Type 2 diabetes mellitus (T2DM) is a chronic, highly prevalent disease that increases with age. Because of this, and due to its chronic complications, T2DM causes high human, social, and financial costs. In addition, the elderly population with T2DM has a marked clinical heterogeneity. Therefore, our main objective was to analyze the relationship of age with the clinical and biological manifestations of the disease and the prevalence of chronic complications in patients with T2DM.
Material and methodsA cross-sectional study of a large population with T2DM (n=405) randomly selected from a Diabetes Unit and 2 health care centers (60%). The clinical, anthropometric, and biochemical variables of the subjects were collected using standard methods to assess the effect of age on the clinical and biochemical phenotype of patients with T2DM.
ResultsWe have noted that patients with T2DM >70 years old have a clinical and biochemical phenotype different from younger subjects (<60 years) including longer times since diabetes onset, higher diastolic blood pressure levels, and lower body mass index (BMI) values. As regards to biological variables, these patients have lower triglyceride levels, impaired kidney function, and lower HbA1c values. Prevalence of metabolic syndrome is lower in patients with T2DM >70 years of age. Age was inversely related to parameters associated to metabolic syndrome (BMI, waist circumference, blood pressure, and triglyceride levels).
ConclusionsWe have defined the clinical and biochemical profile of patients with T2DM >70 years attending health care centers. In addition, the prevalence of stroke, kidney disease, and distal symmetrical polyneuropathy is higher in patients with T2DM >70 years as compared to younger patients (<60 years).
La diabetes tipo 2 (DMT2) es una enfermedad con elevada prevalencia que aumenta con la edad. Por este motivo y por sus complicaciones crónicas genera elevado coste humano, social y económico en la población mayor. Además, la población mayor con DMT2 presenta una marcada heterogeneidad clínica. Por lo que nuestro objetivo principal es conocer cómo se relaciona la edad con el fenotipo clínico-biológico y cuál es la prevalencia de complicaciones crónicas en el paciente con DMT2.
Material y métodosEstudio transversal de una amplia población de DMT2 (n=405) seleccionada de forma aleatoria de una Unidad de Diabetes y 2 centros de salud (60%). En estos sujetos se recogieron variables clínicas, antropométricas y bioquímicas para conocer el efecto de la edad en el fenotipo clínico-biológico de los pacientes con DMT2.
ResultadosHemos observado que los pacientes con DMT2 >70 años presentan un fenotipo clínico y bioquímico diferente al de los sujetos más jóvenes. Se trata de sujetos con mayor tiempo de evolución de la diabetes, mayor valor de la presión arterial diastólica y menor índice de masa corporal (IMC). Con respecto a las variables biológicas, estos sujetos presentan menor valor de triglicéridos, empeoramiento de la función renal y menor valor de HbA1c. La prevalencia de síndrome metabólico es menor en los sujetos con DMT2 >70 años. La edad se relacionó de forma inversa con parámetros relacionados con el síndrome metabólico (IMC, perímetro de cintura, presión arterial y triglicéridos).
La prevalencia de las complicaciones crónicas fue diferente. Así, la prevalencia de accidente cerebrovascular, nefropatía diabética y polineuropatía distal simétrica en la población con DMT2 >70 años fue mayor.
ConclusionesHemos definido el perfil clínico-biológico del paciente con DMT2 > 70 años que acude a centros sanitarios. Los sujetos con diabetes tipo 2 >70 años no presentan el fenotipo de síndrome metabólico observado en los que tienen DMT2 más jóvenes. Además, la prevalencia de accidente cerebrovascular, nefropatía y de polineuropatía distal simétrica es mayor en los pacientes con DMT2 > 70 años.
