bevacizumab inhibited neovascularization in the rabbit cornea. However, this drug was not effective at reducing inflammation. The drug did not induce persistent corneal epithelial defects.
Ocular trauma, infection, inflammation, and degeneration result in corneal neovascularization.1 Neovessels cause structural changes that allow the overflow of fluid to the extravasculature, blood stasis and hemorrhage, and they can reduce corneal transparency with subsequent and progressive vision impairment.1 Corneal neovascularization is one of the greatest risk factors for corneal transplant rejection2 because it allows leukocytes access to donor tissue antigens.
Corticosteroids are the first-line treatment for corneal neovascular diseases because of their ability to reduce the inflammatory process4 and vascular proliferation, both of which are initiated soon after the ocular trauma.5 However, side effects related to the non-specificity of corticosteroids limits their use. Such side-effects include the increased risk of cataracts and glaucoma due to high intra-ocular pressure (IOP).6
Vascular endothelial growth factor (VEGF) and its receptors play an important role in the neovessel formation that is observed in diabetic retinopathy, venous retinal occlusion, age-related macular degeneration, and corneal neovascularization.7 High VEGF expression was observed in neovascularized corneas after penetrating keratoplasty in corneal inflammatory diseases8 and in guinea pigs' corneas that were burned by alkalis during the healing process.9 Anti-VEGF drugs have sparked a revolution in the treatment of neovascular diseases by reducing neovascularization and also by their supposed action on fibroblasts.10 These drugs can provide beneficial effects after intra-vitreous injection in age-related macular degeneration (ARMD) neovascularization, diabetic retinopathy, and glaucoma, with minimal toxicity or side effects.11 These effects may also include the reduced formation of new vessels in other regions of the eye.
The aim of this prospective study was to investigate the effects of subconjunctival injections of bevacizumab on experimentally induced corneal neovascularization by focusing on the neovessel length, inflammation, and re-epithelization.
MATERIALS AND METHODSThis prospective, randomized, blinded study was performed at the Instituto de Pesquisas Médicas (IPEM) of the Faculdade Evangélica do Paraná (FEPAR) - Brazil and Hospital Universitário Evangélico de Curitiba (HUEC). The Animal Experimentation Norms and Principles proposed by the Colégio Brasileiro de Experimentação Animal (1994) were followed.
The studied variables include the vessels' lenght, degree of inflammation/diameter, epithelium integrity, and number of polymorphonuclear cells (PMN).
InterventionTwenty corneas of twenty New Zealand rabbits were studied. All rabbits were healthy male albinos, weighing between 2.300 and 2.500 kg and were three to four months old.
The rabbits were intramuscularly anesthetized with xylazine hydrochloride 0.1 ml/Kg (2.3 mg/kg) and ketamine hydrochloride 0.2 ml/Kg (10 mg/kg). The animals were divided randomly into a control group (Group 1) (n = 10) and a study group (Group 2)(n = 10).
The left corneas of the animals were exposed to 1 N sodium hydroxide (NaOH), through a 5 mm diameter filter paper that was applied to the superior cornea tangential of the limbus for 20 seconds, followed by washing with 20 ml of 0.9% saline solution. Subsequently, the control group animals received a subconjunctival injection of 0.15 ml of 0.9% saline solution, whereas the study group animals received a subconjunctival injection with 0.15 ml (3.75 mg) of bevacizumab (Figure 1). The injections were performed superiorly and close to the burned area. One surgeon performed all of the procedures in a blinded fashion.
The rabbits in Groups 1 and 2 were again anesthetized, examined and digitally photographed 14 days after the corneal burn and were euthanized by a 5-ml intramuscular sodium pentobarbital injection. Subsequently the corneas were removed, maintaining a scleral margin of 3 mm, fixed in formalin for 24 hours and submitted for histopathological study with hematoxylin-eosin. The corneal epithelium integrity, or lack thereof, and the number of PMN cells per field were observed at a magnification of 400x using an optical microscope. The most damaged field in the opacity area was utilized.
