We present the case of a 67-year-old female patient with no relevant medical history or history of smoking or alcohol or substance abuse. She was admitted to Gastroenterology with a six-day history of epigastric pain, for which she had already visited the Accident and Emergency Department five days earlier, but had been discharged home as investigations were normal (lab tests, abdominal ultrasound) and good pain control was achieved with analgesia. On this occasion, analyses showed slight elevation of liver enzymes (AST 64 U/l, ALT 104 U/l, GGT 143 U/l, alkaline phosphatase 187 U/l) and elevation of acute phase reactants (C-reactive protein >350mg/l, fibrinogen 1000mg/dl), but abdominal ultrasound was normal once again. During her stay in hospital, good pain control was achieved, the patient's general condition remained good and to complete the tests, an abdominal computed tomography (CT) scan was requested, which she had on day four. The CT scan showed an intra-abdominal collection with a high air-fluid level (12×14cm) in contact with the left lobe of the liver and gastric antrum (Fig. 1A–B).
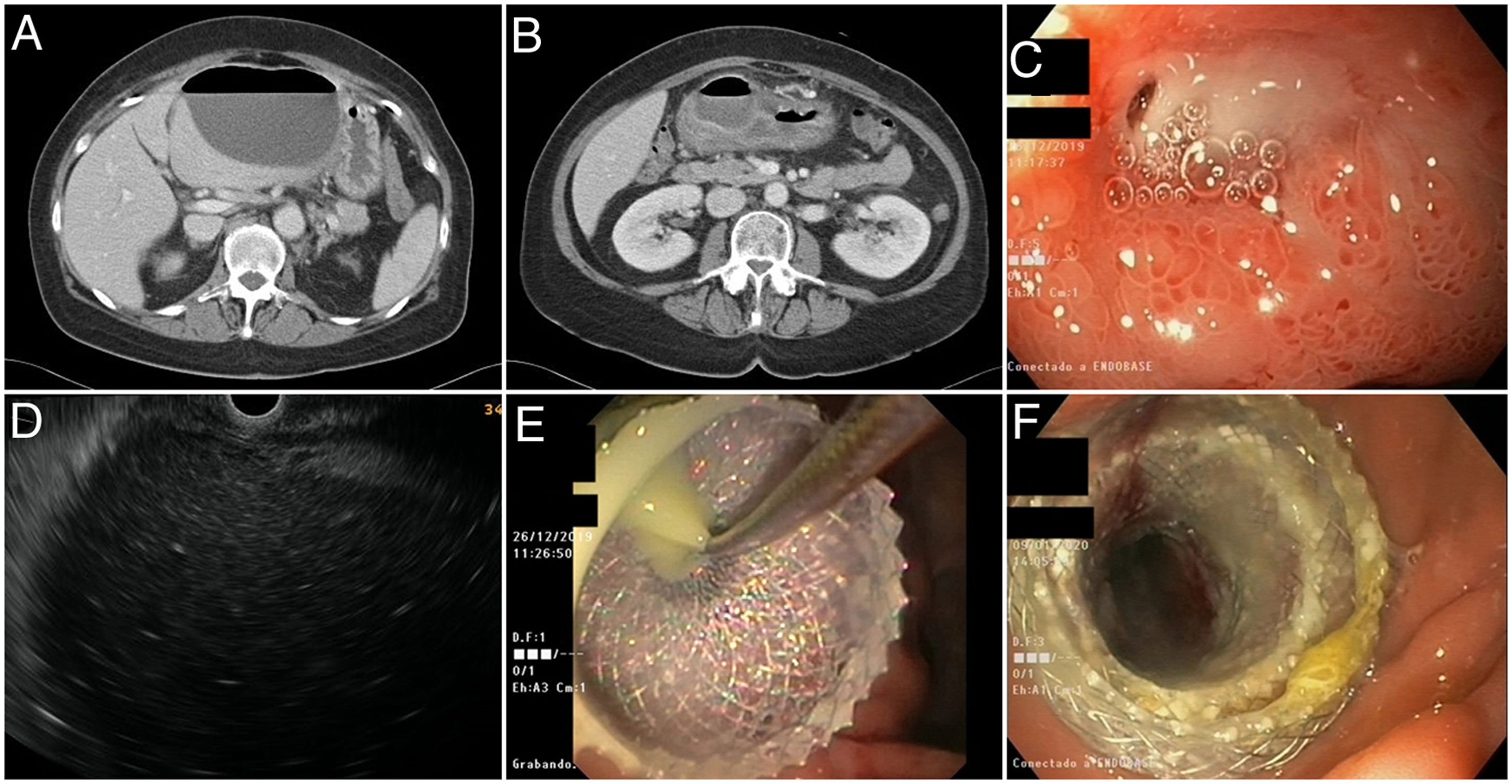
A-B) Abdominal CT images showing a large hypodense collection with an air-fluid level compatible with abscess, showing contact with the left lobe of the liver and with the gastric antrum. C) First gastroscopy. Duodenal bulb ulcer with a hole in its interior suggestive of perforation. D) Endoscopic ultrasound image of the abdominal collection from the gastric antrum. E) Moment of placement of the Hot-Axios® lumen-apposing stent with drainage of purulent material. F) Check-up after one week; open stent allowing access to a cavity now free of purulent material.
