AO/OTA 31-A3 intertrochanteric femoral fractures have completely different fracture line directions and biomechanical characteristics compared with other types of intertrochanteric fractures. The choice of the fixation method has been a focus of dispute among orthopedic trauma surgeons. The purpose of this study was to review the outcomes of these fractures treated with a percutaneous compression plate at our institute.
METHOD:Seventeen patients with AO/OTA 31-A3 intertrochanteric femoral fractures were treated with a percutaneous compression plate at our institute from January 2010 to December 2011. The clinical data and imaging results were retrospectively analyzed.
RESULTS:The medical complication of popliteal vein thrombosis occurred in one patient. Sixteen patients were followed up for 12 to 21 months. Two patients had malunion and mild pain. Fracture collapse occurred in two patients, with one having head penetration. These two patients had moderate pain. There were no occurrences of nonunion or reoperation. The mean Harris hip score obtained during the last follow-up was 84.1 (61-97). Patients with a poor quality of reduction were more likely to have pain results (p =0.001). A trend existed toward the presence of a poor quality of reduction (p =0.05) in patients with a collapse of fracture. Patients with poor preoperative mobility were more likely to have a lower Harris hip score (p =0.000).
CONCLUSION:The percutaneous compression plate is an alternative device for the treatment of AO/OTA 31-A3 intertrochanteric femoral fractures. Good fracture reduction and an ideal placement position of the neck screw are important in the success of the device.
AO/OTA 31-A3 intertrochanteric femoral fractures are different from A1 and A2 intertrochanteric fractures because of their unique anatomical and biomechanical characteristics. According to the report by Haidukewych et al. (1), A3 fractures accounted for 2.2% of hip fractures and 5.3% of intertrochanteric fractures. Currently, there are two main types of implants available for these fractures, namely, extramedullary and intramedullary implants. The treatment of these fractures with a sliding hip screw (SHS) has the disadvantages of massive trauma, poor stability, and a high incidence of fixation failures. Haidukewych et al. (1), Rokito et al. (2), and Henry et al. (3) all believed that this device was not suitable for AO/OTA 31-A3 intertrochanteric femoral fractures. Treating these fractures with the intramedullary nail has an advantage with respect to mechanics and efficacy in clinical applications (4-6). However, it is not minimally invasive. Some unstable proximal femoral fractures, such as intertrochanteric fractures with extension into the piriform fossa (7), fractures in patients with short skeletons and narrow femoral canals (8), and fractures in which a closed reduction can only be performed in the abduction position, are assessed as difficult to treat with nails. Although intramedullary nails may have advantages over extramedullary fixation for AO type A3 fractures, there is currently insufficient evidence to confirm a significant superiority of these nails over extramedullary devices (9). Thus, there is considerable controversy regarding the choice of treatment.
In recent years, minimally invasive surgical techniques have been popularized. Clinical studies on the percutaneous compression plate (PCCP) treatment of intertrochanteric fractures have shown that it has the advantages of being minimally invasive (10-12) and stable (10,13); thus, the PCCP may become the implant of choice for intertrochanteric fractures in elderly patients with multiple comorbidities (14-16). Current studies have been mostly restricted to PCCP treatment for A1 and A2 fractures (10-13,17,18). AO/OTA 31-A3 intertrochanteric femoral fractures were considered to be an absolute contraindication for the PCCP by Peyser et al. (19). However, Simecek et al. (20) reported that the PCCP is suitable for all types of intertrochanteric fractures, including A3 fractures. No clinical study specifically on the PCCP treatment of AO/OTA 31-A3 intertrochanteric femoral fractures has been reported. In this retrospective study, we present the results of PCCP implants used to treat these fractures.
MATERIALS AND METHODSSeventeen patients with AO/OTA 31-A3 intertrochanteric femoral fractures were treated with the PCCP (Orthofix, Italy) at our institute from January 2010 to December 2011. Based on the AO/OTA classification (21), the fractures were classified as 1 case of type 31-A3.1, 5 cases of type 31-A3.2, and 11 cases of type 31-A3.3. The mean age of the patients was 77.8 (37-90) years, with 5 males and 12 females (Table1).
