Eikenella corrodens (E. corrodens) is a slow-growing, Gram-negative, facultative anaerobic coccobacillus commonly found in the flora of the oral cavity, the upper respiratory tract and the digestive tract. It most often causes head, neck and intra-abdominal infections, as well as endocarditis and human bite infections.1 However, there are very few cases of obstetric and gynaecological infections to be found in the literature.
We present a case of chorioamnionitis and neonatal sepsis caused by E. corrodens.
A 25-year-old woman presented with a dichorionic diamniotic twin pregnancy at 24+3 weeks and was admitted for cervical effacement without having gone into labour. The patient had no relevant medical history and the prenatal screening was normal. On the tenth day of admission, and after premature rupture of membranes, the patient went into spontaneous labour, requiring a Caesarian section as one of the twins was lying transverse. Given that chorioamnionitis was suspected, a placenta sample was sent for microbiological culture and histological examination.
The newborn (800g) presented clinical and biochemical signs of infection. The blood count revealed 4000leukocytes/μl, (9% segmented, 72% lymphocytes and 15% monocytes) and 112,000platelets/μl. C-reactive protein was 5.3mg/dl. A bottle of blood culture was extracted and empirical antibiotic treatment with ampicillin (50mg/kg/dose every 12h) and tobramycin (5mg/kg/dose every 48h) was established.
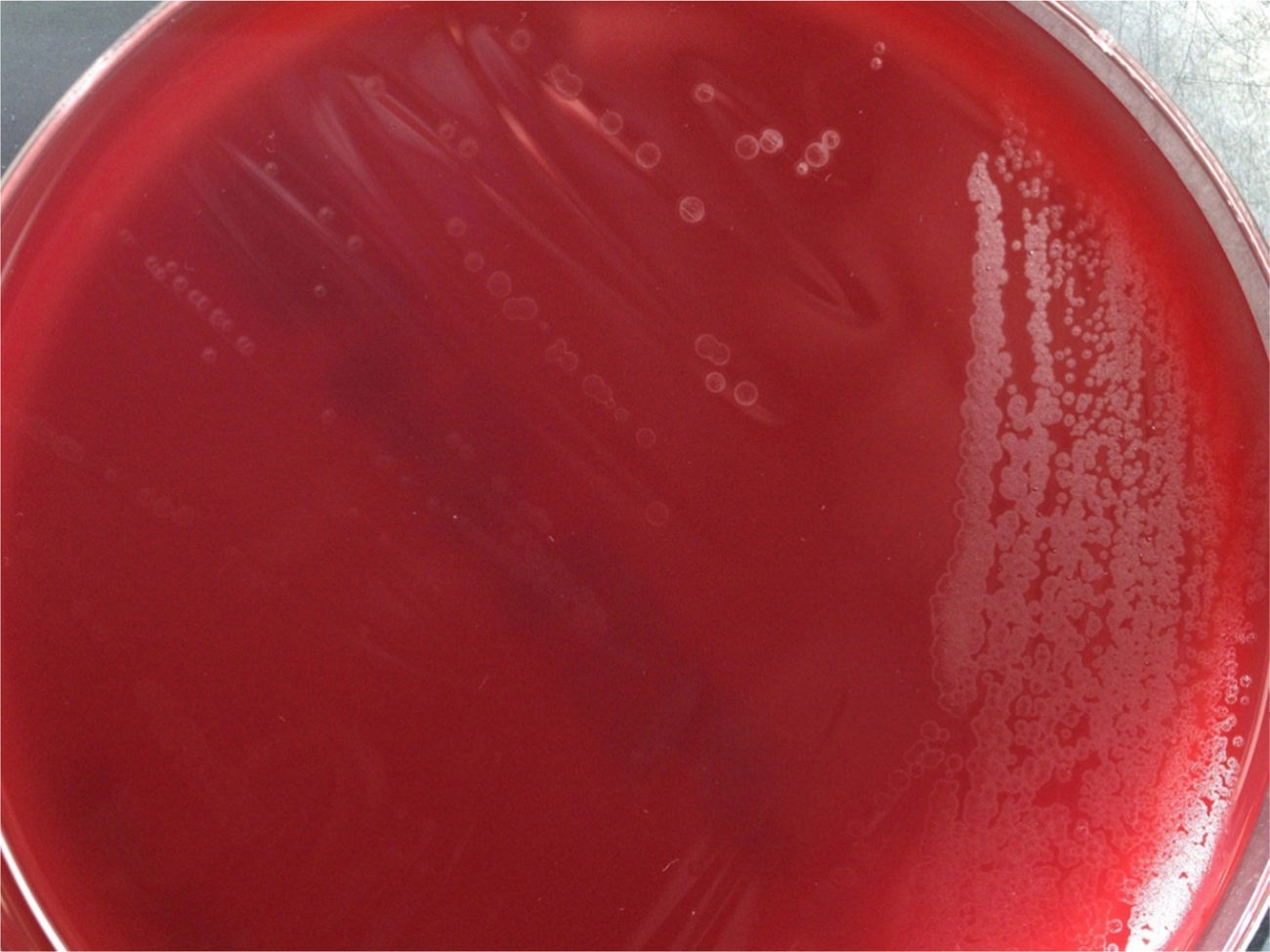
The histological examination of the placenta revealed active sites of chorioamnionitis, and a Gram-negative bacillus was isolated from the microbiological culture after 48h of incubation. The colonies grown in blood agar presented a classic punctiform shape with grey, translucent, non-haemolytic circular borders (Fig. 1). They gave off a characteristic hypochlorite odour and were catalase-negative and oxidase-positive.
The bottle of blood culture was positive after 34h of incubation. After the Gram stain, which revealed Gram-negative coccobacilli, a subculture was prepared in chocolate agar and blood agar at 37°C and 5% CO2. After 24h of incubation, the colonies grown presented the same morphological and biochemical characteristics as the placenta culture. The automated Vitek 2® System (bioMérieux, Spain) was used to identify both microorganisms, but it failed to do so. Presumptive identification was performed using clinical chemistry tests (negative indole, positive ornithine decarboxylase and prolyl arylamidase, no carbohydrate fermentation). Finally, the 16S ribosomal RNA gene was amplified and sequenced, confirming both bacteria to be E. corrodens.