Type 2 diabetes mellitus (T2DM) is a highly prevalent disease, and its prevalence increases with age. In Spain, the Di@bet.es study estimated that over one half of the population with T2DM was over 65 years of age. In that study, its prevalence in people over 75 years old was 30.7% in males and 33.4% in females, with diagnosis unknown in 10% of cases.1 In our autonomous community, the overall prevalence of diabetes is 14.1%. It is more common in males at all ages, and its prevalence clearly increases with age, reaching 43.7% in people over 80 years of age.2
The increased prevalence and incidence of T2DM with age tends to have a greater social and personal impact on this group of subjects due to chronic complications.3,4 In addition, 75% of worldwide healthcare expense for diabetes in 2013 was incurred for patients aged 50–79 years.5 Moreover, age is a strong predictor of cardiovascular disease in this group of subjects with diabetes.4–6
The elderly population with T2DM has a marked clinical heterogeneity in terms of diabetes presentation and duration, chronic complications, associated comorbidities, functional status, and life expectancy. Thus, it is well known that clinical expressivity in patients with T2DM is low, which makes diagnosis difficult.7,8 Moreover, elderly patients with T2DM without obesity have no increase in glucose production in the liver, and their predominant pathophysiological change is impaired insulin secretion.7,8
On the other hand, elderly subjects with diabetes have a very high risk of hypoglycemia, due in many cases to kidney function impairment and malnutrition, along with many other factors, such as decreased glucagon secretion and an impaired perception of warning symptoms of hypoglycemia.9,10
For these reasons, our hypothesis was that from a clinical and biological viewpoint, disease expression should be different in older diabetic patients as compared to younger subjects. The primary objective of our study was therefore to characterize the clinical and biological phenotype of patients with T2DM over 70 years of age.
There is no agreement as to whether the prevalence of chronic microvascular or macrovascular complications is different in subjects with T2DM over 70 years of age as compared to younger subjects.11 It has been clearly shown, however, that age is a determinant factor in the incidence of chronic complications.11,12 It is also known that cardiovascular mortality is twofold greater in subjects with T2DM >75 years as compared to younger subjects.6,11,12 The available data on the prevalence of chronic microvascular complications are conflicting.12 We therefore thought that it would be interesting to find out whether the prevalence of chronic complications varies with and is related to age. This was the secondary objective of our study.
Subjects and methodsSubjectsOur study sample consisted of 405 patients with T2DM randomly selected among those attending the outpatient clinics of the Department of Endocrinology and Nutrition of Hospital Clínico Universitario in Valencia (Diabetes Unit) and two healthcare centers of our regional Department of Health (60% of the selected subjects). Patient recruitment started in 2009 and ended in 2012. Subjects signed an informed consent to participate in the study which was approved by the ethics committee of our hospital.
All the patients met the inclusion criteria: age over 18 years and diagnosis of T2DM based on basal blood glucose levels ≥126mg/dL (measured twice) or glycosylated hemoglobin (HbA1c) levels ≥6.5%. In addition, they had none of the exclusion criteria: cancer, liver cirrhosis, chronic obstructive pulmonary disease, hypothyroidism, severe heart failure (NYHA>III), systemic diseases, pregnancy, or type 1 diabetes mellitus.
DesignThis was a cross-sectional study of a large population with T2DM to ascertain the impact of age on the clinical and biological phenotype of patients with T2DM, and thus discover whether the clinical and biological phenotype is different in older patients with T2DM as compared to younger subjects with the disease.
MethodsClinical and biological parametersThe clinical parameters were collected by two researchers during visits of patients with T2DM to the outpatient clinics of the hospital (Diabetes Unit) and two primary care centers of our healthcare area.
The variables collected included age, sex, time since disease onset, chronic complications of diabetes, dyslipidemia, high blood pressure, metabolic syndrome, diabetes treatment, smoking, weekly physical activity, the body mass index (BMI), and blood pressure. Metabolic syndrome was defined following the NCEPIII criteria.13
The presence of chronic complications of diabetes was assessed as follows: distal symmetrical polyneuropathy using the Neurological Disability Score (NDS); diabetic retinopathy by eye fundus examination by an ophthalmologist; and nephropathy by three measurements of microalbuminuria. Macroangiopathy was assessed based on a history of acute myocardial infarction, acute coronary syndrome, or stroke, or ankle/brachial index (peripheral vascular disease).