Evaluation of demographic characteristics, radiological results, mobility, and complications.
| Case | Gender | Age (years) | AO Fracture Types | Reduction | Position of Neck Screw | Mobility | Complications | |
|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | |||||||
| 1 | Male | 58 | A3.3 | Good | Good | Independent | Independent | |
| 2 | Female | 88 | A3.3 | Good | Good | Independent | One aid | |
| 3 | Female | 90 | A3.2 | Good | Good | One aid | One aid | |
| 4 | Male | 88 | A3.3 | Bad | Bad | Independent | One aid | Mild pain |
| 5 | Female | 87 | A3.3 | Bad | Bad | Independent | Independent | Mild pain |
| 6 | Male | 37 | A3.3 | Good | Good | Independent | Independent | Loosening of sleeve of neck screw |
| 7 | Female | 70 | A3.2 | Acceptable | Good | Independent | Independent | Loosening of sleeve of neck screw |
| 8 | Female | 82 | A3.3 | Bad | Good | Independent | Wheelchair | Collapse of fracture, moderate pain |
| 9 | Female | 84 | A3.3 | Good | Good | Independent | Independent | Protrusion of neck screw |
| 10 | Female | 72 | A3.3 | Bad | Good | Independent | Wheelchair | Collapse of fracture, moderate pain, head penetration |
| 11 | Female | 71 | A3.2 | Acceptable | Good | Independent | Independent | |
| 12 | Female | 82 | A3.1 | Good | Good | Independent | One aid | |
| 13 | Female | 86 | A3.3 | Good | Good | One aid | Frame | Protrusion of neck screw |
| 14 | Male | 81 | A3.3 | Good | Bad | One aid | Deceased | |
| 15 | Male | 80 | A3.2 | Acceptable | Good | Independent | One aid | Protrusion of neck screw, popliteal vein thrombosis |
| 16 | Female | 82 | A3.2 | Acceptable | Bad | Independent | Independent | |
| 17 | Female | 85 | A3.3 | Good | Bad | One aid | Frame |
Attempts were made to stabilize preexisting conditions before surgery. Local nerve blockade anesthesia was applied. All operations were performed and completed by the same associate professor using C-arm fluoroscopy. The fractures were reduced using an orthopedic traction bed. Traction and rotation, when needed, were used with the posterior reduction device to achieve and maintain reduction during the surgical procedure, as observed in the anteroposterior and lateral views.
EthicsThis observational and retrospective study was approved by the ethics committee of the Southwest Hospital, the Third Military Medical University, 30 Gao-tan-yan Street, Shapingba District, Chongqing, China.
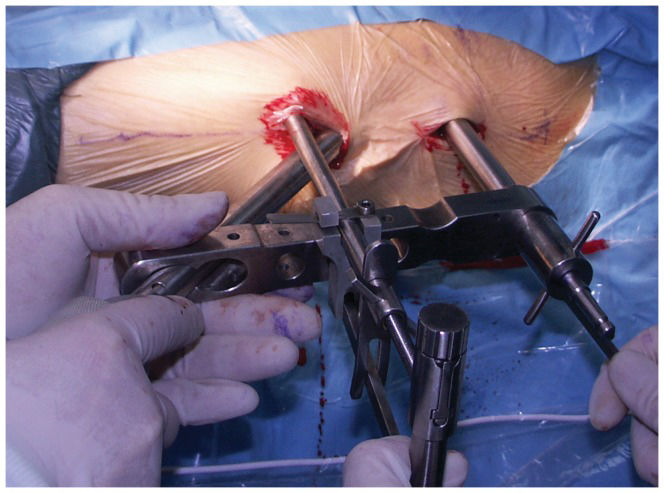
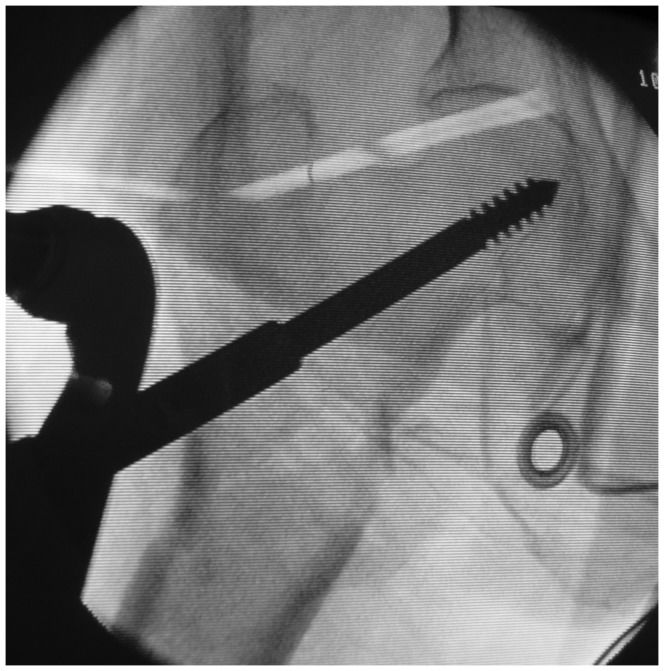
Surgical techniqueAfter basic fracture reduction, the PCCP was inserted with a 2-cm skin incision. After adjusting the plate position, the first neck screw was inserted into the appropriate position in the femoral neck, with the entrance point avoiding the fracture line (to avoid splitting and re-displacement in the proximal fracture when drilling) (Figures1) and 2). Then, three shaft screws were fixed through the second incision. Finally, the second neck screw was placed in the same way as the first screw. The wound was irrigated and closed without the use of a suction drain.
