Women sex workers (WSW) are one of key population on the HIV and other sexually transmitted infections (STIs) monitoring and evaluation. Socioeconomic, structural factors and other factors associated with the workplace influence exposure to these infections. The objectives of this study were to describe and compare the social characteristics, risk behaviours and HIV, chlamydia and gonorrhoeae prevalence according to sex work site (street or highway, clubs and flats).
MethodsCross-sectional study on 400 WSW in Catalonia. Socio-demographic, sex work and behavioral characteristics were collected through personal interview. Oral fluid and urine samples were collected to determine STI prevalence.
ResultsWSW that exercised in the street or highway presented more precarious conditions and a greater vulnerability related to socioeconomic factors: older population, with a lower education level and with less economic remuneration for their service. Other factors associated with lifestyle or behaviour was also observed: greater injecting drug use, longer sex work or vulnerabilities associated with structural or social determinants: less access to health services, higher proportion of forced relations and stay in prison. The overall HIV, chlamydia and gonorrhoeae prevalence was 3.0%, 1.8% and 0.5%, respectively and higher in women who exercised on the street or highway, 5.6%, 1.9% and 1.2%, respectively.
ConclusionThe information generated in this study will be useful for the design specific preventive interventions aimed at this group.
Las mujeres que ejercen el trabajo sexual (MTS) son una de las poblaciones clave en la monitorización y evaluación del VIH y otras infecciones de transmisión sexual (ITS). Factores socioeconómicos, estructurales y asociados al ámbito de trabajo influyen en la exposición a estas infecciones. Los objetivos del estudio fueron describir y comparar características sociales, conductas de riesgo y prevalencia del VIH, clamidia y gonococia según lugar de realización del trabajo sexual (calle o carretera, clubs, pisos).
MétodosEstudio transversal en 400 MTS en Cataluña. Se recogieron características sociodemográficas, del trabajo sexual y conductuales mediante entrevista personal y muestras de fluido oral y orina para determinar la prevalencia de ITS.
ResultadosLas MTS que ejercen en la calle o carretera presentaron condiciones más precarias y mayor vulnerabilidad relacionada con factores socioeconómicos: población más envejecida, con nivel de estudios inferior y menor retribución económica por su servicio. Se observaron otros factores asociados al estilo de vida o conductuales: mayor consumo de drogas por vía parenteral, mayor tiempo de trabajo sexual o vulnerabilidades asociadas a una serie de determinantes a nivel estructural o sociales: menor acceso a servicios de salud, mayor proporción de relaciones forzadas y estancia en prisión. La prevalencia global de VIH, clamidia y gonococia fue del 3,0%, 1,8% y 0,5%, respectivamente y superiores en las mujeres que ejercían en la calle-carretera, 5,6%, 1,9% y 1,2%, respectivamente.
ConclusiónLa información generada en este estudio será clave para el diseño de intervenciones preventivas específicas dirigidas a este colectivo.
Traditionally, due to the degree of exposure and the vulnerability factors associated with them, female sex workers (FSWs) have been considered one of the key populations in the monitoring and evaluation of HIV and other sexually transmitted infections (STIs), as well as a priority target population for prevention and control programmes of these infections1. A recent systematic review found a global prevalence of HIV in FSWs of 11.8%, with significant variation according to geographic region2. In Europe, the prevalence remains relatively low, generally not higher than 5%1. Spain also presents low values, which range between 0.2% and 1.8%3–5, slightly higher than the values in the general population.
Traditionally, commercial sex workers have been viewed as a bridging population for the transmission of HIV6. However, in our country, they have been of little relevance with regard to this transmission to the general population, also due to the low prevalence values. However, various national studies have shown higher prevalences for other STIs7, ranging from 4.7% to 5.9% for Chlamydia trachomatis (CT) and 0.6%–3.7% for Neisseria gonorrhoeae (NG)4,8, two of the most prevalent STIs in women and with significant percentages in immigrants. According to the latest data published in Catalonia and following state and European patterns9,10, NG stood at a rate of 51 cases per 100,000 inhabitants, with a rate of 17 cases in women and 34% of diagnoses in immigrants; 12% of cases were co-infected with HIV11. For CT, the rate stood at 72 cases, with 52% of cases in women and 35% in immigrants; 3.7% of the cases were coinfected with HIV11.