Variables based on physical examination included the BMI, waist circumference, blood pressure, the NDS, and the ankle-brachial index, and were collected by two trained researchers using standardized procedures.
Biochemical variables were measured in peripheral blood (plasma or serum), drawn after a 10-h fast, at the central laboratory of our hospital, and included glucose, HbA1c, total cholesterol, LDL-C, HDL-C, triglycerides, creatinine, urea, albuminuria (to assess diabetic nephropathy), and creatinine clearance with Modification of Diet in Renal Disease (MDRD). Biochemical variables were measured using standardized procedures.
Statistical analysisThe sample was selected by simple randomized sampling. The sample size was estimated assuming differences between subjects <60 years and >70 years greater than 25% for an alpha error of 5% and a beta error of 20%. The estimated sample was at least 110 subjects by group.
A Student's t test for unpaired data was used to compare quantitative variables between the groups (subjects <60 years versus subjects >70 years), while contingency tables and a Chi-square test were used for qualitative variables.
To ascertain the relations between variables with age, a simple regression study was used, and an exploratory factorial analysis was performed.
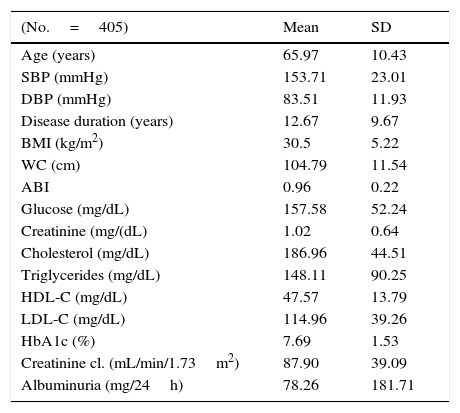
ResultsTable 1 shows the main clinical and biological variables of the 405 subjects with T2DM studied.
Clinical and biological characteristics of subjects with type 2 diabetes studied.
| (No.=405) | Mean | SD |
|---|---|---|
| Age (years) | 65.97 | 10.43 |
| SBP (mmHg) | 153.71 | 23.01 |
| DBP (mmHg) | 83.51 | 11.93 |
| Disease duration (years) | 12.67 | 9.67 |
| BMI (kg/m2) | 30.5 | 5.22 |
| WC (cm) | 104.79 | 11.54 |
| ABI | 0.96 | 0.22 |
| Glucose (mg/dL) | 157.58 | 52.24 |
| Creatinine (mg/(dL) | 1.02 | 0.64 |
| Cholesterol (mg/dL) | 186.96 | 44.51 |
| Triglycerides (mg/dL) | 148.11 | 90.25 |
| HDL-C (mg/dL) | 47.57 | 13.79 |
| LDL-C (mg/dL) | 114.96 | 39.26 |
| HbA1c (%) | 7.69 | 1.53 |
| Creatinine cl. (mL/min/1.73m2) | 87.90 | 39.09 |
| Albuminuria (mg/24h) | 78.26 | 181.71 |
Creatinine cl.: creatinine clearance; SD: standard deviation; HbA1c: glycosylated hemoglobin; HDL: high density lipoprotein cholesterol; BMI: body mass index; ABI: ankle/brachial index; LDL: low density lipoprotein cholesterol; WC: waist circumference; DBP: diastolic blood pressure; SBP: systolic blood pressure.
To ascertain the impact of age on the different variables, subjects with T2DM <60 years (n=110) were compared to those >70 years of age (n=112). No analysis was made of subjects aged 60–70 years.
