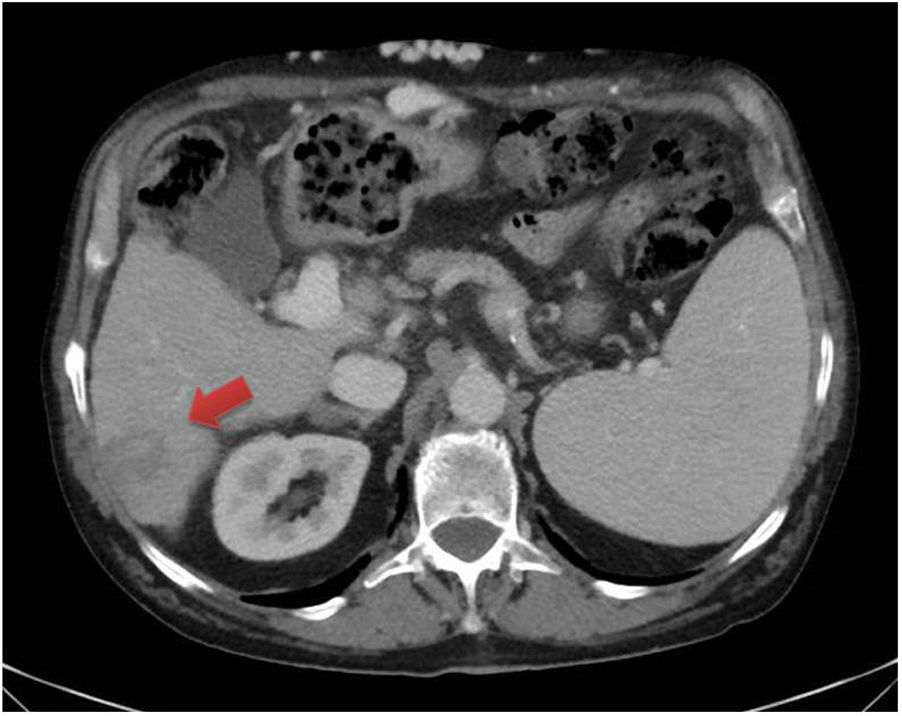
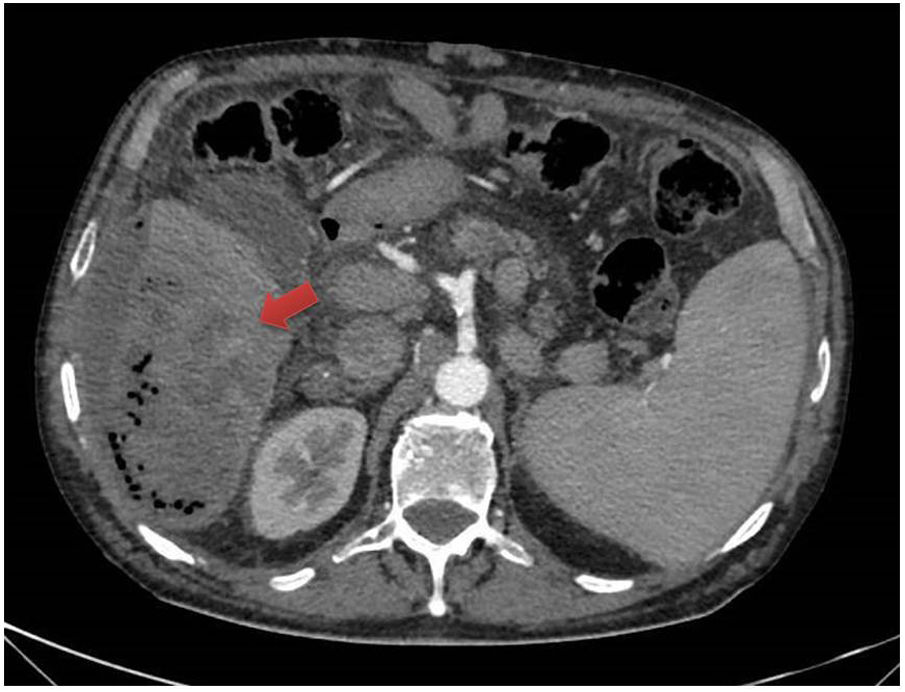
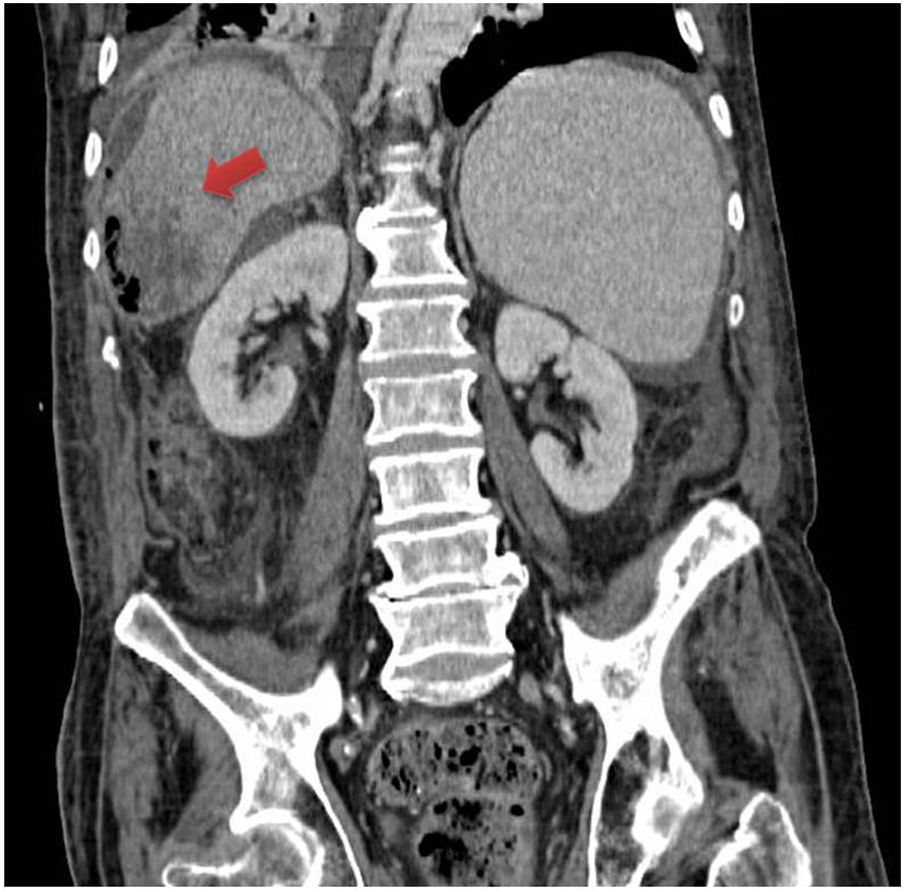
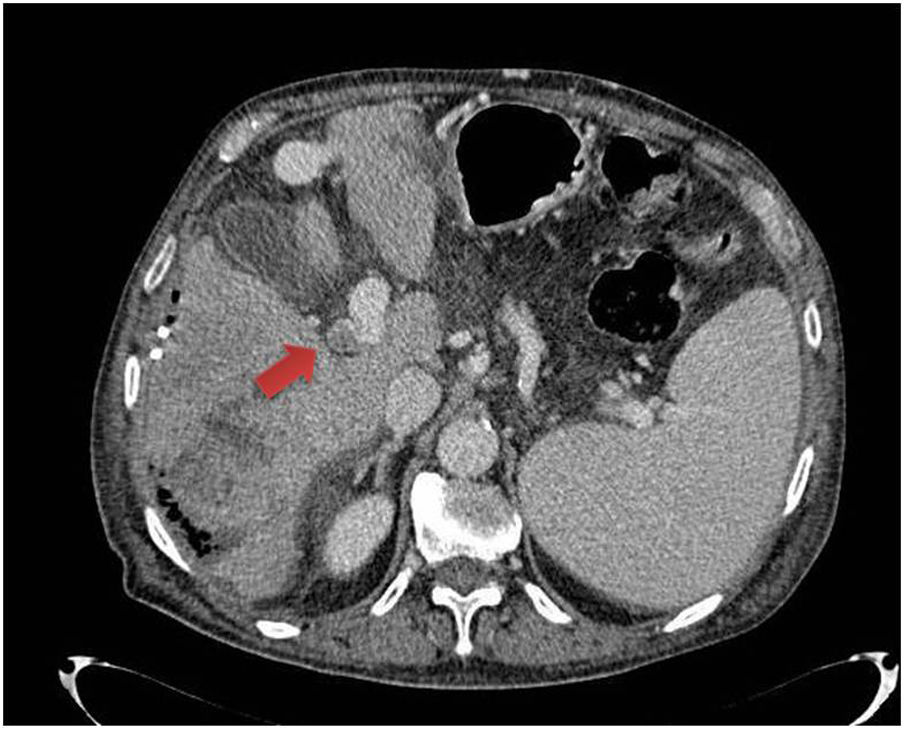
A 74-year-old male with hepatocellular carcinoma in segment 6 (Fig. 1) with underlying alcoholic cirrhosis, Child-Pugh B8, treated with transarterial chemoembolisation (TACE). Five days later, he developed pain in the right hypochondriac region, without fever. Abdominal computed tomography scan showed an abscessed lesion 60 × 100 × 60 mm in size in segment 6, extending to the perihepatic space, with a collection 160 × 22 × 135 mm in size and pylephlebitis (Figs. 2 and 3). This was treated with intravenous meropenem and ultrasound-guided percutaneous drainage with catheter placement. Subsequent scans showed the collection decreasing in size (Fig. 4).
TACE is the treatment of choice in Barcelona Clinic Liver Cancer stage B (BCLC-B) hepatocellular carcinoma, and is also effective in unresectable liver metastases.1–3 It is minimally invasive, but it can have serious complications such as liver abscesses.1,4 These are rare, with an incidence of 0.2–5%, but have high morbidity and mortality rates.1,2,4 Risk factors are biliary disorders (sphincterotomy or biliary anastomosis), advanced age, diabetes, a large tumour and portal thrombosis.1,4 Sphincter of Oddi dysfunction has been suggested as a pathogenic mechanism, as it would allow bacteria to access the hepatic circulation, infecting necrotic tissue.2 The clinical context is important for differentiating between an abscess and the presence of gas in the embolised lesion due to necrosis a few days after embolisation. Moreover, unlike post-embolisation syndrome, which usually occurs early, abscesses may appear more than a week later.1
Please cite this article as: Díaz Alcázar MdM, et al. Complicación infrecuente tras quimioembolización de hepatocarcinoma sobre hígado cirrótico: absceso hepático y pileflebitis. Gastroenterol Hepatol. 2021;44:382–383.