Vulnerability in FSWs is fundamentally related to socioeconomic factors, factors associated with lifestyle (alcohol and drug use), as well as structural determinants: limited access to health services, criminalisation, stigma, or sexual and physical violence12–14. On the other hand, and also increasing vulnerability to these infections, there are determinants related to their activity, such as a high number of sexual partners, sex without a condom and other factors associated with their place of work that influence exposure to risks15.What would mean, a priori, a greater financial gain and autonomy for those who work on the street or in a flat, compared to those working in clubs, is a loss of security. In turn, the entry into force in 2014 of the Citizen Security Law has caused a demand for services in more isolated places. Consequently, women change the better known and closer areas where they feel safer for areas in which they increase their vulnerability and the possibility of suffering attacks, and in turn they are forced to negotiate the "conditions" of the service quickly and clandestinely, which implies a loss of control in negotiating the use of a condom, and the price or type of service. Other authors also show an unequal exposure to HIV depending on the place where sex work is carried out16–18.
In order to generate key information to help design specific preventive interventions aimed at this population, the objectives of this study were to describe and compare the social characteristics, risk behaviours and prevalence of HIV, CT, and NG in FSWs according to the place where the sex work is carried out.
MethodsA cross-sectional study carried out during the second semester of 2018 as part of the bio-behavioural surveillance of the Sistema Integrado de Vigilancia Epidemiológica del VIH/ITS (SIVES) [Integrated HIV/STI Epidemiological Surveillance System], carried out with the collaboration of non-governmental organisations (NGOs) that develop comprehensive services at the social health level, as well as care, support and education programmes for sex workers, and in coordination with the entity Àmbit Prevenció Fundació [Prevention Area Foundation] for field work.
Study populationA (non-random) convenience sample of 400 FSWs >18 years old who worked on the street or on the roadside, in flats and in clubs, was selected, stratifying by country or area of origin (Spanish, Latin American, Eastern European and African) and considering a proportional allocation in each stratum.
Data collectionBehavioural information was collected through personal interviews during the months of March to July directly at the recruitment sites or at collaborating NGOs by interviewers from the social and/or health sectors who worked directly with this population. The participants received financial compensation at the end of the interview. The questionnaire was structured and adapted from the one used by Doctors of the World in 2002 and its adequacy and operation in real conditions was analysed in a pilot study19. The questionnaire included questions on sociodemographic characteristics, drug (cannabis, heroin, cocaine, ecstasy) and alcohol use, characteristics of the sex work, sexual practices with clients and with a stable partner, sexual and reproductive health, and access to social and health services. The reference period for the behaviours was ≤6 months after the interview was conducted. For the detection of antibodies against HIV in oral fluid samples, the Genscreen HIV 1 + 2 V2.0 enzyme-linked immunosorbent assay serological technique (Biorad, Spain) was used. The negative samples for this assay were tested by the Human IgG ELISA technique (Immunoperoxidase Assay for determination of Total IgG in human biological samples) to evaluate the suitability of the oral fluid samples, verifying the IgG concentration. All samples with IgG concentration >3.5 ng/mL were considered optimal. For the detection of CT and NG DNA in urine samples, the Anyplex CT/NG Real Time Detection molecular biology technique (Seegene, Seoul, Korea) was used.
All the samples were analysed in the Microbiology Service of the North Metropolitan Area laboratory of the Hospital Universitari Germans Trias i Pujol (HUGTiP).
Statistical analysisA descriptive analysis of the sociodemographic and behavioural variables was performed, in which frequencies and proportions were calculated for the categorical variables and the proportions were compared using Pearson's χ2 test or Fisher's exact test. For continuous data, the mean and standard deviation were calculated. Statistical significance was set at P < .05 and confidence intervals (CI) were calculated at 95%. The prevalence of HIV, CT and NG was calculated as the number of positive samples for any of these infections over the total number of samples tested. For data analysis, the statistical program IBM SPSS® version 20.0 (SPSS Science, Chicago, IL, USA) was used.