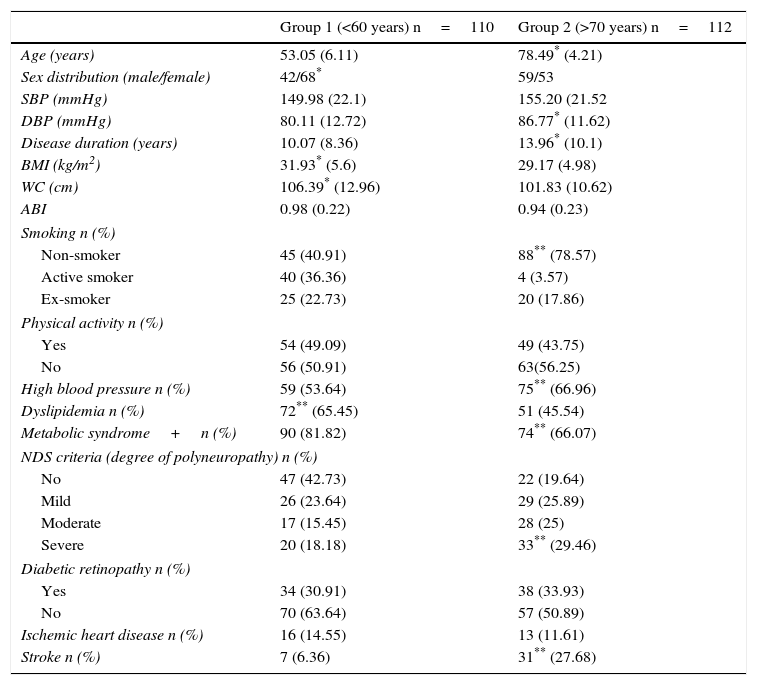
A comparison of clinical and anthropometric variables (Table 2) in subjects aged <60 years versus patients over 70 years of age showed significant differences in sex distribution (68 vs 53 females), diastolic blood pressure (80.11±12.72mmHg vs 86.77±11.62mmHg), diabetes duration (10.07±8.36 years vs 13.96±10.1 years), the BMI (31.93±5.62kg/m2 vs 29.17±4.98kg/m2), waist circumference (106.39±12.96cm vs 101.83±10.62cm), smoking (45 vs 88 non-smokers), the prevalence of high blood pressure (59 vs 75 subjects), and dyslipidemia (72 vs 51 subjects).
A comparison of clinical characteristics, anthropometric parameters, and the prevalence of chronic complications in the group of subjects with T2DM under 60 years of age (group 1) and over 70 years of age (group 2).
| Group 1 (<60 years) n=110 | Group 2 (>70 years) n=112 | |
|---|---|---|
| Age (years) | 53.05 (6.11) | 78.49* (4.21) |
| Sex distribution (male/female) | 42/68* | 59/53 |
| SBP (mmHg) | 149.98 (22.1) | 155.20 (21.52 |
| DBP (mmHg) | 80.11 (12.72) | 86.77* (11.62) |
| Disease duration (years) | 10.07 (8.36) | 13.96* (10.1) |
| BMI (kg/m2) | 31.93* (5.6) | 29.17 (4.98) |
| WC (cm) | 106.39* (12.96) | 101.83 (10.62) |
| ABI | 0.98 (0.22) | 0.94 (0.23) |
| Smoking n (%) | ||
| Non-smoker | 45 (40.91) | 88** (78.57) |
| Active smoker | 40 (36.36) | 4 (3.57) |
| Ex-smoker | 25 (22.73) | 20 (17.86) |
| Physical activity n (%) | ||
| Yes | 54 (49.09) | 49 (43.75) |
| No | 56 (50.91) | 63(56.25) |
| High blood pressure n (%) | 59 (53.64) | 75** (66.96) |
| Dyslipidemia n (%) | 72** (65.45) | 51 (45.54) |
| Metabolic syndrome+n (%) | 90 (81.82) | 74** (66.07) |
| NDS criteria (degree of polyneuropathy) n (%) | ||
| No | 47 (42.73) | 22 (19.64) |
| Mild | 26 (23.64) | 29 (25.89) |
| Moderate | 17 (15.45) | 28 (25) |
| Severe | 20 (18.18) | 33** (29.46) |
| Diabetic retinopathy n (%) | ||
| Yes | 34 (30.91) | 38 (33.93) |
| No | 70 (63.64) | 57 (50.89) |
| Ischemic heart disease n (%) | 16 (14.55) | 13 (11.61) |
| Stroke n (%) | 7 (6.36) | 31** (27.68) |
Creatinine cl.: creatinine clearance; BMI: body mass index; ABI: ankle/brachial index; WC: waist circumference; SBP: systolic blood pressure; DBP: diastolic blood pressure; NDS: neurological disability score.
