The main clinical practice guidelines recommend endoscopy within 24h after admission to the Emergency Department in patients with non-variceal upper gastrointestinal bleeding. However, it is a wide time frame and the role of urgent endoscopy (<6h) is controversial.
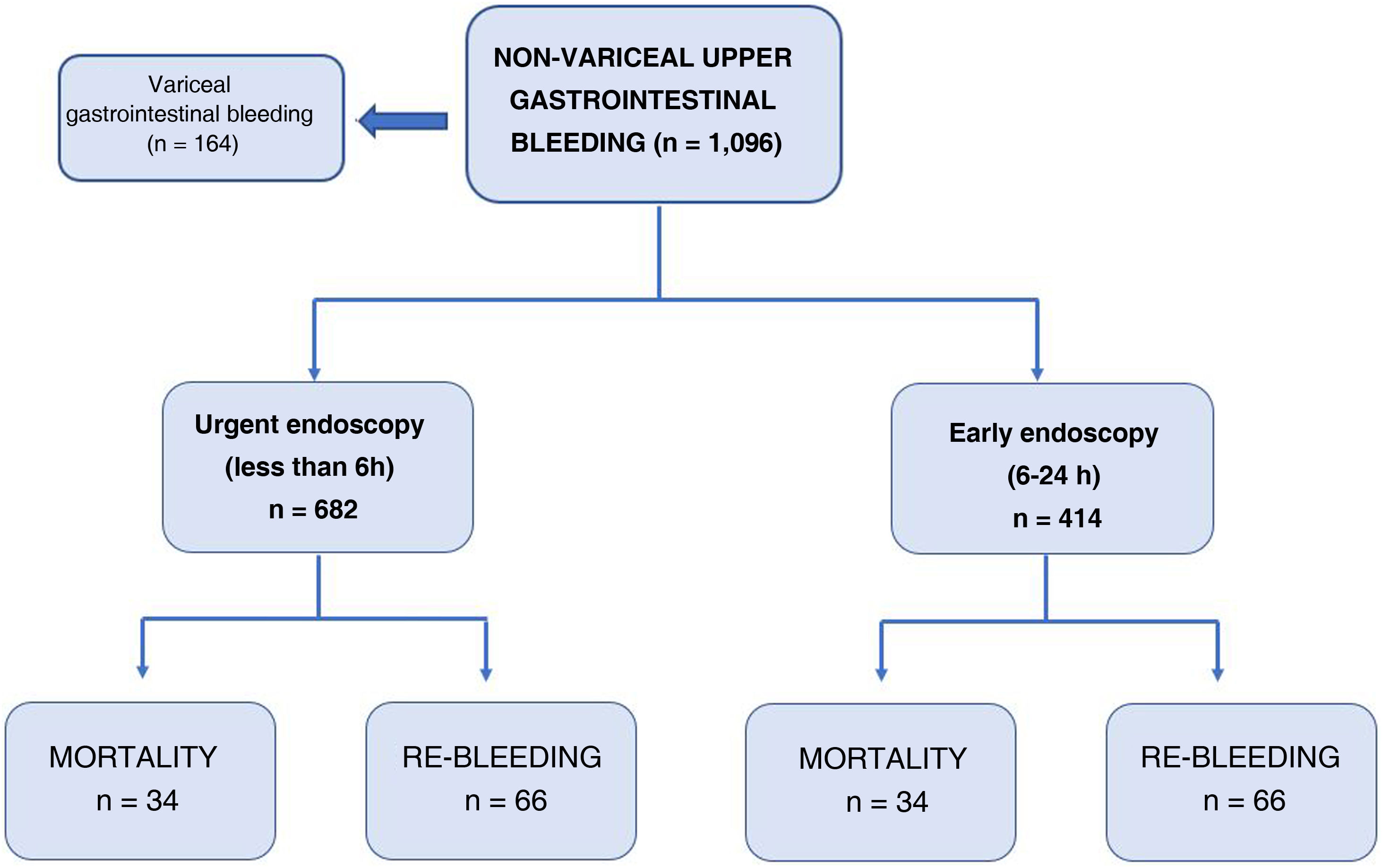
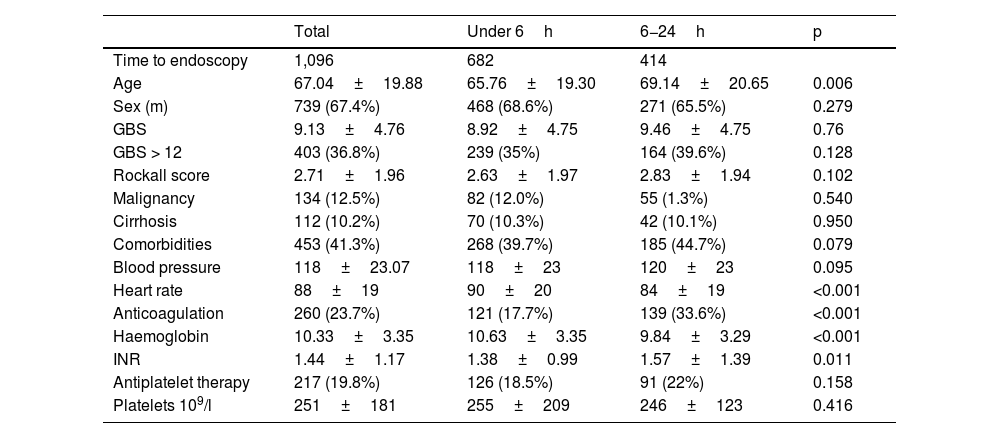
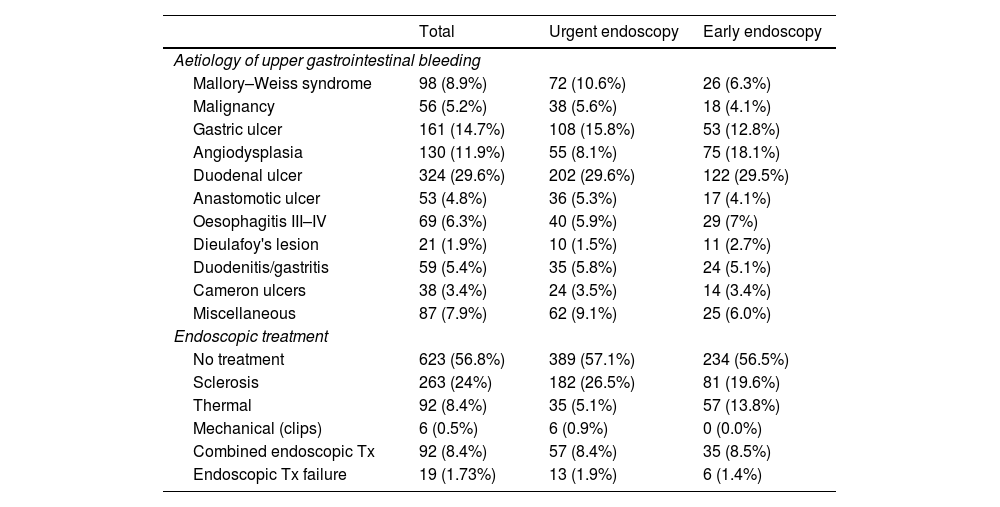
Material and methodsProspective observational study carried out at La Paz University Hospital, where all patients were selected, from January 1, 2015 to April 30, 2020, who attended the Emergency Room and underwent endoscopy for suspected upper gastrointestinal bleeding. Two groups of patients were established: urgent endoscopy (<6h) and early endoscopy (6−24h). The primary endpoint of the study was 30-day mortality.