EthicsParticipation in the study was voluntary. After signing an informed consent form, participants answered the questionnaire and the biological sample was collected. Anonymity of the data was ensured by not including personal identifiers in the database. As they did not undergo a diagnostic test for HIV, but rather a valid test for epidemiological studies, participants were provided with information on where to take the HIV test if they wanted to do one, or confirmation in the event of a positive result. For STIs, they could receive the result by means of a numerical code and, if it was positive, receive medical attention and standard treatment. This study was approved by the HUGTiP research ethics committee, code EO-11-050.
ResultsSociodemographic, behavioural characteristics and use of social health services according to the place of sex workOf the 400 women recruited, the sample was distributed according to region or area of origin, with 45 Spanish, 160 Latin American, 101 Eastern European and 94 African.
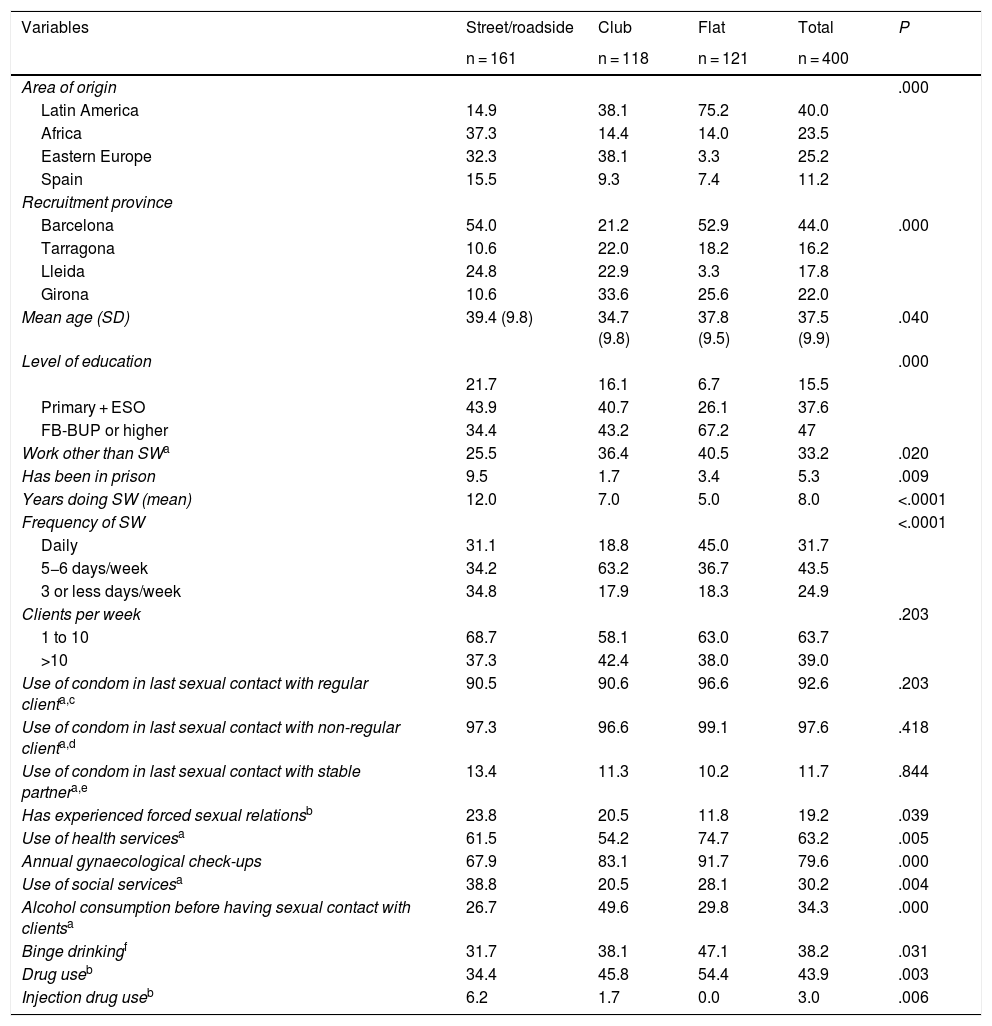
Table 1 shows the sociodemographic and behavioural characteristics and the use of social health services according to the place of sex work: street/roadside, club and flat. In total, 40.3% (161) of the interviewees engaged in sex work on the street/roadside, 29.5% (118) in clubs and 30.3% (121) in flats. According to the place of origin, Spanish and African women worked in a greater proportion in the street/roadside (15.5% and 37.3%, respectively), Latin American women in flats (75.2%) and those from Eastern Europe in clubs (38.1%). The mean age was 37.5 years (SD 9.9), with club workers being the youngest (34.7 years) and street/roadside workers being the oldest (39.4 years) and those with the lowest educational level (21.7% up to primary studies).