The prevalence of chronic complications of diabetes was significantly different (Table 2): subjects >70 years showed a greater prevalence of stroke (6.36% vs 27.68%) and severe distal symmetrical polyneuropathy (18.18% vs 29.46%).
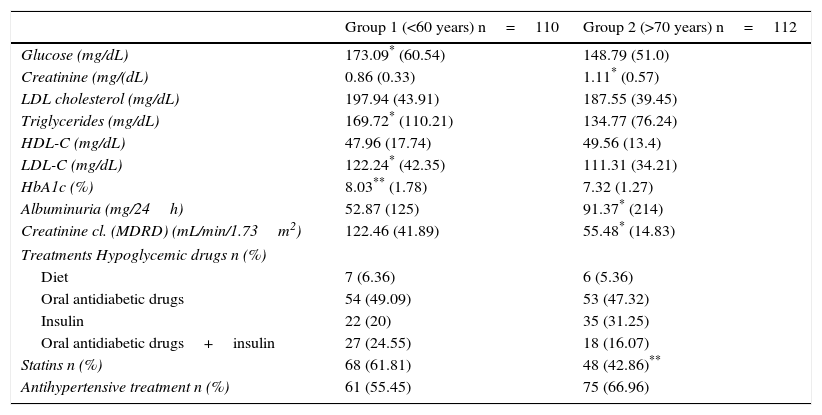
A comparison of biological variables between the two groups (Table 3) showed statistically significant differences in basal blood glucose (173.09±60.54mg/dL vs 148.79±51mg/dL), creatinine (0.86±0.33mg/dL vs 1.11±0.57mg/dL), triglycerides (169.72±110.21mg/dL vs 134.72±76.24mg/dL), LDL-C (122.24±42.35mg/dL vs 111.31±34.21mg/dL), HbA1c (8.03±1.78% vs 7.32±1.27%), albuminuria (52.87±125mg/24h vs 91.37±214mg/24h), and creatinine clearance (MDRD: 122.4±41.89mL/min/1.73m2 vs 55.5±14.83mL/min/1.73m2).
A comparison of biochemical parameters and treatments between subjects with T2DM under 60 years of age (group 1) and over 70 years of age (group 2).
| Group 1 (<60 years) n=110 | Group 2 (>70 years) n=112 | |
|---|---|---|
| Glucose (mg/dL) | 173.09* (60.54) | 148.79 (51.0) |
| Creatinine (mg/(dL) | 0.86 (0.33) | 1.11* (0.57) |
| LDL cholesterol (mg/dL) | 197.94 (43.91) | 187.55 (39.45) |
| Triglycerides (mg/dL) | 169.72* (110.21) | 134.77 (76.24) |
| HDL-C (mg/dL) | 47.96 (17.74) | 49.56 (13.4) |
| LDL-C (mg/dL) | 122.24* (42.35) | 111.31 (34.21) |
| HbA1c (%) | 8.03** (1.78) | 7.32 (1.27) |
| Albuminuria (mg/24h) | 52.87 (125) | 91.37* (214) |
| Creatinine cl. (MDRD) (mL/min/1.73m2) | 122.46 (41.89) | 55.48* (14.83) |
| Treatments Hypoglycemic drugs n (%) | ||
| Diet | 7 (6.36) | 6 (5.36) |
| Oral antidiabetic drugs | 54 (49.09) | 53 (47.32) |
| Insulin | 22 (20) | 35 (31.25) |
| Oral antidiabetic drugs+insulin | 27 (24.55) | 18 (16.07) |
| Statins n (%) | 68 (61.81) | 48 (42.86)** |
| Antihypertensive treatment n (%) | 61 (55.45) | 75 (66.96) |
Creatinine cl.: creatinine clearance; HbA1c: glycosylated hemoglobin; HDL: high density lipoprotein cholesterol; LDL: low density lipoprotein cholesterol.