Digital images were obtained to examine the vessel extent and the vessel inflammation/diameter in the frontal position using a Sony Cybershot® (Sony Corporation – Tokyo/Japan) 7.2-megapixel camera, which was supported by a fixed tripod with an accessory Zeiss® (Carl Zeiss AG – Oberkochen/Germany) lens with a magnification of 40x at a distance of 5 cm. Each animal was submitted to two digital photography evaluations for each variable (vessel extent and vessel inflammation/diameter). A cornea specialist performed the two evaluations of the digital pictures in a blinded and randomized fashion. The corneal neovascularization was determined using a score given by the cornea specialist according to the vessel extent and inflammation/diameter degree observed.
The vessel extent was determined using a scale from 0 to 4 (0 – no vessels on the corneal limbus; 1 – vessels that advanced over the corneal limbus, covering 0-25% of the burned area; 2 – vessels that reached 25-50% of the burned area; 3 – vessels that reached 50-75% of the burned area; 4 – vessels that extended to the entire burned area).
The inflammation and diameter degree on the vessels were determined using a scale from 0 to 3: (0 – no inflammation or vessels; 1 – little inflammation and vessels of small diameter; 2 – moderate inflammation and vessels of medium diameter; 3 – intense inflammation and vessels of large diameter).
Statistical AnalysisTo validate the evaluation model, the reproducibility of these measurements was evaluated using the Kappa statistic.
For each evaluation, the two groups were compared with respect to the ordinal variables by using the Mann-Whitney non-parametrical test. The group comparison for dichotomous variables was executed using the Fisher exact test. p<0.05 indicated statistical significance.
RESULTSOn the seventh day after the corneal burn, a rabbit from the study group presented corneal perforation and was excluded from the research. Thus, 19 animals were left in the study, including ten from the control group and nine from the study group.
The digital pictures of each animal were submitted to two evaluations for each variable, as shown in Table 1 (control group) and Table 2 (study group).
Blinded photographic analysis of vessel extent and inflammation/diameter in the control group, fourteen days after chemical burn.
| Animal | Vessel Extent | Vessel Inflammation/Diameter | ||
|---|---|---|---|---|
| Evaluation 1 | Evaluation 2 | Evaluation 1 | Evaluation 2 | |
| 1 | 2 | 3 | 1 | 1 |
| 2 | 3 | 3 | 2 | 2 |
| 3 | 2 | 2 | 2 | 1 |
| 4 | 2 | 3 | 1 | 1 |
| 5 | 3 | 3 | 2 | 2 |
| 6 | 3 | 3 | 2 | 2 |
| 7 | 4 | 4 | 1 | 1 |
| 8 | 3 | 3 | 3 | 3 |
| 9 | 3 | 3 | 3 | 3 |
| 10 | 2 | 2 | 1 | 2 |
Blinded photographic analysis of vessel extent and inflammation/diameter in the study group, fourteen days after the corneal burn.
| Animal | Vessel Extent | Vessel Inflammation/Diameter | ||
|---|---|---|---|---|
| Evaluation 1 | Evaluation 2 | Evaluation 1 | Evaluation 2 | |
| 1 | 1 | 1 | 2 | 2 |
| 2 | 1 | 1 | 3 | 3 |
| 3 | 2 | 1 | 2 | 2 |
| 4 | 1 | 2 | 1 | 2 |
| 5 | 1 | 1 | 1 | 1 |
| 6 | 1 | 1 | 1 | 2 |
| 7 | 1 | 1 | 1 | 2 |
| 8 | 1 | 1 | 1 | 2 |
| 9 | 1 | 1 | 2 | 2 |
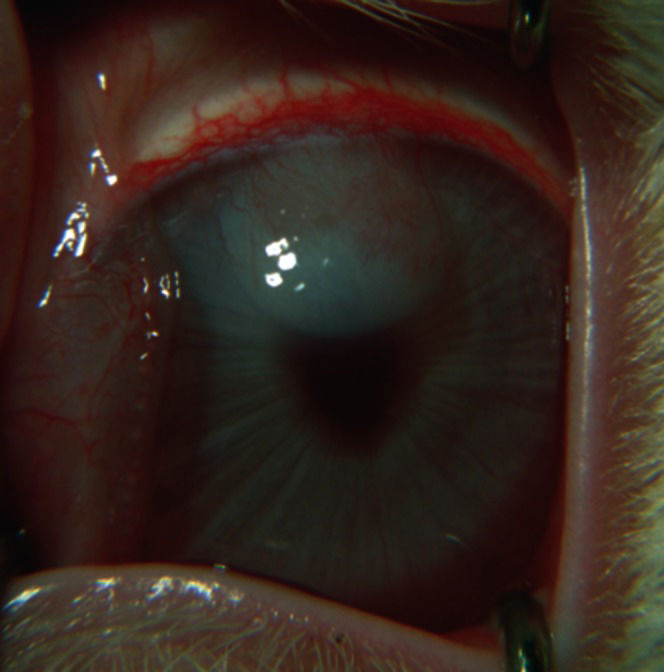
Animal 8 of the control group (Figure 1) had a cornea classified as degree 3 in both evaluations (vessels reaching up to 75% of the burned area) according to the vessel extent criteria and inflammatory reaction (intense inflammation and vessels of large diameter). Animal 5 of the study group (Figure 2) had a cornea classified as degree 1 for both vessel extent criteria (vessels advancing over the corneal limbus, reaching up to 25% of the burned area) and inflammatory reaction (little inflammation and small-diameter vessels).