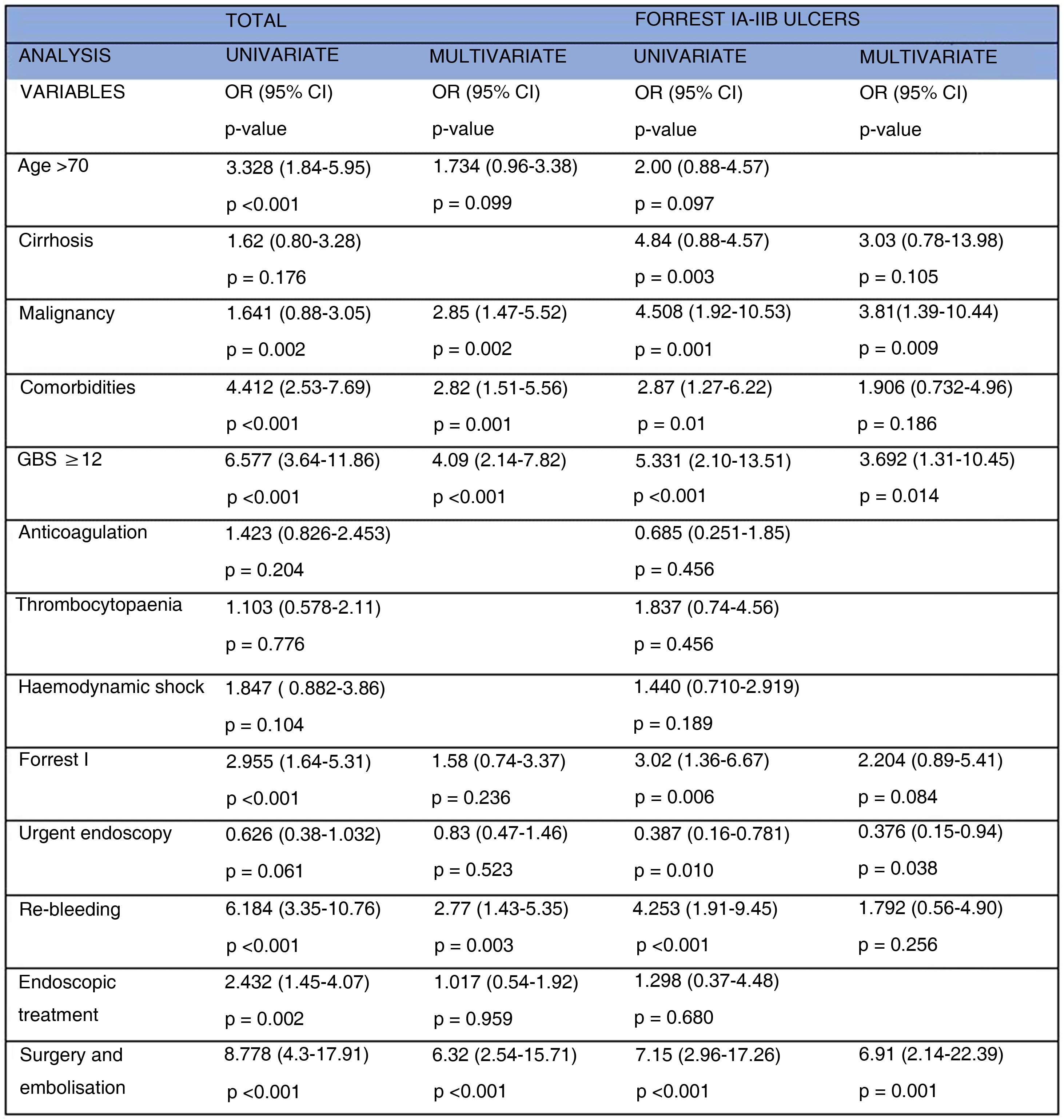
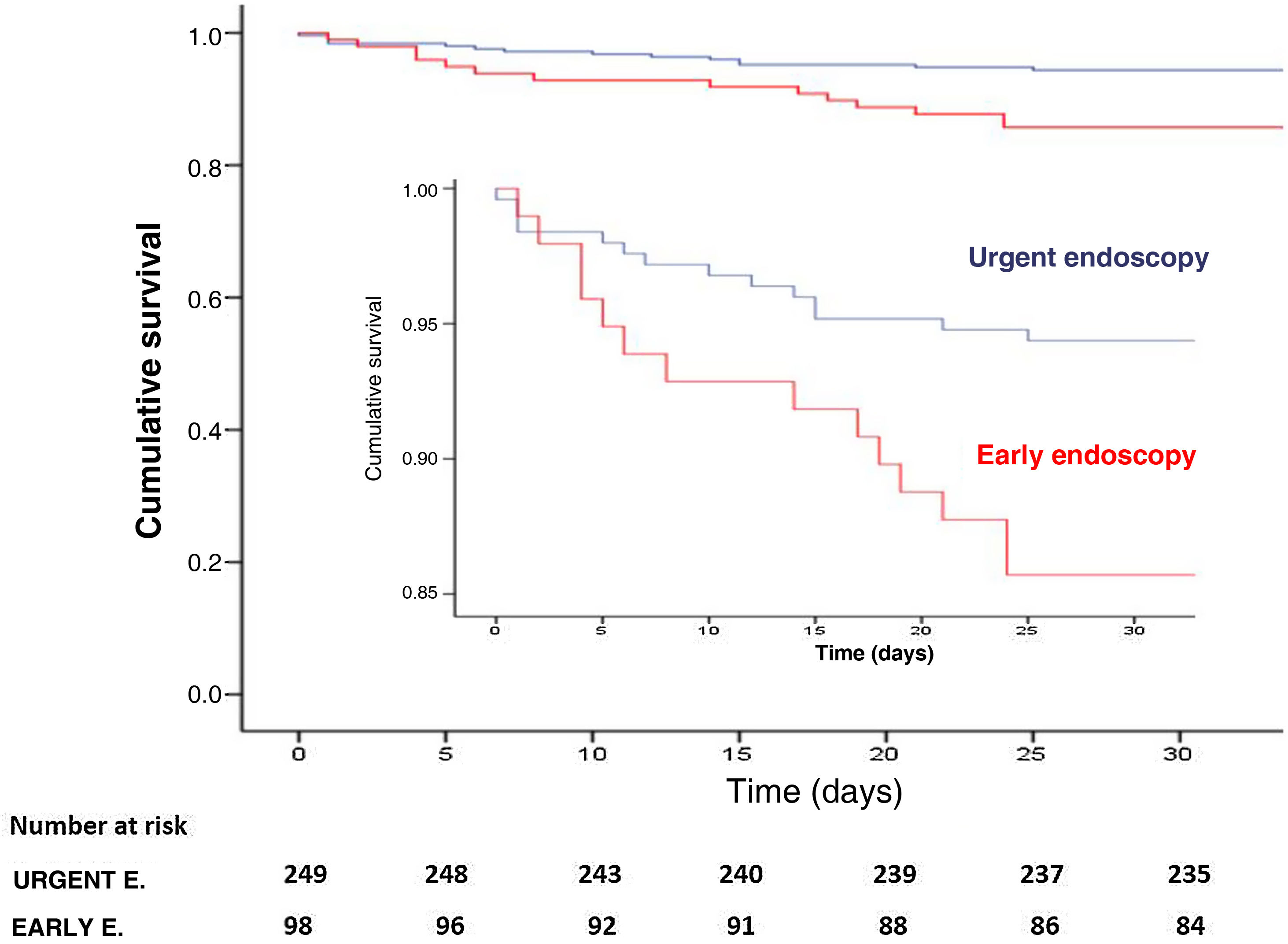
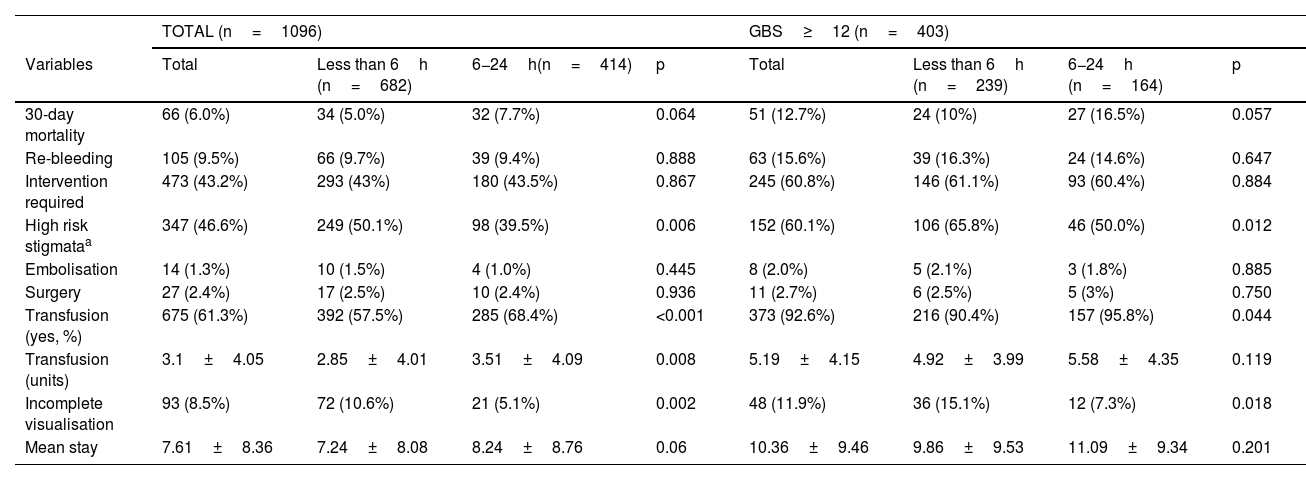
ResultsA total of 1096 were included, of whom 682 underwent urgent endoscopy. Mortality at 30 days was 6% (5% vs. 7.7%, p=0.064) and rebleeding was 9.6%. There were no statistically significant differences in mortality, rebleeding, need for endoscopic treatment, surgery and/or embolization, but there were differences in the necesity for transfusion(57.5% vs. 68.4%, p<0.001) and the number of concentrates of transfused red blood cells(2.85±4.01 vs. 3.51±4.09, p=0.008).
ConclusionUrgent endoscopy, in patients with acute upper gastrointestinal bleeding, as well as the high-risk subgroup (GBS≥12), was not associated with lower 30-day mortality than early endoscopy. However, urgent endoscopy in patients with high-risk endoscopic lesions (Forrest I-IIB), was a significant predictor of lower mortality. Therefore, more studies are required for the correct identification of patients who benefit from this medical approach (urgent endoscopy).
