Brunner's glands are found in the submucosa of the duodenal bulb and in the second portion of the duodenum. Their primary function is to secrete a mucin-rich alkaline fluid that protects the duodenal epithelium from the contents of the stomach. Brunner's gland adenoma is an extremely rare tumour, with an incidence of less than 0.4% in endoscopic studies.1 It is usually identified by chance following a gastroscopy performed for other reasons and in extremely rare circumstances it can present as an acute complication.2
We present the case of a Brunner's gland adenoma that manifested as upper gastrointestinal bleeding.
The case concerns a 57-year-old woman with a prior history of hypertension and a former smoker who attended A&E due to a 48-h history of passing melaenic stool. The patient had no changes in her bowel habit nor a history of non-steroidal anti-inflammatory drug intake. She reported mild gastrointestinal symptoms such as pyrosis and occasional postprandial dyspepsia, with no warning signs.
Upon arrival at A&E, the patient was in good general condition and haemodynamically stable. The digital rectal examination was positive for melaena. The blood panel was completely normal (haemoglobin: 14.1g/dl; haematocrit: 43.1%; platelets: 192×109/l; prothrombin time: 12.5s; urea: 18mg/dl).
The gastroscopy revealed a polypoid formation measuring approx. 8mm in diameter on the anterior aspect of the apex of the duodenal bulb, with an erosion on the apex and haematin on the surface indicative of recent bleeding. Given the lack of active bleeding at that time, therapeutic endoscopy was not performed and the site was not biopsied. The patient was discharged with antisecretory therapy (omeprazole 40mg/day) and an endoscopy was scheduled to assess the lesion.
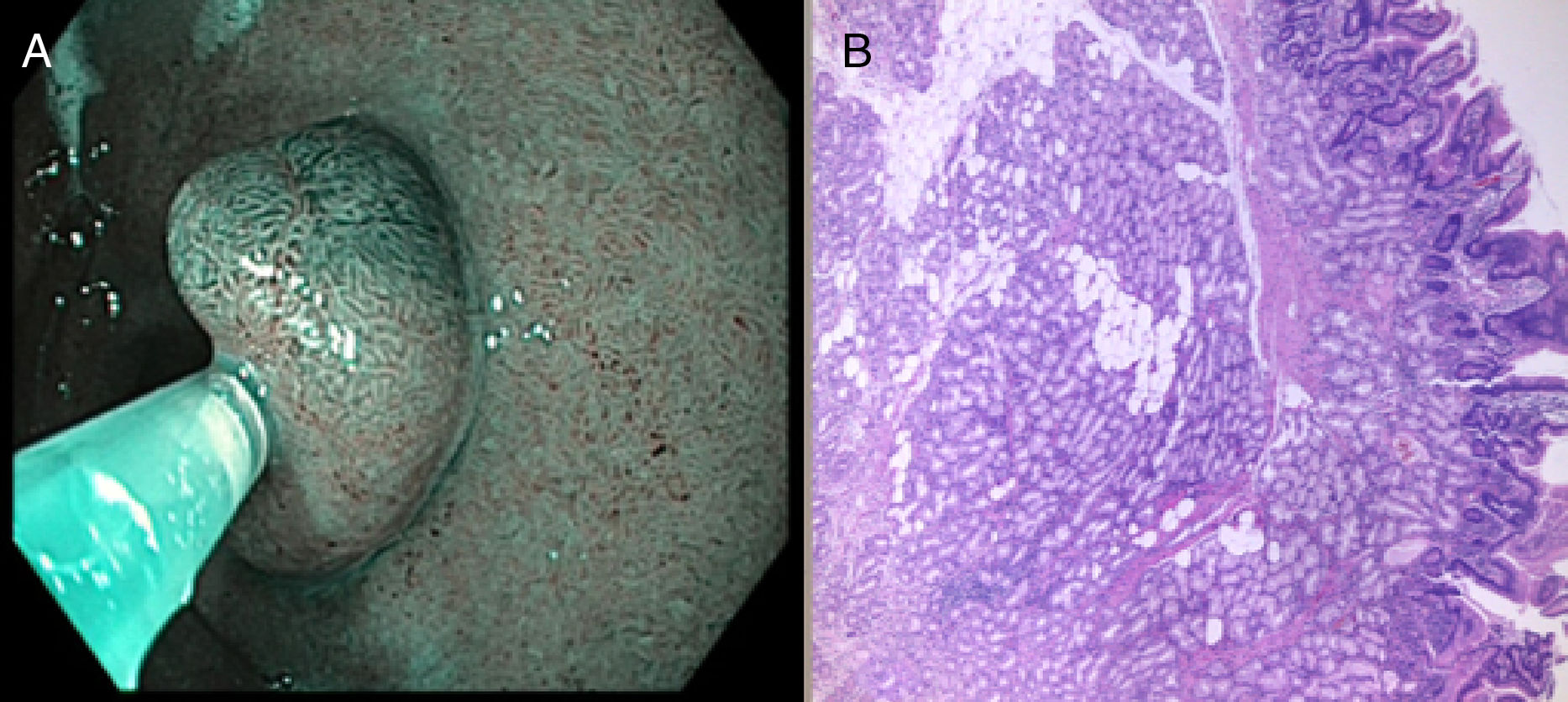
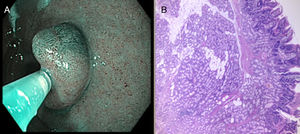
At the second endoscopy, the lesion was characterised with narrow-band imaging: a homogeneous and preserved surface pattern was observed with a villus size similar to that of the surrounding mucosa and a preserved and regular vascular pattern (Fig. 1A), suggestive of a benign, probably subepithelial lesion. A mucosectomy was performed to excise the lesion en bloc, with no immediate complications. The pathology findings confirmed Brunner's gland adenoma with no associated dysplasia (Fig. 1B).