The concordance analysis of the vessel extent estimated by the Kappa coefficient was 0.705 (95% confidence interval: 0.514 – 0.895), which indicates a high level of agreement between the two evaluations. The estimated Kappa coefficients for each of the vessel extent classifications are presented in Table 3. The concordance was better characterized at the most extreme degrees (1 and 4).
Concordance analysis among evaluations with respect to vessel extent.
| Classification | Kappa | CI 95% | Concordance |
|---|---|---|---|
| Degree 0: no vessels on the corneal lamina | - | - | - |
| Degree 1: vessels that advanced over the corneal limbus, reaching up to ¼ of the burned area | 0.863 | 0.541 – 1 | Excellent |
| Degree 2: vessels that advanced over the corneal limbus, reaching up to ½ of the burned area | 0.471 | 0.149 – 0.794 | Good |
| Degree 3: vessels that advanced over the corneal limbus, reaching up to 3/4 of the burned area | 0.644 | 0.322 – 0.967 | Good |
| Degree 4: vessels that extended throughout the entire burned area | 0.824 | 0.502 – 1 | Excellent |
CI – confidence interval.
Regarding the vessel inflammation/diameter, the estimated Kappa coefficient between the two blinded evaluations was 0.500 (95% confidence interval: 0.269 – 0.731), which again indicates a satisfactory level of agreement between the two evaluations. The estimated Kappa coefficients for each classification of vessel diameter are presented in Table 4.
Concordance analysis among the evaluations with respected to vessel diameter/inflammation.
| Classification | Kappa | CI 95% | Concordance |
|---|---|---|---|
| Degree 0: no vessels or inflammation | - | - | - |
| Degree 1: little inflammation, vessels of small diameter | 0.383 | 0.061 – 0.706 | Weak |
| Degree 2: moderate inflammatory reaction, medium diameter vessels | 0.339 | 0.017 – 0.661 | Weak |
| Degree 3: intense inflammatory reaction, vessels of large diameter | 0.853 | 0.531 – 1 | Excellent |
CI – confidence interval.
Although a satisfactory level of reproducibility was found in the evaluations of large diameter vessels, the concordance seemed to be weak at Degrees 1 and 2, indicating a difficulty in distinguishing between little and moderate inflammation.
The comparison among the study and control groups considered the average of the two evaluations. The null hypothesis of the same results in both groups was tested versus the alternative hypothesis of different values for the considered variable.
The analysis of the vessel extent showed a significant difference between the control and the study group, with smaller vessels being found 14 days after the chemical burn in the study group (Table 5). Nevertheless, no meaningful difference was found among the same groups during the same follow-up when evaluating the vessel inflammation and diameter (Table 6).