As regards the treatments used to control diabetes (Table 3), statistically significant differences were found in the use of statins (greater in subjects <60 years) despite the fact that LDL-C goals were not reached, and no differences were seen in antihypertensive or hypoglycemic treatment.
In the whole group of study subjects with T2DM (n=405), age was statistically related (p<0.05) to diastolic blood pressure (r=0.225), BMI (r=−0.178), diabetes duration (r=0.195), creatinine (r=0.191), total cholesterol (r=−0.101), triglycerides (r=−0.136), HbA1c (−0.154), creatinine clearance (kidney function (r=−0.683), HBP (r=0.106), and distal symmetrical polyneuropathy (NDS criteria, r=0.194).
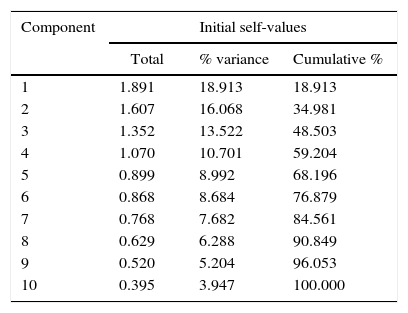
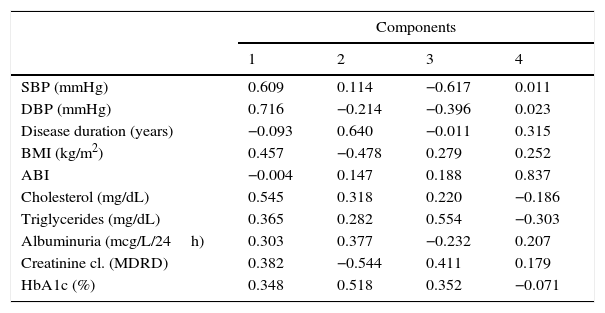
An exploratory factorial analysis (Table 4 and Table 5) was conducted to see whether the variables which characterize the person with diabetes are grouped in different components in the study sample of 405 patients with T2DM. The KMO measure of sampling adequacy was 0.536, with a significance of p<0.001. The total variance explained was significantly explained by four components, as shown in Table 4. Table 5 shows the matrix of such components. In component 1, subjects with high blood pressure, obesity, and elevated cholesterol and triglyceride levels predominate. In component 2, subjects with longer disease duration and lower HbAc, BMI, and renal clearance predominate. Component 3 consists of patients with low systolic blood pressure and elevated triglyceride levels, and component 4 consists of subjects with no macroangiopathy as assessed through the ankle/brachial index.
Exploratory factorial analysis of the study sample of subjects with T2DM (n=405). Total variance explained.
| Component | Initial self-values | ||
|---|---|---|---|
| Total | % variance | Cumulative % | |
| 1 | 1.891 | 18.913 | 18.913 |
| 2 | 1.607 | 16.068 | 34.981 |
| 3 | 1.352 | 13.522 | 48.503 |
| 4 | 1.070 | 10.701 | 59.204 |
| 5 | 0.899 | 8.992 | 68.196 |
| 6 | 0.868 | 8.684 | 76.879 |
| 7 | 0.768 | 7.682 | 84.561 |
| 8 | 0.629 | 6.288 | 90.849 |
| 9 | 0.520 | 5.204 | 96.053 |
| 10 | 0.395 | 3.947 | 100.000 |
Main components of the factorial analysis of study subjects with T2DM (n=405). Matrix of the 4 components extracted.