Intraoperative photograph of one patient. The PCCP was inserted in a submuscular manner and temporarily fixed with a butterfly pin and percutaneous bone hook to the femur via the proximal and distal incisions, respectively. The main sleeve was brought through one of the oblique holes in the proximal plate.
Antibiotics were applied for 3-5 days postoperatively, and anticoagulant therapy was not administered before or after surgery. After an X-ray examination was performed on the second postoperative day, the patients were encouraged to perform functional exercises with the affected limb. Touchdown weight-bearing with the help of crutches or a frame began two weeks after the surgery. One month after the surgery, progressive weight bearing was encouraged as tolerated. Full weight bearing was encouraged 3 months after surgery, based on evidence of callus formation on radiographs. The patients were examined clinically and radiographically with a minimum follow-up period of 12 months.
Clinical assessmentThe operation time, perioperative blood loss, occurrence of medical complications, length of stay in the hospital, and preoperative functional activity status were recorded. Complications such as pain, particularly in the thigh, protrusion or cutouts of the neck screw, collapse of the fracture, head penetration, malunion and nonunion were recorded. The functional assessment of the affected limb was based on the Harris hip score (22), with possible ratings of excellent (90–100 points), good (80–89 points), fair (70–79 points), or poor (<70 points).
Radiographic assessmentPostoperative radiographs were assessed to determine fracture reduction and the position of the neck screw. The reduction was regarded as acceptable if there was no significant varus malalignment of the proximal fragment or if there was less than 10 mm of translation between the main fragments (23). The optimal position of the neck screw (17,24) was in the center or the distal third of the femoral neck on the anteroposterior view and in the middle third of the femoral neck on the lateral view. Fractures were judged to be healed radiographically if bridging callus was evident on three of four cortices, as observed on two anteroposterior and lateral views (1). A deviation of the neck-shaft angle of more than 15° was defined as malunion.
Statistical analysisThe data were analyzed using the SPSS 13.0 statistical software package (SPSS Inc., Chicago, IL, USA). Age, operation time, blood loss, and Harris hip scores were compared between the groups by independent t-tests. Patient gender and quality of the reduction were compared using Fisher's exact tests. A two-tailed value of p<0.05 was considered statistically significant.
RESULTSNo deaths occurred during the perioperative period. The mean operating time was 41.5 (26-73) min, the mean intraoperative blood loss was 41.3 (10-80) ml, and the mean hospital stay was 8.5 (5-14) days. Based on the preoperative X-rays, one patient was diagnosed with a type 31-A2 fracture, which was confirmed as type 31-A3 after the intraoperative reduction. The medical complication of popliteal vein thrombosis occurred in one patient, and no other medical complications occurred in the remaining 16 cases.
