A 20-year-old woman attended the emergency room reporting anxiety, palpitations, orthopnea, and paroxysmal nocturnal dyspnea for the previous three days. She had no lower limb edema or decreased urine output. No headache, excess sweating, or infection was reported either. The patient's history included type IIb von Hippel–Lindau disease (VHL), with bilateral amaurosis secondary to multiple retinal angiomas since 14 years of age. Syndrome screening and monitoring was not performed because the patient refused to return for regular visits for personal reasons.
Clinical examination showed a fair general status. BP 125/70mmHg; HR 120bpm; SatO2 96% (FiO2 21%); temperature 36.5°C. Cardiac auscultation found rhythmic sounds, with grade IV/VI panfocal systolic murmur, more audible in mitral focus and irradiating to axilla. The rest of the systematic examination was normal.
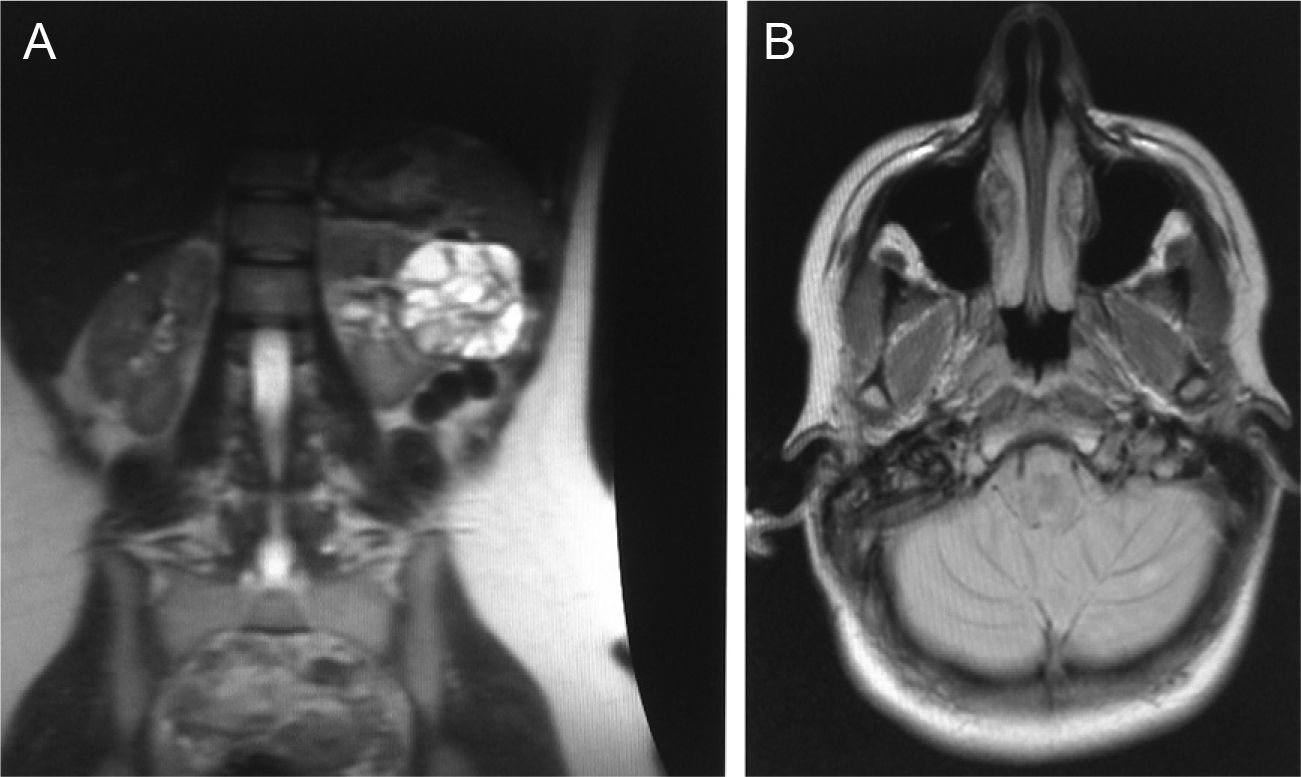
An electrocardiogram revealed sinus tachycardia at 120bpm, with no impaired atrioventricular or intraventricular conduction, nor repolarization changes. A test showed an NTproBNP level of 2948.7pg/mL (normal range (NR): 0–125pg/mL) and a CA 12.5 level of 180.5U/mL (NR 0–35U/mL). These are both markers of congestion with a known prognostic value in heart failure. No remarkable changes were found in any other tested parameters. Thyroid function, lipid profile, and autoimmunity markers were normal. A chest X-ray showed a cardiac silhouette of normal size with bilateral reticular pattern suggesting interstitial edema. After the above findings, a transthoracic echocardiography revealed a slight left ventricular dilation with moderately depressed (45%; NR for age 60%) left ventricular ejection fraction (LVEF) and severe grade IV/VI mitral regurgitation with an apparently normal valve (Fig. 1A).
