La hipertensión arterial (HTA) representa el principal factor de riesgo individual, con mayor carga a nivel mundial de enfermedades cardiovasculares (ECV). En nuestro país, algunos trabajos epidemiológicos han mostrado marcadas diferencias en las prevalencias de estos factores de riesgo de acuerdo con la población evaluada. Sin embargo, no hay estudios epidemiológicos de evaluación de factores de riesgo cardiovascular exclusivos referentes a barrios vulnerables con muy bajos recursos económicos, socioculturales y poca accesibilidad a los sistemas de salud.
Materiales y métodosEstudio observacional de corte transversal multicéntrico en habitantes de comunas vulnerables de muy bajos recursos, como asentamientos populares y barrios carenciados con muestreo aleatorizado simple de casas.
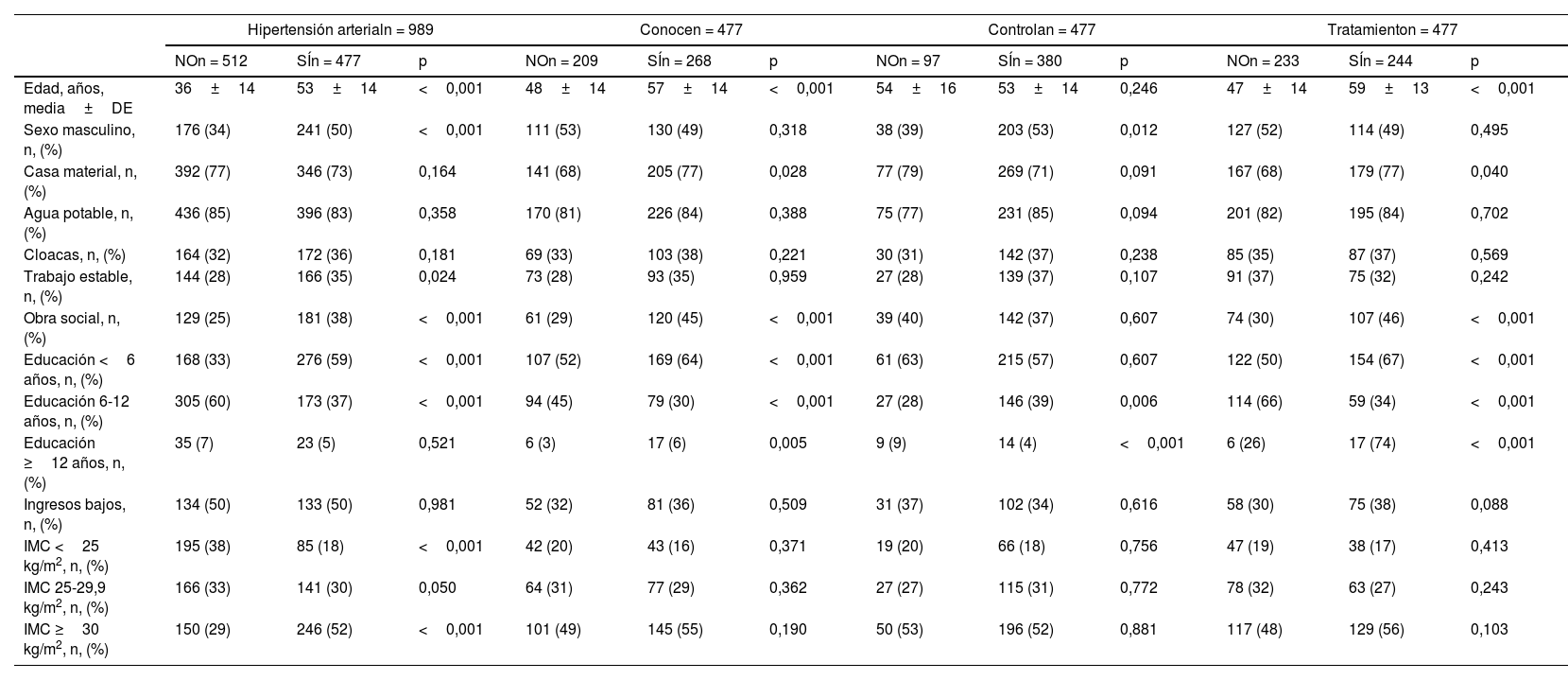
Se realizaron tomas de presión arterial (PA), medidas antropométricas, así como cuestionarios epidemiológicos, económicos y socioculturales.