Las principales guías de práctica clínica recomiendan la realización de endoscopia dentro de las 24horas posteriores a la admisión en Urgencias en pacientes con hemorragia digestiva alta no variceal. Sin embargo, es un margen de tiempo muy amplio y el papel de la endoscopia urgente (<6horas) es controvertido.
Material y métodosEstudio prospectivo observacional realizado en Hospital Universitario La Paz, donde son seleccionados todos los pacientes, desde el 1 de enero de 2015 hasta el 30 de abril de 2020, que acudieron a Urgencias y fueron sometidos a endoscopia por sospecha de hemorragia digestiva alta. Se establecieron dos grupos de pacientes: endoscopia urgente (<6horas) y precoz(6−24horas). El objetivo primario del estudio fue la mortalidad a los 30 días.
ResultadosUn total de 1096 fueron incluidos, de los cuales 682 fueron sometidos a endoscopia urgente. La mortalidad a los 30 días fue del 6% (5% vs. 7,7%, p=0,064) y del resangrado del 9,6%. No hubo diferencias estadísticamente significativas en la mortalidad, resangrado, necesidad de tratamiento endoscópico, cirugía y/o embolización, pero sí en la necesidad de transfusión (57,5% vs. 68,4%, p<0,001) y el número de concentrados de hematíes transfundidos (2,85+/-4,01 vs. 3,51+/-4,09, p=0,008).
ConclusiónLa endoscopia urgente, en pacientes con hemorragia digestiva alta aguda, también el subgrupo de alto riesgo (GBS≥12), no se asoció con una mortalidad menor a los 30 días que la endoscopia precoz. Sin embargo, en los pacientes con lesiones endoscópicas de alto riesgo (Forrest I-IIB), fue un predictor significativo de menor mortalidad. Por lo tanto, se requieren más estudios para la identificación correcta de pacientes, que se beneficien de esta actitud médica (endoscopia urgente).