A gastroscopy was performed to make a differential diagnosis between abscess of biliary or gastroduodenal origin. In addition to an image of extrinsic compression of the gastric antrum, the duodenal bulb was found to have oedema and inflammation and, on its anterior surface, a small 5-mm ulcer covered with fibrin with spontaneous drainage of purulent content through a 2-mm hole in the interior, suggestive of perforation (Fig. 1C). As the patient was virtually asymptomatic and there were no signs of alarm, we opted for non-surgical management and endoscopic ultrasound was performed, again visualising the collection (Fig. 1D) and placing a Hot-Axios® 10×20mm lumen-apposing stent at the level of the antrum which enabled drainage of abundant purulent material (Fig. 1E). Due to its large size, easy access, and low output from the orifice of the fistula, we decided to drain the collection, as we considered that conservative management would not resolve the problem and would substantially prolong hospital admission. A repeat gastroscopy was performed a week later, showing a collection containing no purulent material (Fig. 1F), covered with granulation tissue. Two weeks later, the stent was removed after complete resolution of the condition. As regards the aetiology of the ulcer, biopsies taken to rule out H. pylori came back negative, and it was assumed that the ulcer was related to the patient taking non-steroidal anti-inflammatory drugs (NSAID) prescribed for joint pain weeks prior to admission. The patient had been started on treatment with proton pump inhibitors (PPI) at diagnosis, with subsequent follow-up endoscopies showing the ulcer to have completely healed.
Endoscopic ultrasound-guided drainage, less invasive than percutaneous or surgical, is a procedure increasingly used in a range of indications. Lumen-apposing stents are shorter than conventional metal stents and have wider ends, which reduces the risk of migration. They are currently one of the most widely used stents for endoscopic ultrasound-guided drainage of infected encapsulated pancreatic necrosis, with data suggesting that they may be superior to drainage with plastic stents, although as yet there is a lack of solid evidence. These stents have a big enough diameter to facilitate adequate drainage and even perform endoscopic necrosectomy through them.1 They have also been used successfully for endoscopic drainage of the bile duct (choledochoduodenostomy), treatment of acute cholecystitis in patients with high surgical risk (cholecystogastrostomy) and to perform gastroenteroanastomosis in patients with gastric outflow tract obstruction or other indications (enable endoscopic retrograde cholangiopancreatography [ERCP] in patients with Roux-en-Y anatomy).2
The incidence of admissions for peptic ulcer is declining. The most common complication is gastrointestinal bleeding. Perforation is less common; it usually manifests as an acute abdomen with a CT finding of pneumoperitoneum and requires urgent surgery in most cases. Less often, if the perforation is contained by neighbouring organs or if concomitant treatments interfere with its clinical course, it can present in a more latent form, giving rise to an intra-abdominal abscess.3 We have presented a case of intra-abdominal abscess secondary to a perforated duodenal ulcer with an atypical clinical presentation, which we were able to completely resolve by inserting a lumen-apposing stent. There is very little evidence on the use of this technique for the drainage of non-pancreatic intra-abdominal collections. It has mainly been used for post-surgical collections, with good outcomes.4 A Spanish series of 18 intra-abdominal abscesses, which were neither pancreatic nor postoperative, recently reported high technical and clinical success rates (both 88.9%) for endoscopic ultrasound drainage, including eight lumen-apposing stents and ten conventional metal or plastic stents.5 Although controlled studies are required, using our case as illustration, we believe this technique could be useful for the management of intra-abdominal abscesses.
Conflicts of interestThe authors declare that they have no conflicts of interest.
FundingThis study has received no specific funding from public, private or non-profit organisations.
Please cite this article as: Hijos G, Abad D, Laredo V, Alfaro E, Cañamares P, García S, et al. Absceso secundario a úlcera péptica complicada resuelto mediante drenaje guiado por ecoendoscopia con prótesis de aposición luminal. Gastroenterol Hepatol. 2021;44:128–130.