Sociodemographic, behavioural characteristics and access to social and health services according to the place of work.
| Variables | Street/roadside | Club | Flat | Total | P |
|---|---|---|---|---|---|
| n = 161 | n = 118 | n = 121 | n = 400 | ||
| Area of origin | .000 | ||||
| Latin America | 14.9 | 38.1 | 75.2 | 40.0 | |
| Africa | 37.3 | 14.4 | 14.0 | 23.5 | |
| Eastern Europe | 32.3 | 38.1 | 3.3 | 25.2 | |
| Spain | 15.5 | 9.3 | 7.4 | 11.2 | |
| Recruitment province | |||||
| Barcelona | 54.0 | 21.2 | 52.9 | 44.0 | .000 |
| Tarragona | 10.6 | 22.0 | 18.2 | 16.2 | |
| Lleida | 24.8 | 22.9 | 3.3 | 17.8 | |
| Girona | 10.6 | 33.6 | 25.6 | 22.0 | |
| Mean age (SD) | 39.4 (9.8) | 34.7 (9.8) | 37.8 (9.5) | 37.5 (9.9) | .040 |
| Level of education | .000 | ||||
| 21.7 | 16.1 | 6.7 | 15.5 | ||
| Primary + ESO | 43.9 | 40.7 | 26.1 | 37.6 | |
| FB-BUP or higher | 34.4 | 43.2 | 67.2 | 47 | |
| Work other than SWa | 25.5 | 36.4 | 40.5 | 33.2 | .020 |
| Has been in prison | 9.5 | 1.7 | 3.4 | 5.3 | .009 |
| Years doing SW (mean) | 12.0 | 7.0 | 5.0 | 8.0 | <.0001 |
| Frequency of SW | <.0001 | ||||
| Daily | 31.1 | 18.8 | 45.0 | 31.7 | |
| 5−6 days/week | 34.2 | 63.2 | 36.7 | 43.5 | |
| 3 or less days/week | 34.8 | 17.9 | 18.3 | 24.9 | |
| Clients per week | .203 | ||||
| 1 to 10 | 68.7 | 58.1 | 63.0 | 63.7 | |
| >10 | 37.3 | 42.4 | 38.0 | 39.0 | |
| Use of condom in last sexual contact with regular clienta,c | 90.5 | 90.6 | 96.6 | 92.6 | .203 |
| Use of condom in last sexual contact with non-regular clienta,d | 97.3 | 96.6 | 99.1 | 97.6 | .418 |
| Use of condom in last sexual contact with stable partnera,e | 13.4 | 11.3 | 10.2 | 11.7 | .844 |
| Has experienced forced sexual relationsb | 23.8 | 20.5 | 11.8 | 19.2 | .039 |
| Use of health servicesa | 61.5 | 54.2 | 74.7 | 63.2 | .005 |
| Annual gynaecological check-ups | 67.9 | 83.1 | 91.7 | 79.6 | .000 |
| Use of social servicesa | 38.8 | 20.5 | 28.1 | 30.2 | .004 |
| Alcohol consumption before having sexual contact with clientsa | 26.7 | 49.6 | 29.8 | 34.3 | .000 |
| Binge drinkingf | 31.7 | 38.1 | 47.1 | 38.2 | .031 |
| Drug useb | 34.4 | 45.8 | 54.4 | 43.9 | .003 |
| Injection drug useb | 6.2 | 1.7 | 0.0 | 3.0 | .006 |
STI: sexually transmitted infection; SW: sex work.