Analysis of vessel extent among the groups.
| Group | n | Median | Minimum | Maximum | p-value |
|---|---|---|---|---|---|
| Control | 10 | 3 | 2 | 4 | |
| Study | 9 | 1 | 1 | 1.5 | <0.001∗ |
Vessel inflammation/diameter analysis among the groups.
| Group | n | Median | Minimum | Maximum | p-value |
|---|---|---|---|---|---|
| Control | 10 | 1.75 | 1 | 3 | |
| Study | 9 | 1.5 | 1 | 3 | = 0.968∗ |
The microscopic evaluation of the corneal epithelial integrity revealed that the epithelium of all corneas from the study group had healed at 14 days compared with 60% in the control group (Table 7). Despite the reduced number of corneas that had epithelized in the control rabbits, no statistically significant difference was found between the groups.
A lower number of polymorphonuclear cells was found in the treated group compared with the control group. Figure 3 shows the polymorphonuclear infiltration in Animal 1 of the control group, whereas Figure 4 shows Animal 3 of study group, which displayed little polymorphonuclear infiltration and full corneal epithelium integrity. In spite of the discrepancies among some rabbits (Figures 3 and 4) and an overall lower number of PMNs being found in the study group, no meaningful statistical differences among the groups were encountered in terms of PMN cell number (Figure 5).
Previous studies used subconjunctivally administered bevacizumab at dosages varying from 1.25 mg to 3.75 mg.6,12,13 In this study, we chose a dose of 3.75 mg. Because we were only administering one injection during the study, we wanted a high dose that would suppress the initial angiogenic stimulus. No drug-related toxicity has been reported using this concentration. Hurmeric et al.13 compared the effect of injected bevacizumab when it was used immediately after the injury or at three days after the injury. Better anti-angiogenic responses were found in the group treated soon after the induced damage. Thus, we also administered the subconjunctival injection soon after the injury.
Vascular growth, which is mainly analyzed using the angiogenesis parameters of vessel extent and degree of inflammation, is usually determined through photographic analysis.12,6 However, no established model for this analysis was found. Thus, an experimental model of digital photographic analysis was established, which allowed the vessel extent and inflammation/diameter to be evaluated within the indicated time period. Other photographic evaluation methods have been applied with pixel counting or measurements. Although these methods give the impression of a mathematical certainty as they appear quantitative, the data are subjective with regard to where the vessels begin and end. In addition, the delineation of the affected area may not be accurate when it is determined mathematically. Thus, we have proposed a photographic clinical analysis, in which the evaluator, who is a cornea specialist, observes not only the vessel extent but also the vessel aspect and inflammation degree.
We chose to evaluate the corneas at 14 days because angiogenesis has shown a rapid growth until the 12th day in other models.14 In the previous studies, the vessel extent stabilized after this initial period. Fourteen days was sufficient to produce the highest level for each variable (vessel extent and inflammation).
On the seventh day, a rabbit from the study group showed corneal perforation and was excluded from the study. As only one rabbit showed perforation and the remaining rabbits in the group showed an intact epithelium by the end of the 14-day period, the perforation was unlikely to be directly caused by the drug. The rabbit may have had a bacterial infection in the wound that was acquired early in the experiment when the corneal epithelium was not fully healed.
Statistical analysis confirmed that the evaluation method was excellent for identifying vessel extension at Degrees 1 and 4 and good for identifying vessel extension at Degrees 2 and 3. The method was also good for identifying vessel inflammation/diameter, as indicated by the good agreement between the two blinded evaluations. For this variable, Degree 3 (intense inflammation and vessels of large diameter) showed excellent agreement.
The results obtained show that this method may be reproduced for the evaluation of other anti-angiogenic drugs intended to reduce corneal neovascularization.
There was a statistically significant difference in the vessel extent between the two groups, with a lesser extent in the study group compared with the control group. These data indicate a positive effect on the chemical burn and agree with the data found in recent literature.12,13 Neovascularization is considered to be related to a poor prognosis in corneal transplants because it interferes with corneal transparency, which can result in low visual acuity.1 Thus, bevacizumab may improve the prognosis in cases with progressive neovessels after penetrant keratoplasty or in the case of some chemical burns, especially those that require a corneal transplant.
The degree of inflammation was evaluated because although the drug does not possess direct anti-inflammatory actions, it does affect fibroblasts.15,16 Although its action in acute inflammation is not fully understood, some authors suggest that the drug decreases neutrophil invasion within the wound.17 The results for inflammation/diameter and the number of PMN cells showed that the drug does not have a clinically meaningful anti-inflammatory effect, which agrees with the theory that the inflammatory process has many pathways and the inhibition of VEGF alone does not significantly affect inflammation.