| Components | ||||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| SBP (mmHg) | 0.609 | 0.114 | −0.617 | 0.011 |
| DBP (mmHg) | 0.716 | −0.214 | −0.396 | 0.023 |
| Disease duration (years) | −0.093 | 0.640 | −0.011 | 0.315 |
| BMI (kg/m2) | 0.457 | −0.478 | 0.279 | 0.252 |
| ABI | −0.004 | 0.147 | 0.188 | 0.837 |
| Cholesterol (mg/dL) | 0.545 | 0.318 | 0.220 | −0.186 |
| Triglycerides (mg/dL) | 0.365 | 0.282 | 0.554 | −0.303 |
| Albuminuria (mcg/L/24h) | 0.303 | 0.377 | −0.232 | 0.207 |
| Creatinine cl. (MDRD) | 0.382 | −0.544 | 0.411 | 0.179 |
| HbA1c (%) | 0.348 | 0.518 | 0.352 | −0.071 |
Creatinine cl.: creatinine clearance; BMI: body mass index; ABI: ankle/brachial index; DBP: diastolic blood pressure; SBP: systolic blood pressure.
A simple correlation found age to be significantly related to all four components. The relationship was negative with components 1 and 3 (r=−0.330; p<0.001; r=−0.348; p<0.001 respectively) and positive with component 2 (r=0.265; p<0.001) and, to a lesser extent, with component 4 (r=−0.110; p<0.04).
Thus, in the study sample with T2DM, patients with T2DM at an older age have higher blood pressure at the expense of diastolic blood pressure, a lower BMI, and lower total cholesterol and triglyceride levels. For this reason, the prevalence of metabolic syndrome was significantly lower in the group of subjects >70 years as compared to those <60 years (Table 2). In group 1 (<60 years), 90 out of the 110 subjects had metabolic syndrome. In group 2 (>70 years), 74 out of 112 subjects had metabolic syndrome (p=0.017).
DiscussionElderly patients with T2DM have a marked clinical heterogeneity. Understanding the clinical and biological characteristics of this group of patients is therefore necessary if they are to be adequately characterized.7,8 These patients are also affected by factors that modulate the disease, including comorbidities, geriatric syndromes, treatment with multiple drugs, situations of dependence and social isolation, a high risk of hypoglycemia, and nutritional problems.7,8 Consequently, it is necessary to conduct an integral clinical, biological, functional, and cognitive assessment in elderly patients with T2DM both to improve their care and to establish individualized therapeutic goals.9,10 The results of our study show that patients with T2DM >70 years of age have clinical and biological characteristics and prevalence rates of chronic complications different from those of diabetic patients <60 years.
Thus, diabetic patients over 70 years have a lower prevalence of metabolic syndrome. In addition, they show a significantly lower BMI, waist circumference, and triglyceride, LDL-C, and HbA1c levels. Data similar to those collected in our study have been reported by other authors, who found that patients with T2DM over 80 years of age had lower waist circumference and HbA1c, triglyceride, and LDL-C levels as compared to patients who were younger, but over 60.14
These results may be explained by the distinction made in our study between elderly patients with T2DM recently diagnosed (with disease starting after 65 years of age) and those with long-standing diabetes starting at or before middle age. Elderly subjects with longer disease duration, such as our study patients, have a decreased function of the pancreatic islets.15 Age contributes to pancreatic beta cell dysfunction. Insulin secretion decreases with age, even in people with normal glucose tolerance, probably because of the decrease in pancreatic beta mass and the proliferation capacity of beta cells.16,17 The longer disease duration in patients >70 years of age in our study could explain the greater contribution of insulin secretion as compared to insulin resistance. This factor would partly account for the clinical and biological differences found. Unfortunately, insulin levels were not measured, and the HOMA index could not be calculated in our study in support of this hypothesis. It would also explain the lower prevalence of severe obesity and metabolic syndrome in older subjects with T2DM. Moreover, age-related insulin resistance is associated with greater adiposity, sarcopenia, and physical inactivity.16 Study patients >70 years had the same physical inactivity as those <60 years and a lower BMI and waist circumference, which suggests that impaired insulin secretion is more important in them.