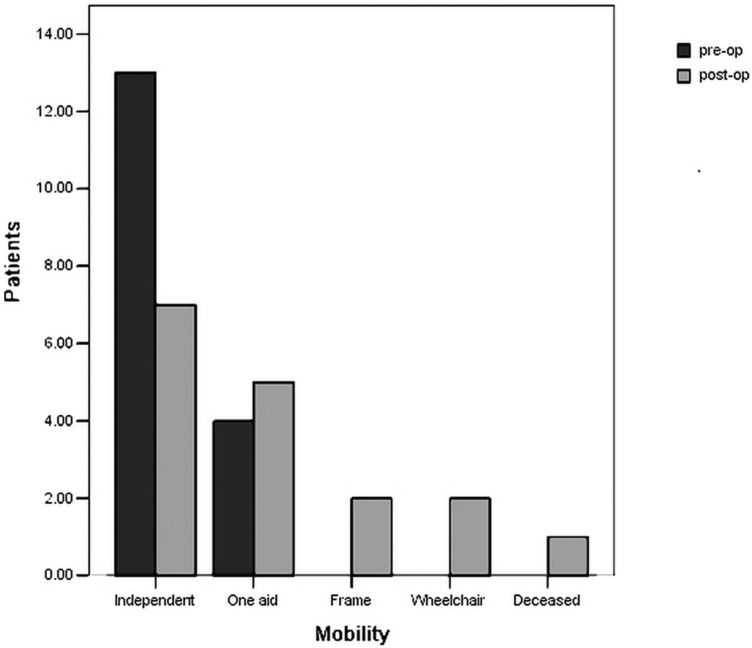
Clinical outcomesOne patient died of a lung infection after 25 postoperative days. Sixteen patients attended the follow-up examinations for a minimum of 12 months. The mean follow-up period was 14 (12–21) months. There were no occurrences of nonunion or reoperation. Pain was absent in 12 patients, mild in 2 patients, and moderate in 2 patients (Table1). According to the Harris hip score, 6 patients had excellent results, 6 had good results, 2 had fair results, and 2 had poor results. The mean Harris hip score of the last follow-up was 84.1 (61-97). Additionally, the mobility of 8 patients basically recovered to the preoperative level, and that of the remaining 8 patients decreased to different extents. Two patients, who suffered collapse of the fracture, depended on a wheelchair. As expected in a group of elderly patients, mobility was reduced after the surgery (Figure3).
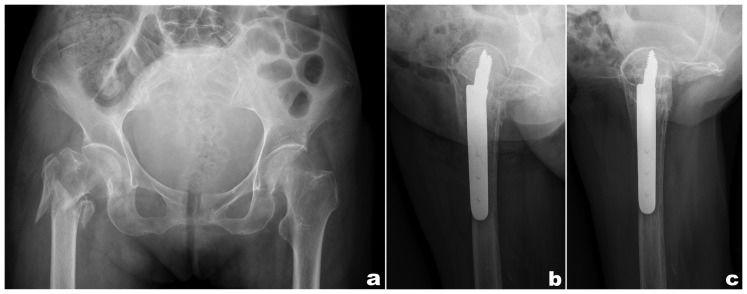
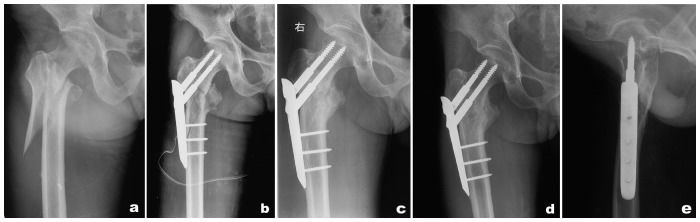
Radiographic outcomesAccording to the definition of the quality of the reduction, 9 patients showed good reduction, 4 had an acceptable reduction, and 4 had a poor reduction, with a bad position of the neck screw found in 5 patients (Table1). Imaging follow-ups were conducted in 16 cases, with complete imaging data (including preoperative, postoperative, and final follow-up X-rays). All patients achieved fracture unions without additional procedures. Two patients had a malunion, with femoral neck-shaft angles with varus deformities being greater than those of the contralateral sides by 15°. Two patients had a loosening of the sleeve of the neck screw, and three patients had protrusion of the neck screw. Collapse of the fracture occurred in two patients, with one having head penetration (Figure4). The initial and follow-up radiographs of a sample case are presented in Figure5.
A 72-year-old female patient with a type 31-A3.3 fracture. A) Initial radiograph. B) Lateral radiograph of the proximal femur at the 6th postoperative week. C) Lateral radiograph of the proximal femur at the 12th postoperative month showing the head penetration of the proximal neck screw.
The initial and follow-up radiographs of a sample case. A) Initial radiograph. B) Radiograph 1 day postoperatively. C) Anteroposterior radiograph at 10 months postoperatively demonstrating the fracture healing. D, E) Anteroposterior and lateral radiographs at 21 months postoperatively showing the fracture healing with no obvious changes in the proximal femur.
We also attempted to identify the factors predictive of pain or fracture collapse following minimally invasive osteosynthesis with the PCCP. Factors such as age, gender, operation time, blood loss, and quality of the reduction were analyzed. Although the factors were compared between patients with and without pain (Table2), those patients with a poor quality of the reduction were more likely to experience pain (p =0.001). No significant difference existed in the presence of a poor quality of the reduction between the groups with and without fracture collapse, whereas a trend existed toward the presence of a poor quality of reduction (p =0.05) in the fracture collapse group (Table3). Furthermore, we found that patients with poor preoperative mobility were more likely to have a lower Harris hip score (p =0.000) (Table4).