The gastroscopy performed four months after the excision revealed normal mucosa and, to date, the patient has experienced no further episodes of gastrointestinal bleeding.
Brunner's gland adenoma is a rare tumour found in the duodenal bulb and in the second portion of the duodenum. Although it tends to be asymptomatic, on rare occasions it can give rise to gastrointestinal bleeding, bowel obstruction, chronic anaemia and, anecdotally, recurrent pancreatitis. Fewer than 20 cases involving gastrointestinal bleeding have been published, the majority manifesting as melaena.3 In most cases, the tumours measured in excess of 20mm, approximately twice the size of the adenoma of our patient. However, the absence of other causes that could explain the bleeding, the finding of ulceration on the surface and the lack of recurrent bleeding once the adenoma had been excised confirmed the cause of the bleeding to be a tumour.
With regard to treatment, resection is not recommended in asymptomatic patients with lesions measuring less than 2cm.4 For symptomatic tumours, surgical resection was the treatment of choice in most of the published cases, due to the size of the lesion. However, endoscopic resection was performed in those cases, such as ours, where the tumour measured ≤2cm. It may be feasible to confirm the diagnosis of subepithelial lesion by endoscopic ultrasound prior to resection. However, its diagnostic performance in duodenal lesions measuring less than 1cm is not well documented and it may be complicated to obtain suitable samples for diagnosis by puncture.5 Taking all of the above into consideration, together with its non-malignant appearance in the optical diagnosis and its manifestation as gastrointestinal bleeding, we opted for mucosal resection without prior endoscopic ultrasound.
Upper gastrointestinal bleeding secondary to Brunner's gland adenoma is a rare complication. Larger lesions have been associated with more significant bleeding with a greater impact on clinical status and blood test results. Resection of the lesion is indicated when any adenoma-associated complications manifest. Endoscopy is the approach of choice for lesions measuring less than 2cm, while surgery is reserved for larger lesions.
Please cite this article as: Herreras J, Giner F, Cordon G, Roca MJ, Bustamante-Balén M. Hemorragia digestiva alta como complicación de un adenoma de glándulas de Brunner. Una presentación inusual. Gastroenterol Hepatol. 2019;42:395–397.