Continuous intraduodenal levodopa/carbidopa infusion (Duodopa®) is indicated in patients with advanced Parkinson's disease refractory to conventional treatment. This type of novel pump may give rise to adverse effects that tend to be similar in nature to a gastrostomy tube used for other indications such as infection, granuloma, haemorrhage, pneumoperitoneum or buried bumper syndrome.1,2 We present the case of a 74-year-old male patient with advanced Parkinson's disease who has been undergoing Duodopa® pump treatment for the last two years. He attended A&E owing to a lodged tube and abdominal pain.
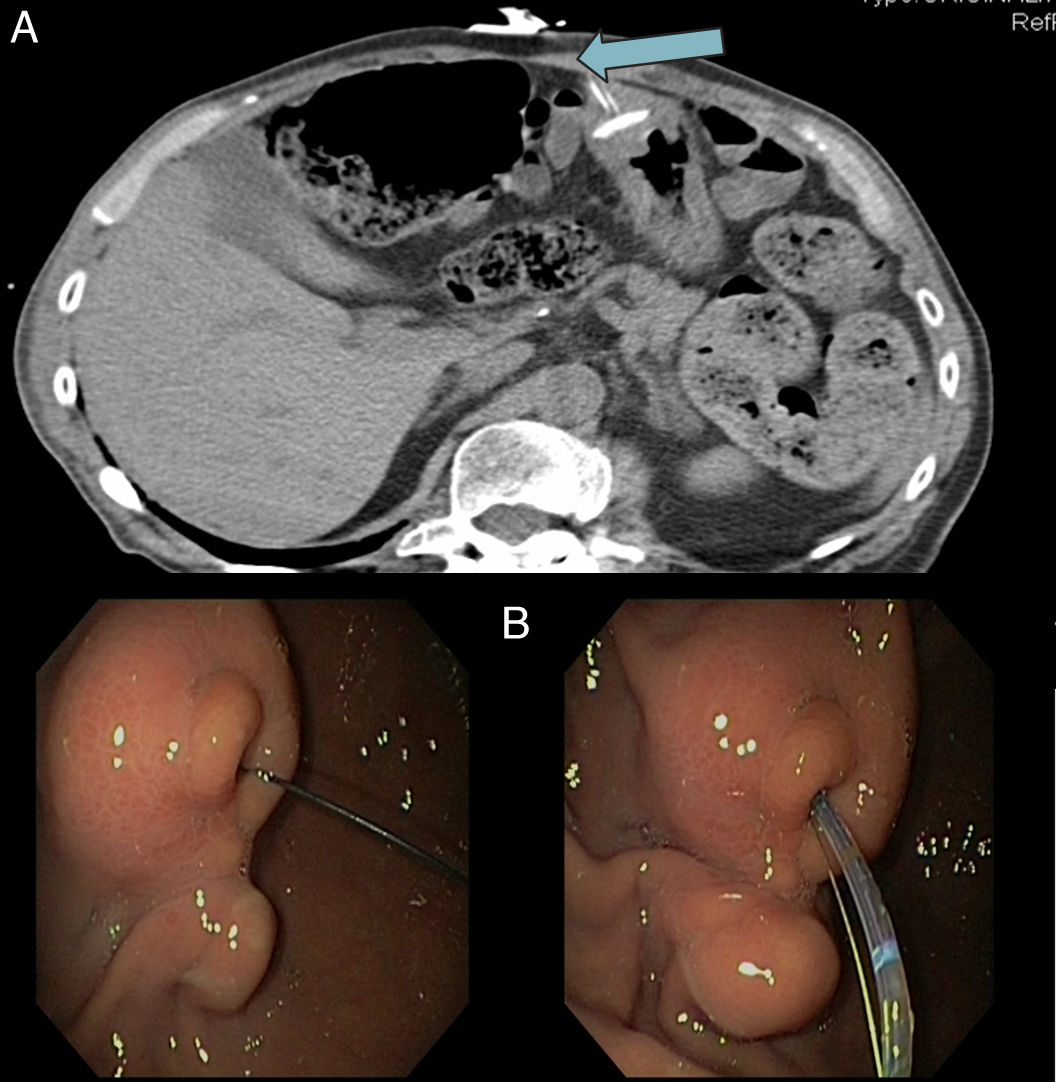
An abdominal CT scan was performed which revealed a buried bumper (Fig. 1, arrow). An oral panendoscopy under propofol anaesthesia was then performed using the Olympus EVIS EXERA II® GIF-H180 conventional gastroscope (2.8mm lumen). A mamelon in the antrum was found with the internal bumper completely buried and the tube protruding through it. The internal tubing was removed through the gastrostomy tube. A 0.0035 guidewire was introduced through the external pump to check its access to the gastric cavity and a conventional sphincterotome was placed following the guidewire (Fig. 1).