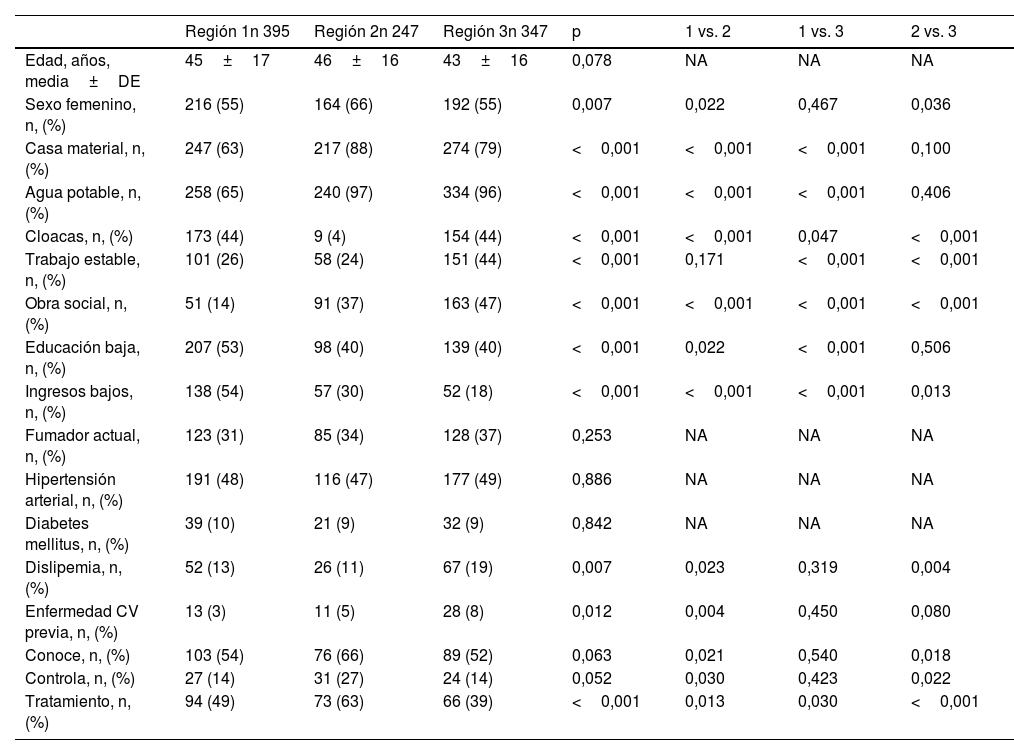
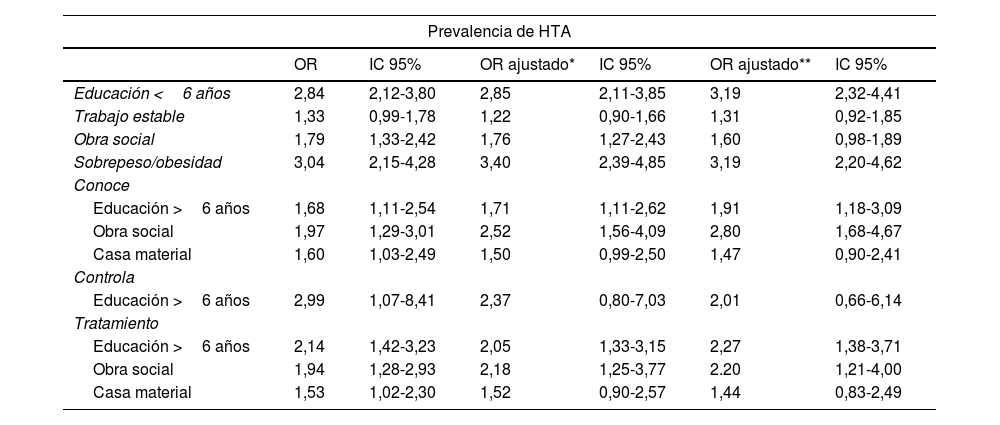
Se describen los hallazgos: prevalencia, conocimiento y control de la PA en las distintas regiones. Se efectuó una regresión logística para determinar las variables independientes a los resultados principales.