On the other hand, our study showed no differences in the prevalence of chronic complications. Thus, subjects with T2DM >70 years showed a higher prevalence of distal symmetrical polyneuropathy, as measured by NDS, and stroke. A higher prevalence of polyneuropathy may be related to the associated deficiency of nutritional factors in this group of elderly subjects. An additional reason could be that exploratory NDS criteria used in the diagnosis of polyneuropathy may be altered by age, not only by diabetes. Increased stroke prevalence may be explained by the greater prevalence of high blood pressure in the group of subjects >70 years. However, other studies found no difference in the prevalence of chronic microvascular complications in elderly patients with T2DM as compared to younger subjects.12,18
Kidney function impairment is more likely with age, as was shown in our study.19 This accounts for the significant differences in renal clearance found in subjects >70 years as compared to younger patients (<60 years). Interestingly, however, glucose lowering treatment was not significantly different in subjects >70 years, in whom the use of oral antidiabetic drugs was very similar. A trend in insulin use similar to that reported in another study was seen.20 Our results support the need for the different management of blood pressure and glucose control because of the risk of hypoglycemia in elderly subjects with diabetes, as has been shown in different studies and recommendations.9,10 However, this was not shown in our study.
Female prevalence was significantly greater in patients >70 years. In the Valencian Autonomous Community, diabetes has been shown to be more common in males in all age groups, except in subjects over 70 years of age, in whom no sex differences are found, coinciding with an increased prevalence in females.2 These data agree with our analysis.
The main limitation of our study was the survival bias inherent to a cross-sectional study in this population with high cardiovascular risk. An additional limitation is that patient selection was not representative of the population with T2DM, because it was made among subjects diagnosed with the disease who attended healthcare centers, instead of a general population with T2DM. This meant that subjects with unknown diabetes, or elderly subjects with significant geriatric syndromes who were not attending healthcare centers because they were institutionalized or receiving home care were excluded. But even recognizing these limitations, the study provides a lot of significant data collected in standard clinical practice from subjects with T2DM >70 years attending healthcare centers and with no advanced comorbidities.
In conclusion, patients with T2DM >70 have clinical and biological characteristics different from those of subjects with T2DM <60 years. They have a lower BMI and waist circumference, a greater prevalence of high blood pressure, less prevalence of metabolic syndrome, and lower levels of metabolic factors (HbA1c, LDL-C, and triglycerides). These results were also supported by the factorial study, as age was significantly associated with component.2 On the other hand, the prevalence of chronic complications was different, with a greater prevalence of stroke, distal symmetrical polyneuropathy and diabetic nephropathy, with the decrease in kidney function characteristic of their age. It should be noted that, despite this, glucose lowering treatment is not different in subjects with T2DM <60 years as compared to those >70 years.
We think that our findings should have a clinical impact, because they objectively indicate that patients with T2DM >70 years have clinical and biological characteristics different from those of younger patients with the disease. This could imply changes in the management of these subjects, regardless of factors associated with age such as geriatric syndromes, multiple drug use, and dependency found in elderly subjects. Prospective studies are however needed to support our data.
FundingThis study was funded by projects AP-04/06 and AP 068/08 of the Department of Health of the Valencian Government and by CIBERDEM (ISCIII). CIBER of diabetes and associated metabolic diseases (CIBERDEM) is an initiative of Instituto de Salud Carlos III.
Conflicts of interestThere are no conflicts of interest.
Please cite this article as: Basanta-Alario ML, Ferri J, Civera M, Martínez-Hervás S, Ascaso JF, Real JT. Diferencias en las características clínico-biológicas y prevalencia de complicaciones crónicas en relación con el envejecimiento de pacientes con diabetes tipo 2. Endocrinol Nutr. 2016;63:79–86.