The patient was diagnosed mitral regurgitation of unknown etiology and admitted to the cardiology department, where beta-blocker and diuretic treatment was started. Dyspnea slightly improved in the first 48h of hospitalization, which improved supine position tolerance. The patient subsequently experienced an attack of anxiety with profuse sweating and palpitations. An electrocardiogram showed sinus tachycardia at 135bpm. Since this was the first clinical episode of mitral regurgitation in a young patient who had shown improvement, a secondary origin was suspected. Tests were therefore requested for autoimmunity and urinary catecholamines, which were positive (vanillylmandelic acid 17.5mg/24h (NR 2.9–11.0mg/24h), total metanephrines 3012.5μg/24h (NR 0–1000μg/24h), normetanephrine 2987.5μg/24h (NR 105–354μg/24h), total catecholamines 657.5μg/24h (NR 217–575μg/24h), norepinephrine 467.5μg/24h (NR 23–105μg/24h), dopamine 177.5μg/24h (NR 190–450μg/24h).
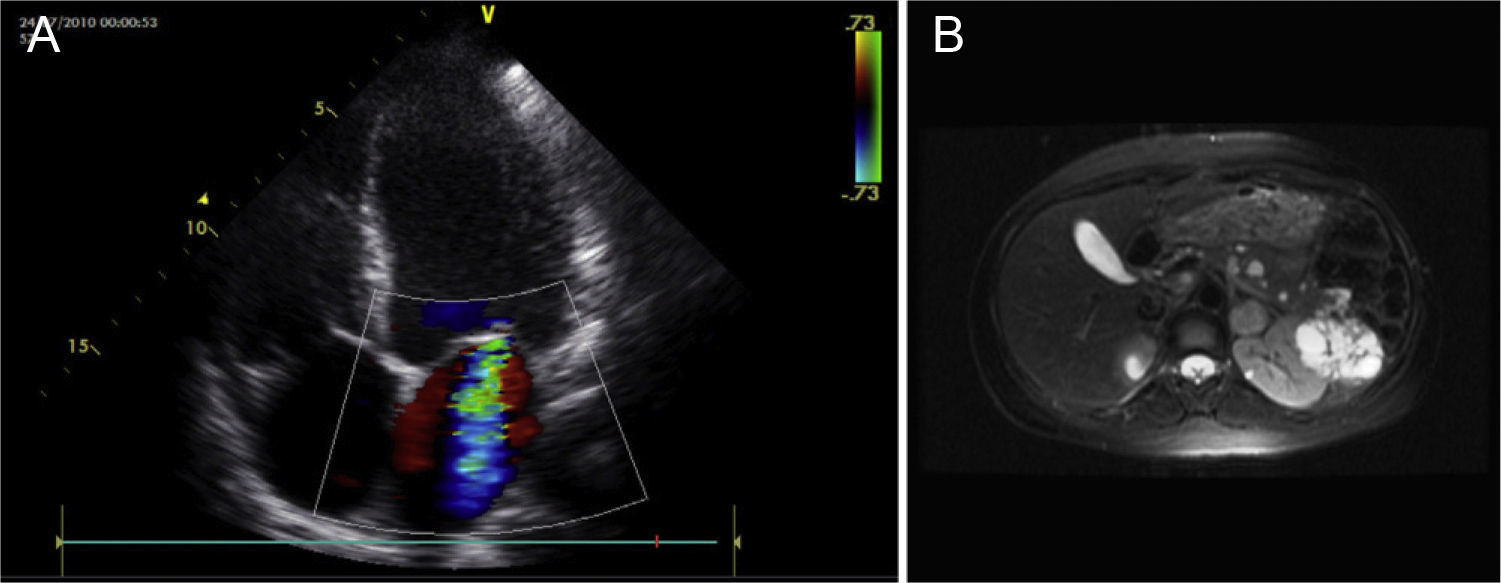
These results suggested pheochromocytoma and justified the clinical picture. Based on this suspected diagnosis in the setting of von Hippel–Lindau syndrome, the patient was referred to the Endocrinology Department. Diagnostic work-up was completed by requesting abdominal and brain MRI. Abdominal MRI revealed a clearly outlined left adrenal mass, 2.3cm in diameter, suggesting pheochromocytoma (Fig. 1B). A heterogeneous cystic tumor, 7.6cm×6.2cm in diameter, was also reported in the left kidney, and multiple formations were seen in the pancreas, with cystic signal in the head, neck, and tail (Fig. 2A). Brain MRI revealed two small high uptake lesions in the left cerebellar hemisphere, a 5-mm lesion and a more peripheral 3-mm lesion, corresponding to cerebellar hemangioblastomas (Fig. 2B). Once imaging diagnosis had been performed, the Urology Department was contacted to plan the surgical approach. Preparation for surgery was started by increasing phenoxybenzamine doses up to 20mg/12h. The patient subsequently experienced palpitations, showing sinus tachycardia which was controlled with propranolol 20mg/12h. Once clinical stability had been achieved, surgery was decided upon. This was performed 20 days later and consisted of radical nephrectomy and adrenalectomy through a laparoscopic approach. The patient experienced no immediate complications and showed an improvement in blood pressure values and palpitations. A pathological study found pheochromocytoma and clear cell renal carcinoma. Postoperative chemistry tests showed a normalization of urinary catecholamines and metanephrines. The patient had no family history of the condition, and genetic analysis by multiplex ligation-dependent probe amplification (MLPA) of leukocyte DNA showed that the patient had a deletion in exon 3 of the VHL gene in heterozygosis, leaving no doubts about her predisposition to VHL syndrome. As there were no affected relatives, it was concluded that this was a de novo mutation. The patient was subsequently admitted to Neurology for hypesthesia in the left half of the body and was diagnosed with intramedullary hemangioblastoma (February 2011) which is being monitored by neurosurgery. The patient currently has no cardiovascular symptoms, and a control echocardiography has shown an absence of mitral regurgitation and normal LVEF.