Factors that may be predictive of a ‘‘pain“ result.
| Pain-absent (N = 12) | Pain (N = 4) | p-value | |
|---|---|---|---|
| Age (years) | 76.1±15.3 | 82.3±7.3 | 0.458a) |
| Gender (female) | 9 (75%) | 3 (75%) | 1.000b) |
| Operation time (min) | 41.3±11.0 | 41.7±5.9 | 0.933a) |
| Blood loss (ml) | 37.9±17.2 | 50.0±21.6 | 0.271a) |
| Quality of reduction (poor) | 0 (0%) | 4 (100%) | 0.001b) |
a Analyzed using the independent t-test.
Factors that may be predictive of a ‘‘collapse of fracture“ result.
| No collapse of fracture (N = 14) | Collapse of fracture (N = 2) | p-value | |
|---|---|---|---|
| Age (years) | 77.7±14.7 | 77.0±7.1 | 0.948a) |
| Gender (female) | 10(71.4%) | 2(100%) | 1.000b) |
| Operation time (min) | 40.9±10.2 | 45.0±7.1 | 0.594a) |
| Blood loss (ml) | 38.9±16.2 | 55.0±35.4 | 0.263a) |
| Quality of reduction (poor) | 2 (14.3%) | 2 (100%) | 0.05b) |
a Analyzed using the independent t-test.
Preoperative mobility is predictive of the Harris hip score.
| Independent (N = 13) | One aid (N = 3) | p-value | |
|---|---|---|---|
| Harris hip score | 87.0±9.8 | 78.1±7.9 | 0.000a) |
a Analyzed using the independent t-test.
AO/OTA 31-A3 intertrochanteric femoral fractures have unique anatomical and biomechanical characteristics, with the major fracture line running from distal-lateral to proximal-medial. When an SHS is used for fixation, the fracture line is almost parallel to the orientation of the neck screw, and the effect of sliding compression can contrarily cause a lateral displacement of the proximal fracture, leading to protrusion of the neck screw. Meanwhile, a proximal fracture can easily split during drilling because the integrity of the lateral wall of the femur is destroyed and the entrance point of the neck screw is located just at the fracture line. Haidukewych et al. (1) reported that the failure rate was as high as 56%.
The internal fixation treatment with an intramedullary nail for these fractures involves central fixation and theoretically provides better biomechanical stability (25). Kokoroghiannis et al. (26) considered intramedullary devices to be more appropriate for the very unstable AO31-A3 fractures. Although such devices have mechanical advantages in theory, the reported failure rates of intramedullary nails when used to treat these fractures vary greatly due to the different numbers of clinical cases (4,5,23,27-29). Some unstable proximal femoral fractures (7,8) are difficult to fix with an intramedullary nail. Additionally, intramedullary fixation is associated with a large amount of hidden blood loss (30), with no significant difference in the soft tissue damage compared with extramedullary fixation (31). Thus, the use of intramedullary nails is not considered to be a genuine minimally invasive treatment. Although the technology of the intramedullary nail has been continuously improved, the systematic review by Norris et al. (32) reported that the incidence of a second fracture after internal fixation with an intramedullary nail was approximately 1.7%.
Hip fractures involve a complex coupling of fragile patients with fragile bones, which an ideal treatment method should be able to address. Gotfried (17) believed that the application of the PCCP could meet these requirements. The PCCP consists of one steel plate, two neck screws, and three cortical bone screws. Closed reduction is applied during surgery. The proximal fracture is fixed by two neck screws with rotational stability; meanwhile, these screws are placed in a parallel direction to restrict the lateral displacement of the fragments in the proximal fracture, yielding more biomechanical advantages than the SHS (33). The diameters of the two neck screws (7.2 mm) in the PCCP are smaller than those of the SHS. The small diameter and gradual drilling can protect the lateral wall and reduce the occurrence of an intraoperative split or postoperative fracture collapse (10,13).