The average number of years engaged in sex work was 8.4 years, and was higher in street/roadside workers. Three-quarters of the women engaged in sex work daily or 5−6 days a week, with street/roadside workers having the lowest percentage (65%) compared to those in clubs or flats (82%) in both cases. Overall, 33% had worked in a job other than prostitution, with the street/roadside workers in a smaller proportion (25.5%). Similarly, a greater proportion of these had been in prison at some time in their lives (9.5%).
More than 90% stated they used condoms with both regular and non-regular clients, with no differences according to the place of work. The use decreased with a stable partner, being no higher than 15%, and was also similar according to the place of work. Around 20% of the women had been forced to have sexual relations at some time, a significantly higher percentage amongst street/roadside workers (23.8%) compared to those working in a flat (11.8%), who presented the lowest percentages.
Nearly half (43.9%) of the women had used some type of drug at some time in their lives. The consumption of both alcohol and other drugs was significantly lower in street/roadside workers, except for the consumption of injected drugs, which was significantly higher. Consumption before having sexual relations with clients was 34.3%, and significantly higher in club workers (49.6%). Binge drinking - intensive alcohol consumption - was reported by 38.2% of the women, being significantly higher in those who worked in flats (47.1%).
The use of health services in the last six months was 63.2% and significantly higher amongst those working in a flat (74.7%), a higher proportion of whom (48.8%) used private health services. Meanwhile, street/roadside workers used social services in a greater proportion (38.8%) compared to the total that used them in the last six months (30.2%).
The majority of women (79.6%) had annual gynaecological check-ups, though to a lesser extent amongst street/roadside workers (67.9%).
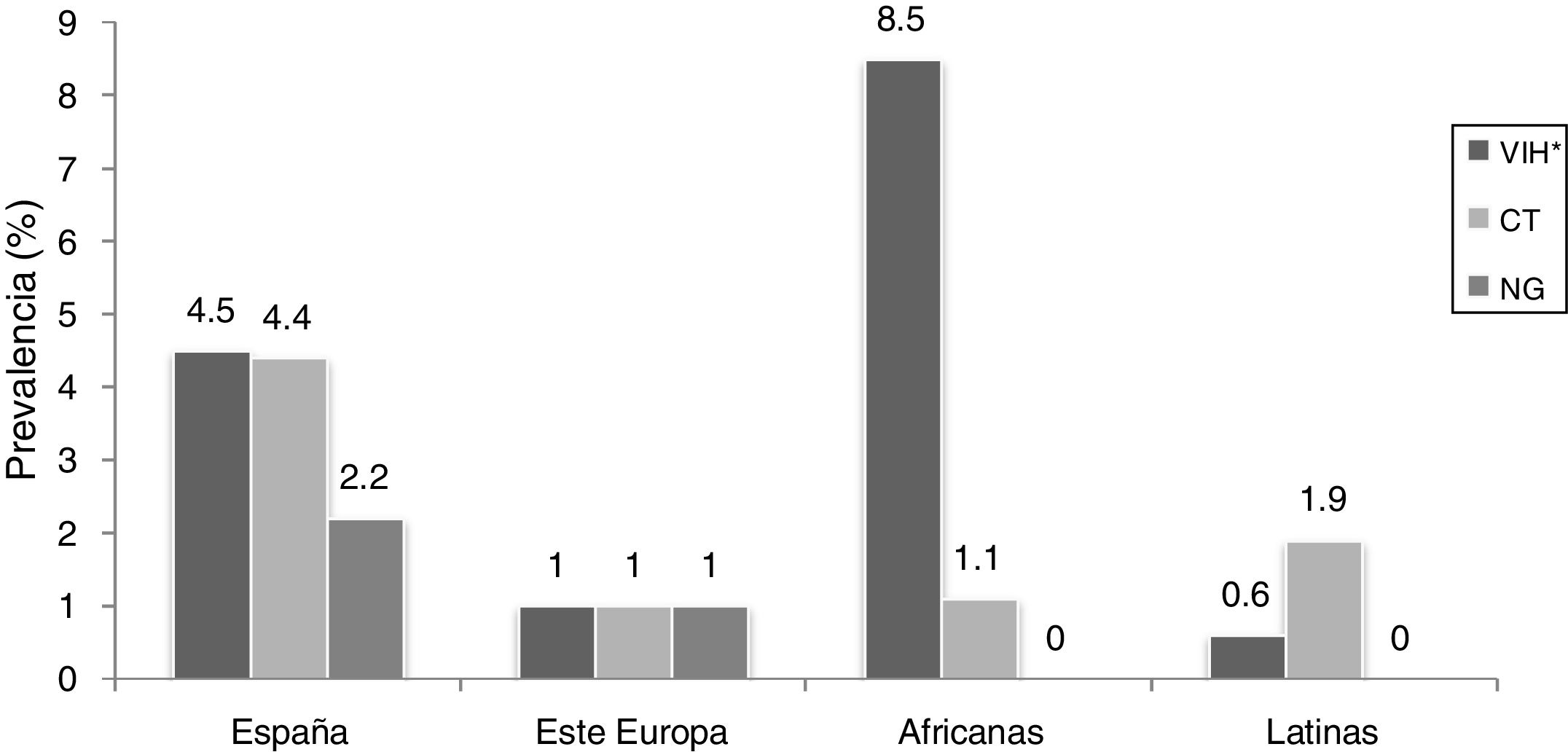
