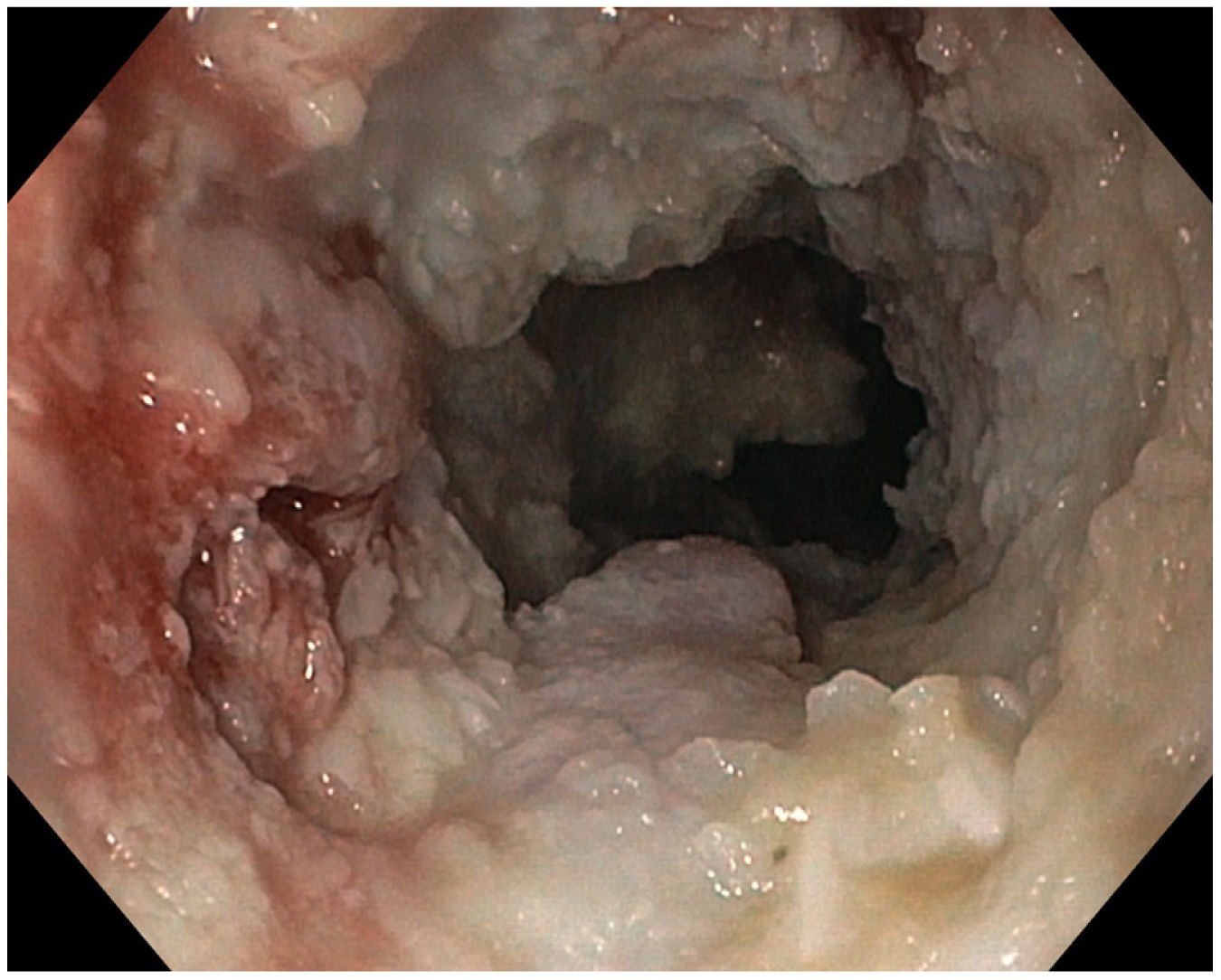
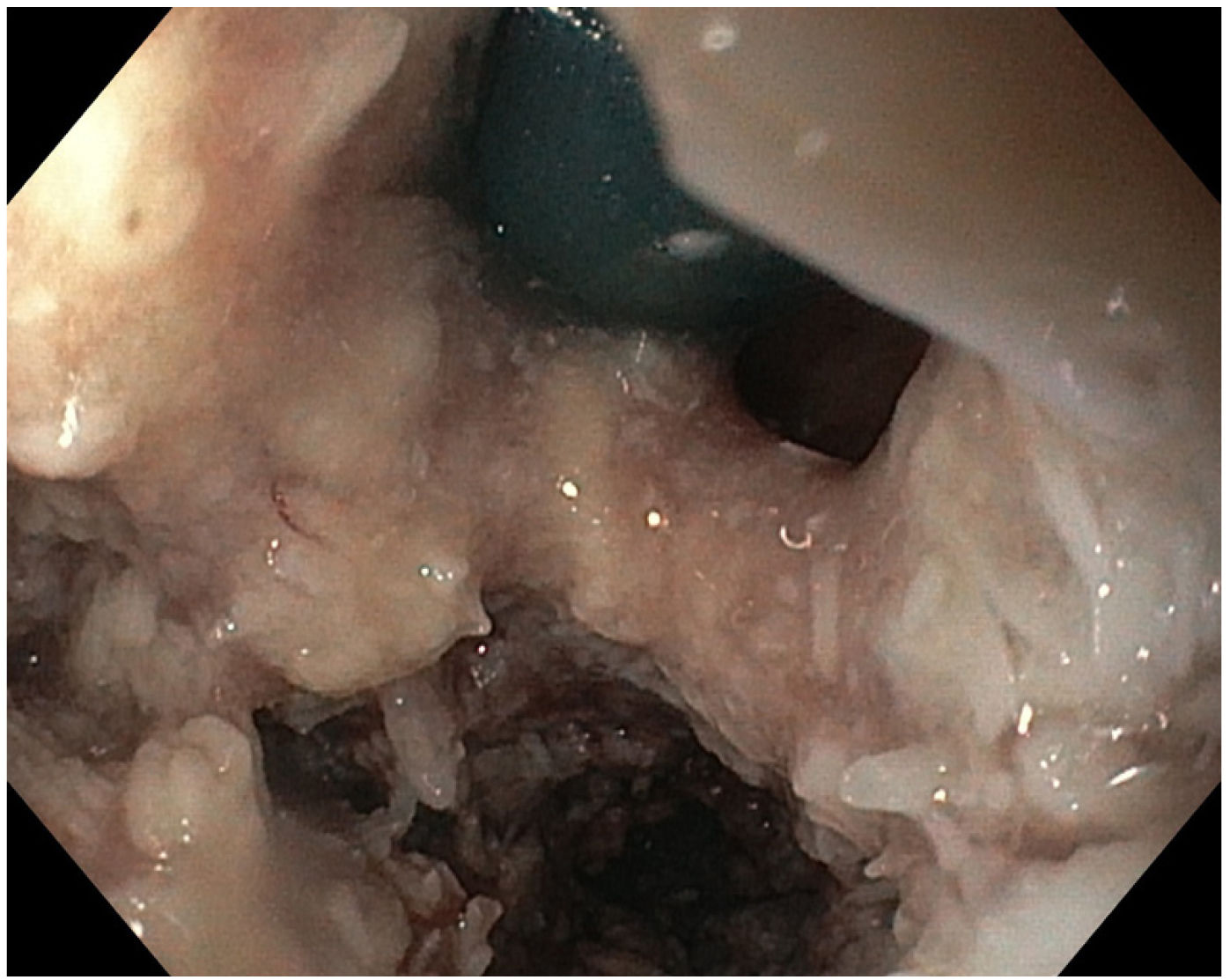
A 53-year-old woman, a smoker with no other medical history, who reported dysphagia and weight loss. The oesophago-gastro-duodenoscopy revealed a polypoid oesophageal mucosa covered by whitish plaques and a fistula towards the bronchial tree (Fig. 1). The histological study of the biopsies revealed hyphae and spores and ruled out malignancy. The biopsy culture showed growth of Candida glabrata. In addition, a PCR test for herpes simplex virus was positive. Computed tomography and a videofluoroscopy swallow study were performed, confirming an 8-mm fistula connecting the oesophagus and the left bronchus (Fig. 2). The patient's only risk factor for candidiasis was malnutrition.
Initially, she received treatment with intravenous fluconazole and parenteral nutrition. Given the lack of improvement, a bronchial prosthesis (Fig. 3) and a gastrostomy tube were inserted. An oesophageal prosthesis was not placed due to the very proximal location of the fistula. Two months later, the patient was admitted for pneumonia and the decision to perform surgical treatment of the fistula was finally taken.
Candidal oesophagitis usually involves the mucosa. There are few reported cases of transmural candidiasis and they are usually associated with severe immunosuppression.1,2 Necrosis is the cause of most complications and is related to viral superinfection.1 Treatment is fundamentally based on the placement of an oesophageal and/or bronchial prosthesis.