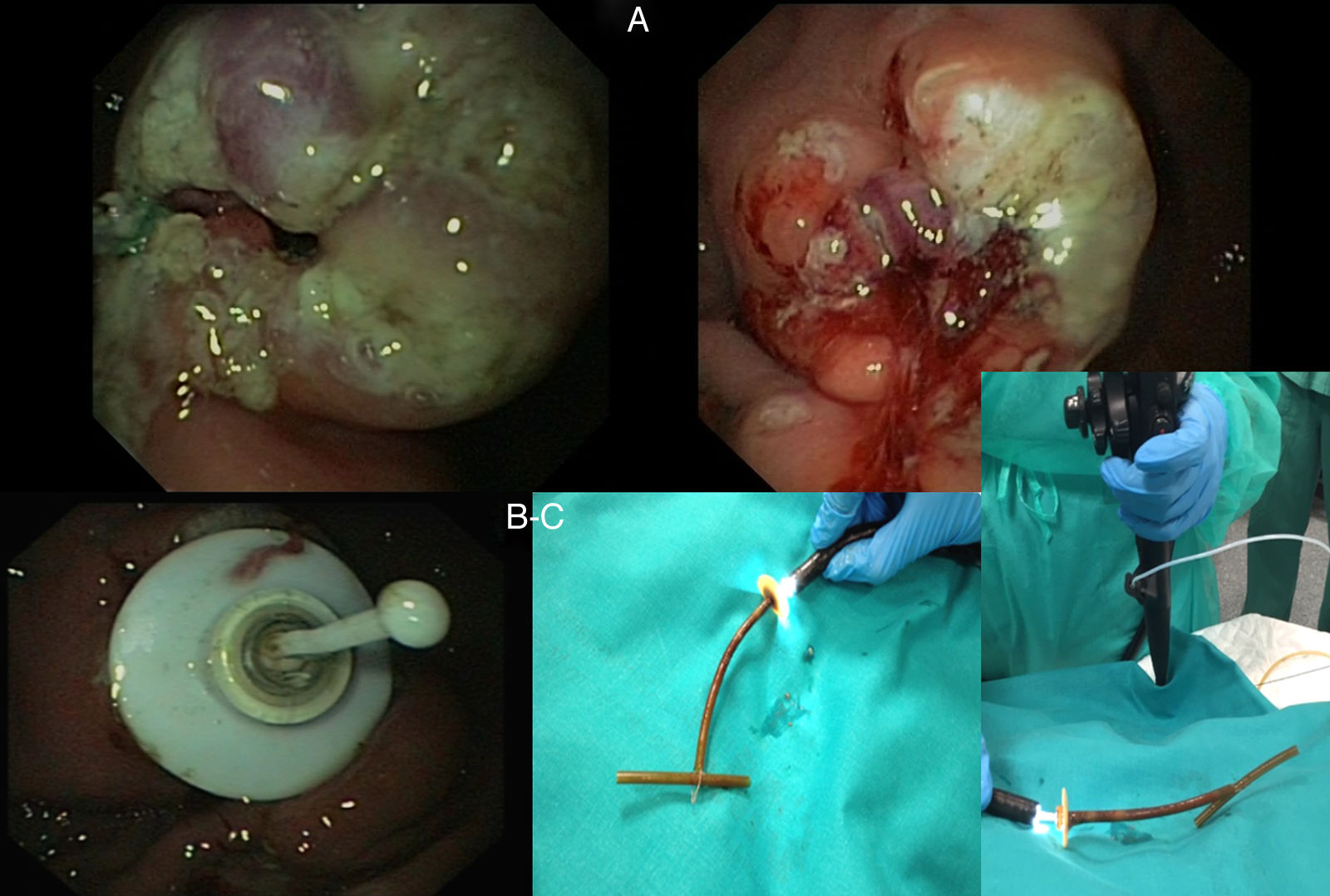
First, a number of tangential incisions were made to the exit port with a conventional sphincterotome, and then with a precut needle knife or MicroKnife to expose the bumper and dislodge it. Using the push-pull T technique, the tube was cut about 3cm from the abdominal wall and then a conventional polypectomy snare was fed through the gastroscope channel before passing through the gastrostomy tube (following the guidewire) and ultimately exiting the abdominal wall. The snare was then tied to the cut end of the tube and perpendicular to the tube to form a “T”, before being pulled back into the gastric cavity, where it dragged the bumper with it to be removed through the mouth. Finally, a new Freka® PEG Gastric FR 15 tube was inserted (Fig. 2). A Freka® FR 9 enteral tube was then inserted. The distal end of the tube was fed to the duodenum and its correct operation was confirmed. Currently, six months later, the patient is completely asymptomatic.
(A) Multiple tangential incisions to the exit port exposing the bumper and enabling it to be dislodged. (B) A polypectomy snare was then fed in and pulled out. A stopper was tied to its end in the form of a “T”, before being pulled back into the gastric cavity, where it dragged the bumper with it to be removed through the mouth. (C) Finally, a guidewire was fed through the gastrostomy opening and removed through the mouth and a Freka® FR 15 tube was inserted.
Whilst the combination of techniques conducted (Needle Knife technique and push-pull T technique) have been previously reported in conventional gastrostomy feeding tubes, this case is of particular interest because they have never been reported in Duodopa® pumps. In this case, an Olympus 120W Needle Knife at a diathermy power of 80W was used. The Needle Knife facilitates exposure of the internal bumper, reducing the resistance exerted by the gastric wall on the tube thereby making it easier to dislodge.3,4
Although still new, use of Duodopa® pumps in patients with advanced Parkinson's is steadily increasing thanks to its excellent results.1,2 This means that gastroenterologists will come across this type of tubing and its adverse effects, including perforation and haemorrhage, more and more often in routine clinical practice. Other types of percutaneous gastrostomy tube feature a flexible fixation plate to facilitate their extraction. As our case featured a rigid plate, it had to be dislodged and orally extracted. The prevalence of buried bumper syndrome is around 1%.5 Numerous techniques to treat this complication have been reported,3,4,6–8 and the technique described above should be considered a complementary procedure in its treatment. As it represents a simple and low-risk alternative, it could play a future role in the treatment of a greater number of patients with gastrostomy tubes.3
FundingThe authors declare that they did not receive funding to complete this study.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Magaz Martínez M, Martínez Porras JL, López Gómez M, Santiago J, Bernardo C, Abreu L. Alternativa endoscópica al síndrome de buried bumper secundario a bomba de Duodopa®. Gastroenterol Hepatol. 2017;40:360–362.