HIV/STI prevalenceThe overall prevalence of HIV was 3.0% (95% CI: 1.5–5.0), and the prevalence of CT and NG was 1.8% (95% CI: 0.5%–3.3%) and 0.5% (95% CI, 0.0–1.5), respectively. By country of origin, HIV prevalence was significantly higher (P = .002) amongst African women (8.5%), followed by Spanish (4.5%), Latin American (1.9%) and Eastern European (1%). The prevalence of CT and NG was higher in Spanish FSWs (4.4% and 2.2%, respectively) (Fig. 1).
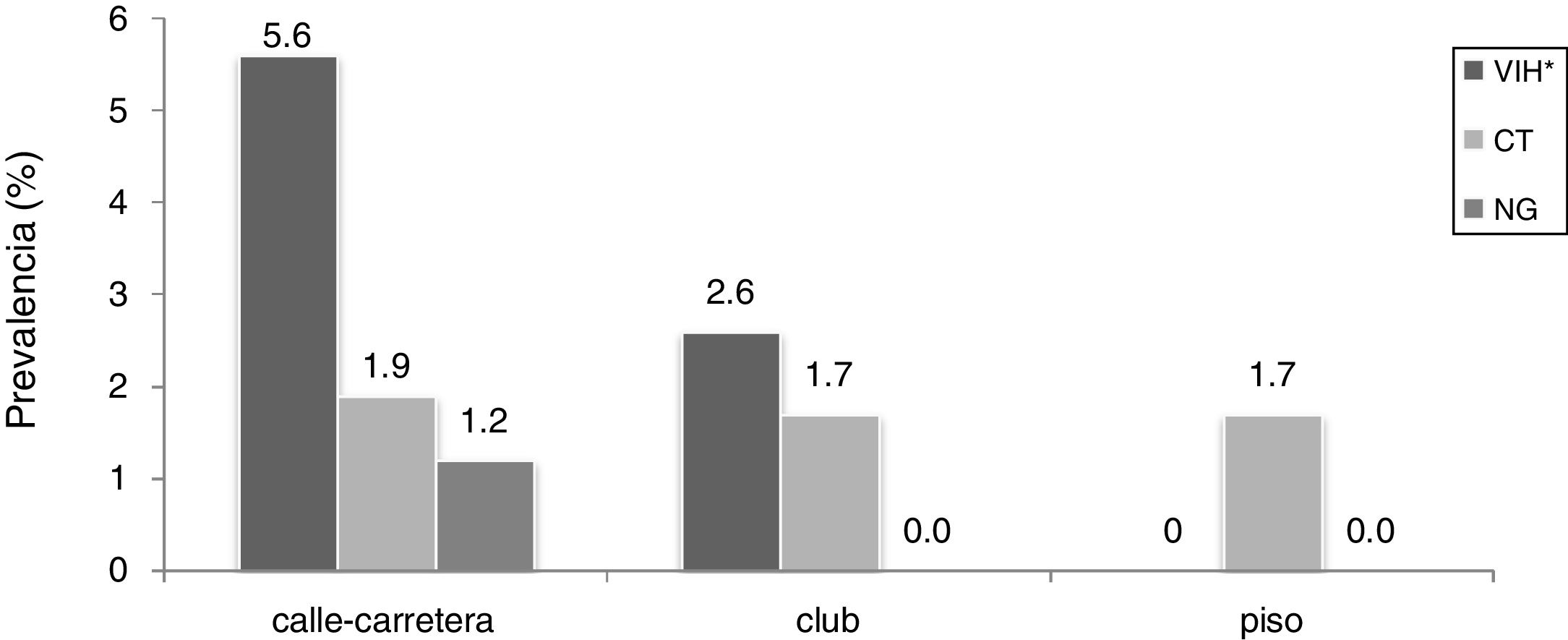
On the other hand, women who worked on the street/roadside presented higher prevalences for CT and NG (1.9% and 1.2%, respectively) and significantly higher prevalence (P = .023) for HIV (5.6%) compared to the lowest values (1.7%) for those working in a flat (Fig. 2).
DiscussionThis study shows that FSWs present different vulnerabilities depending on the place where they carry out their work, and women who work on the street/roadside are the ones with the most precarious conditions and the greatest vulnerability related to socioeconomic factors: they are older, with a lower level of studies and lower financial remuneration for their services. Other factors associated with lifestyle or behaviour are also observed: injection drug use, more time in sex work or vulnerabilities associated with a series of structural or social determinants, less access to health services, sexual violence with forced sexual relations and stay in prison. Other factors associated with increasing vulnerability observed in the literature have been psychological and/or social problems of stigmatisation and social uprooting13.
Street/roadside prostitution is the one that has experienced the greatest change in our country. If it was traditionally linked above all to the consumption of injected drugs, exercised by Spanish women and located in central urban areas, today it is exercised in a greater proportion by women from sub-Saharan Africa and has been moving away from urban centres after the entry into force of new citizen security laws, which has increased their vulnerability.