The sensitivity test was performed using antibiotic gradient strips in Müeller-Hinton agar, supplemented with 5% blood and NAD (MH-F, Oxoid). According to the CLSI M45 guidelines,2 the isolated strains were sensitive to penicillin (MIC: 1μg/ml), amoxicillin–clavulanic acid (MIC: 1μg/ml), cefotaxime (MIC: 0.06μg/ml), erythromycin (MIC: 4μg/ml), ciprofloxacin (MIC: 0.006μg/ml), cotrimoxazole (MIC: <0.002μg/ml) and doxycycline (MIC: 1μg/ml), intermediate to gentamicin (MIC: 4μg/ml) and amikacin (MIC: 16μg/ml), and resistant to clindamycin (MIC: >256μg/ml) and metronidazole (MIC: >256μg/ml), consistent with the antibiotic sensitivity described in the bibliography for this microorganism.1
The bacteria E. corrodens has traditionally been included in the so-called HACEK group of slow-growing, fastidious microorganisms, which are made up of the following genera: Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella and Kingella.
Penicillin G or amoxicillin-clavulanic acid are considered the treatment of choice. In our case, after obtaining the antibiogram, intravenous penicillin G was administered (50,000IU/kg/dose every 12h for 7 days), with favourable progression and sterile blood culture at 5 days of life.
Very few cases of neonatal sepsis caused by E. corrodens have been published.3–5 It is usually isolated in mixed infections, in patients with some degree of immunosuppression. In the case presented, E. corrodens chorioamnionitis was caused by genital colonisation of the bacteria during pregnancy, that ascended from the vagina. Some authors have suggested that oral sex during pregnancy may trigger chorioamnionitis by this microorganism.6–9 It is presumed that the neonatal sepsis was vertically transmitted.
Infections caused by E. corrodens may be underestimated because of the bacteria's slow growth and due to the fact that they may be present in mixed infections, thereby hindering their microbiological identification.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Angulo López I, Aguirre Quiñonero A, Fernández Torres M, Alegría Echauri E. Corioamnionitis y sepsis neonatal causada por Eikenella corrodens. Enferm Infecc Microbiol Clin. 2017;35:266–267.