(A) Transthoracic echocardiography (apical plane 4C). Mitral regurgitation. (B) Abdominal MRI cross-section. Clearly outlined left adrenal mass, 2.3cm in diameter, suggesting pheochromocytoma (marked with red arrow). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of the article.)
VHL syndrome is a genetic disease with an autosomal dominant inheritance. The VHL gene, located in the short arm of chromosome 3 (3p25–26), is affected.1 Only 20% of cases of VHL are familial, and there are therefore a great number of de novo mutations. Signs of disease include retinal (50%), cerebellar, and medullary (39%) hemangiomas, renal cell carcinoma (79%), pheochromocytoma, pancreatic tumors, polycythemia (15%), etc. In this case, the patient had the following signs of the syndrome: multiple retinal angiomas, pheochromocytoma, renal cell carcinoma, and cerebellar and medullary hemangioblastomas. In VHL, the clinical signs of pheochromocytoma are different from those occurring in isolated pheochromocytoma. Annual chemical testing is recommended from 10 years of age in all subjects with VHL for pheochromocytoma screening. The tumor occurrence rate is approximately 10–20%, according to published studies. It should be noted that bilateral tumors occur in up to a half of all cases, although they are rarely malignant. As regards clinical signs and symptoms, up to one third of tumors are diagnosed in their asymptomatic stage. This is due to the monitoring of these patients and because they are tumors with less catecholamine production than sporadic pheochromocytomas.2 Heart involvement may be the main clinical sign of pheochromocytoma and occurs as catecholamine-induced cardiomyopathy, due to the toxic effect of catecholamines and their oxidation products on the myocardium, either direct or mediated through the beta-adrenergic receptor.3 The clinical characteristics of cardiomyopathy related to pheochromocytoma include: arterial hypertension, hypertrophic or dilated cardiomyopathy, heart failure (by a direct effect of catecholamines in the lungs increasing pulmonary capillary permeability and pulmonary venous tone, and damaging pulmonary capillary endothelium), myocardial stunning, ECG changes, cardiac arrhythmia, and cardiac arrest.4 The prognosis of catecholamine-induced cardiomyopathy associated with pheochromocytoma depends on early identification and treatment. Catecholamine-induced cardiomyopathy due to pheochromocytoma should be recognized because its treatment differs from that of other forms of heart failure, and beta-blockers are poorly tolerated. It should also be noted that the myocardium returns to normal within months after treatment. The treatment of choice for pheochromocytoma is surgery after alpha-adrenergic blockade, and was the one used in the reported case.5
Please cite this article as: Caro J, et al. Insuficiencia mitral de etiología desconocida en paciente de 20 años. Endocrinol Nutr. 2012;59:333–5.