On the one hand, and related to this increase in vulnerability, we find HIV. It is estimated that, globally, 15% of infections are attributable to female sex work, though this figure is lower than 2% in Europe20. The prevalence of HIV in our study (3%) has remained low since 20055. These low prevalences are consistent with the widespread use of condoms in the work setting, and also coincide with European data21,22. Of special note is the significantly higher prevalence amongst female street/roadside workers, already described by other authors16–18, which highlights the greater risk of infection amongst this group compared to those who work in closed premises23,24, mainly attributable to differences in origin, age, legal status, working conditions, type of sexual practices or access to health services3.
Regarding origin, the street/roadside FSWs were mainly Spanish and African. The former have traditionally presented a higher prevalence of HIV associated mainly with the consumption of injected drugs1,24,25, a risk factor associated with HIV26, and in our study, the street/roadside workers presented a higher consumption of these. On the other hand, African FSWs, of sub-Saharan origin, have higher endemic prevalences of HIV, with 55% of infections in young women and by heterosexual transmission2.
On the other hand, street/roadside workers also presented prevalences for CT and NG higher than the rest of the groups, although they continue to be lower than other populations in our country27 and those reported in European studies, situated at around 7% and 5% for CT and NG, respectively16. As is the case in other European countries23 and in previous studies carried out in our country, a decrease in the global prevalence of CT is observed (from 5.9% in 2005 to 1.8% in 2018), whilst NG remains stable8.This decrease is due, on the one hand, to the widespread use of condoms with clients, and on the other, to the fact that the majority of FSWs go annually to sexual and reproductive health services, which in Catalonia perform CT screening on all women under 25 years of age and older women with risk criteria, with FSWs forming part of this group.