Through these data, we suggest that this treatment may be more effective when administered along with corticosteroids, which would reduce the inflammation. Further studies are necessary to determine whether concomitant inhibition of inflammation and neovascularization leads to massive cellular death by acute hypoxia, which may occur because of the inhibition of all physiological mechanisms involved in such ischemia.
The integrity of the corneal epithelium was evaluated on the 14th day because the drug may have affected the healing process and delayed wound healing. Rapid restoration of the epithelium is fundamental to the healing process and prevents wound contamination. The comparison between the two groups did not show persistent epithelial defects in the study group at the end of the follow-up. The results showed fewer corneas with an exposed stroma in the study group compared with the control group. However, no statistical difference was observed between the groups, which suggests that the drug did not impair epithelial healing. This study suggests that the bevacizumab has potential for use during the acute healing stage, in which the epithelium is still open. Corticosteroids should be used carefully during this stage because they may impair epithelial healing.18
Delayed epithelial healing has been described previously19,20 and is believed to be caused by the reduced expression of surface integrins and collagens, which interferes with epithelial cell adhesion. However, these studies were performed with higher doses that were applied topically several times a day. Kim et al. showed a dose-related effect.20 Thus, we suggest that the subconjunctival administration is safer because in our study, it did not jeopardize the re-epithelialization.
Chalam et al.21 showed that bevacizumab is not toxic to corneal cells or fibroblasts when administered in concentrations up to 25 mg/ml. This finding is supported by the current study, in which there was no inhibition of re-epithelialization.
Although the neovascularization induced by the burn was suppressed, the suppression was not as complete as has been described in previous studies.12 This is possibly because VEGF is not the only factor responsible for angiogenesis. Other pro-angiogenic factors, such as TGF-beta and fibroblast growth factor, may still be involved.16 We suggest that bevacizumab should not to be used as a monotherapy; instead, it should serve as one aspect of a multi-factorial treatment alongside other drugs, such as corticosteroids, in acute cases. This association has not been fully studied, and some conflicting results have been reported. Using a rabbit model, Kang et al.22 showed that a combined treatment of bevacizumab and triamcinolone acetonide was no more effective than the use of bevacizumab alone. Another study23 examined the inhibition of neovascularization in a rat model using bevacizumab alone and with dexamethasone. However, again there was no clear advantage when dexamethasone was included. Newer anti-angiogenic drugs have also been studied over the last year with promising results. For example, suramin is a non-specific anti-angiogenic drug that has a longer half-life than bevacizumb. It has been suggested that this association could provide a more potent and longer effect.24 Pérez-Santonja et al.25 showed a greater inhibition of the neovessels by sunitinib (an anti-VEGF and anti-PDGF drug) compared with bevacizumab.
It has been found that established neovessels, such as those in diabetic retinopathy, are re-established after the drug is discontinued, thereby requiring additional treatments.26 The drug's effect has not been extensively studied in cases of acute neovascularization, such as that following burns or the initial neovessel growth following a corneal transplant. It is also possible that if the angiogenic stimulus is reduced by specific inhibitors such as bevacizumab in the acute stage, neovessel formation may decrease in the long-term because the angiogenic stimulus has a short duration and is not maintained by the injury's physiopathology as it is in diseases such as diabetic retinopathy. Thus, this treatment could have a positive effect in the long-term for some treatments such as subsequent corneal transplants.
Anti-angiogenic drugs have a great potential for beneficial effects in severely neovascularized eyes with little or no limbal damage, which generally present with very low visual acuity. Presently, there is no available treatment for this condition. Further studies with different dosages and steroids combinations with the various VEGF inhibitors that compare not only the neovascularization itself but also the inflammatory response and side effects would contribute to the search for an ideal treatment. This association may have a synergistic effect on burns or in cases with a possibility of acute neovascularization, where the neovascular stimulus occurs as a part of the acute inflammatory response.
Thus, we conclude that the subconjunctival administration of bevacizumab efficiently reduces corneal neovascularization without inducing persistent epithelial defects following a chemical burn. However, this treatment does not show meaningful anti-inflammatory effects.