In our study, the mean operating time was 41.5 (26-73) min, and the mean perioperative blood loss was 41.3 (10-80) ml. These outcomes demonstrated that the PCCP has the advantage of being minimally invasive in the treatment of type A3 fractures. The short operation time and low perioperative blood loss associated with this method are extremely important in elderly patients in whom other diseases may take precedence, thereby requiring rapid fracture fixation. All patients achieved fracture unions without the use of additional procedures. The mean Harris hip score obtained during the last follow-up was 84.1 (61-97). Although the results were satisfactory, there were some orthopedic complications in our study. The sleeve of the neck screw was loose in two cases. This complication may have been due to a technical problem where the screw was not tightened between the sleeve and plate in some patients, causing the gradual loosening of the sleeve from the plate. Protrusion of the neck screw occurred in three cases. The cause of this protrusion is most likely the shearing force caused by the tendency for a lateral displacement of the proximal end and a medial displacement of the distal end in type A3 fractures. However, these complications did not affect the fracture healing, demonstrating that dual axial fixation of the PCCP can effectively control the lateral displacement of the fragments in proximal fractures. Because of poor intraoperative reduction, four patients had pain (p =0.001). Two patients had malunion, with a varus malalignment of the proximal fragment. However, the X-rays obtained during follow-up showed fracture healing. These two patients had the capability to perform normal activities in daily life. Collapse of the fracture occurred in two patients and led to head penetration in one patient. This complication may have been due to poor reduction of the fracture (p =0.05). Furthermore, both of these patients were older than 60 years old and had severe osteoporosis. Two patients depended on a walker frame because they all also had sequelae of cerebrovascular disease and depended on a walking aid before the surgery (p =0.000).
According to existing studies, for AO/OTA 31-A3 intertrochanteric femoral fractures, regardless of intramedullary or extramedullary fixation, fracture reduction and the implant placement position are the two key factors affecting the efficacy of the surgery(1,4-6,23,34). A poor reduction of the fracture and a bad position of the neck screw are important causes of fixation failure. However, based on a retrospective study of 101 cases with reverse obliquity and transverse fractures of the trochanteric region of the femur, Brammar et al. (35) found that the incidence of screw cut-out was independent of the degree of fracture reduction and the position of the neck screw in cases of either intramedullary or extramedullary fixation. They attributed this result to the small number of cases with cut-out failure. Based on the results of our clinical observation and follow-up, the reduction, reduction maintenance, and placement of the neck screw during the surgical procedure are the key steps for a successful surgery in the PCCP treatment of AO/OTA 31-A3 intertrochanteric femoral fractures. The dual axial fixation of the device, which contributes to rotational stability and thus provides controlled fracture impaction, has a strong anti-cut-out ability. The occurrence of the lateral displacement of the fragments in the proximal fracture and coxa vara was effectively controlled if the fracture achieved good reduction. In this study, varus malunion and collapse of the fracture occurred in four patients because of poor reduction. The two neck screws were placed in an orderly manner, with the goal of avoiding the fracture line as much as possible. Progressive drilling with a small-diameter drill bit ranging from 7.0-9.3 mm was performed. This protocol is important to prevent the splitting and re-displacement of the proximal fragment during the drilling process. The optimal position of the neck screw was in the center or the distal third of the femoral neck on the anteroposterior view and in the middle third of the head on the lateral view. In this study, the position of the neck screw was not good in five cases, which may be attributed to poor reduction in two cases and the entrance point avoiding the fracture line during the placement of the first neck screw in the other three cases. For these patients with poor reduction and/or a bad neck screw position, functional exercise in the early postoperative period and weight bearing in the later period is an effective method to avoid complications.
Undoubtedly, this study also had some limitations. First, because of the absence of a control group, the results of the retrospective study remain to be further confirmed by prospective randomized controlled trials. Second, the number of cases was small because of the low morbidity of these fractures, making a significant conclusion between the occurrence of fracture collapse and the quality of the reduction difficult. Third, the follow-up period was short, and the long-term outcomes need to be evaluated through observations during a further follow-up.
According to the results of this study, the PCCP is an alternative device treatment for AO/OTA 31-A3 intertrochanteric femoral fractures. Good fracture reduction and an ideal placement position of the neck screw are important in the success of the device. Furthermore, the preoperative mobility of patients is also an important factor in postoperative functional recovery. Although fracture collapse occurred in two patients, this outcome could be improved by anatomic reduction and a more accurate placement of the neck screw in the femoral head.
AUTHOR CONTRIBUTIONSXie Z and Xu JZ conceived and designed the study. Shen J and Luo F wrote the manuscript. Luo F and Huang Q participated in data management and performed the statistical analysis. Xie Z performed the operations. Dong SW critically commented on the manuscript. All authors read and approved the final version of the manuscript.
No potential conflict of interest was reported.