Likewise, street/roadside workers show a series of structural factors, such as violence associated with higher percentages of forced sexual relations or abuse, which also increase their vulnerability. The data indicates that around 30% of the FSWs have suffered harassment or violence in clubs, compared to 70% of those who have suffered it on the street28. Physical and sexual violence in the place of work, whether by clients, managers or other people in their environment, is often related to drug use29, becoming in turn a determining factor in the acquisition of HIV, given the risk of transmission related to lack of protection in sexual practices, in part due to clients refusing to use a condom or it breaking when they do25. In fact, one study addresses that the elimination of client sexual violence, by itself, could prevent 20% of HIV infections30. Thus, violent events, drug use and lack of protection in sexual practices seem to be related. Women sex workers who inject drugs and work on the street have suffered more episodes of aggression than those who work in other sectors, whose drug use is occasional or instrumental25.
Therefore, the policies and the social and physical characteristics of sex work can mitigate or confer a higher risk of HIV/STIs amongst FSWs. Thus, environments with management policies, such as clubs, usually have security mechanisms and promote the use of condoms compared to other places such as the street/roadside where incentives are offered by the client for unprotected sex, and refusal of payment, fines from the authorities, assaults, drug use and limited access to resources are factors that are associated with greater vulnerability to HIV/STIs. When FSWs have adequate access to sexual health services with the provision of preventive material, HIV/STI detection tests and treatment, increased condom use and lower prevalence of these infections are observed.
Amongst the limitations of the study, it should be noted that the sample was not representative of the FSW population in Catalonia, which makes it difficult to generalise and extrapolate the results to the total FSW population. However, through prior mapping, information was collected to diversify the sample, including women from different countries in different contexts where sex work is carried out in Catalonia. The second limitation is related to the validity of the data, since the prevalence of some behaviours may be underestimated. In this sense, an attempt was made to establish anonymity so as to encourage FSWs to do interviews, using understandable language, in addition to the fact that the interviewers, professionals who work directly with this population, facilitated participation.
Despite its limitations, this study makes it possible to monitor the prevalence of HIV/STIs and the associated determinants in a vulnerable group, due in part to social and structural factors. It therefore provides key information to adapt the specific health promotion and prevention interventions carried out in our context. These comprehensive health interventions must be approached holistically and taking into account unmet needs, considering social, health and inequality determinants, including access to services and the experience of violence and migration, without forgetting FSWs' non-commercial sexual partner as a key element. In addition, it is necessary to raise awareness amongst FSWs about the risks of these infections, and the need to carry out periodic tests. Therefore, prevention measures with the aim of improving, above all, the conditions of women who work in conditions of special difficulty and/or vulnerability, especially immigrants, and in those who work on the street/roadside, are a priority.
FundingPublic Health Agency of Catalonia, Generalitat de Catalunya; Agència de Gestió d’Ajuts Universitaris i de Recerca - AGAUR [Agency for the Management of University and Research Grants] (2005/SGR/00505), Department of Universities, Research and Information Society of the Generalitat de Catalunya.
Conflicts of interestThe authors declare that they have no conflicts of interest.
To the participating women, interviewers and collaborating NGOs: ACAS Girona, Actua Vallès Sabadell, Àmbit Prevenció - ÀMBITdona and ÀMBITmaresme programmes, Assexora’t Tarragona, Associació Anti-sida [Anti-AIDS Association] Lleida, Maresme-Selva Health Corporation, El Lloc de la Dona [The Women's Place], Programa Carretera [Road Programme] (Hospital St. Jaume de Calella).
Please cite this article as: Lopez-Corbeto E, Sanclemente C, González V, Mansilla R, Casabona J, Folch C. Vulnerabilidad frente al VIH, clamidia y gonococia según el lugar donde se ejerce el trabajo sexual. Enferm Infecc Microbiol Clin. 2022;40:166–171.