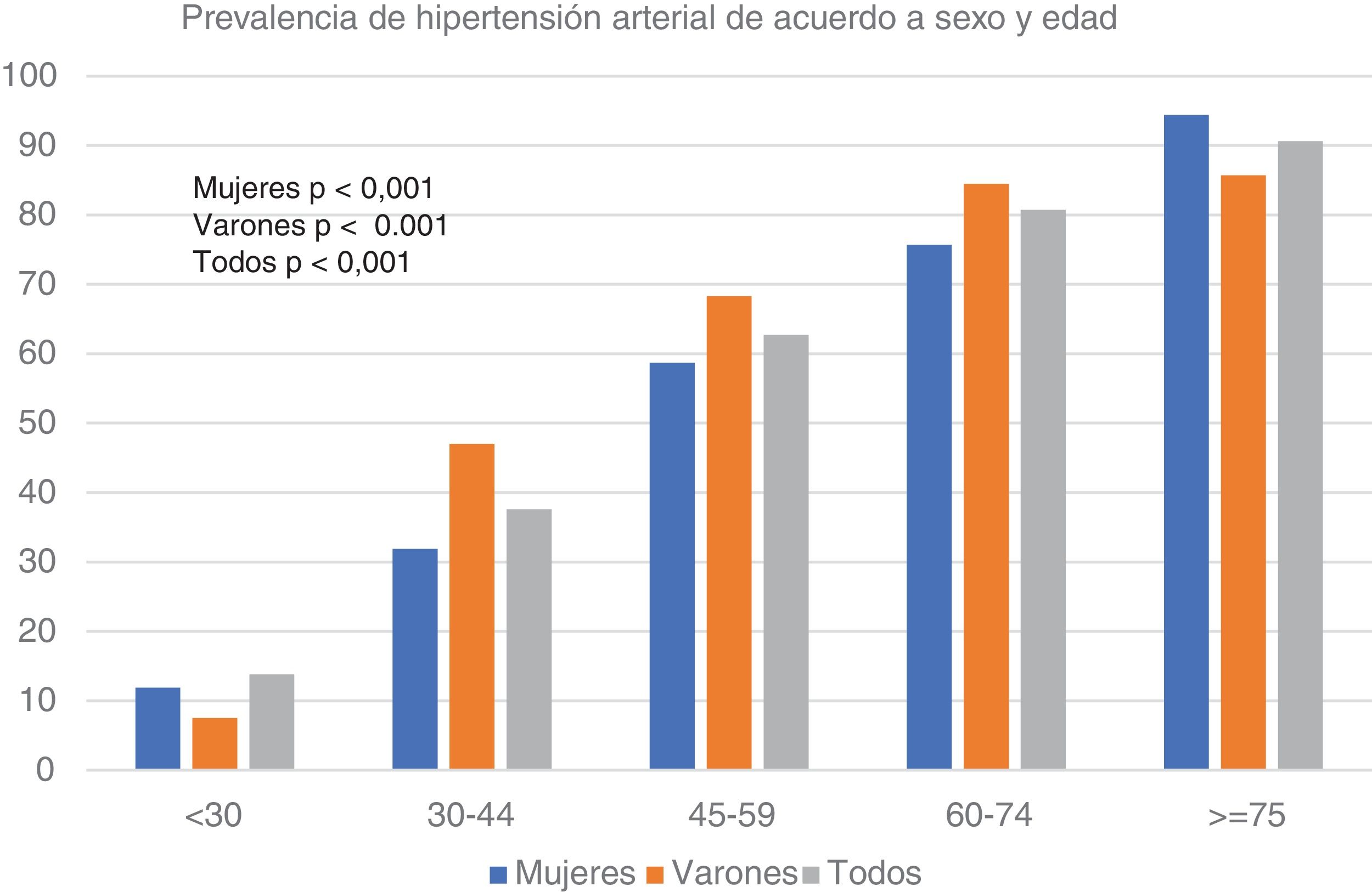
ResultadosSe analizaron 989 participantes. La prevalencia de HTA global fue de 48,2%. Un total de 82% tenía un índice de masa corporal (IMC) >25 kg/m2. De estos pacientes, 45,3% tenían menos de seis años de educación. Este último aspecto se asoció a mayor prevalencia de HTA de forma independiente.
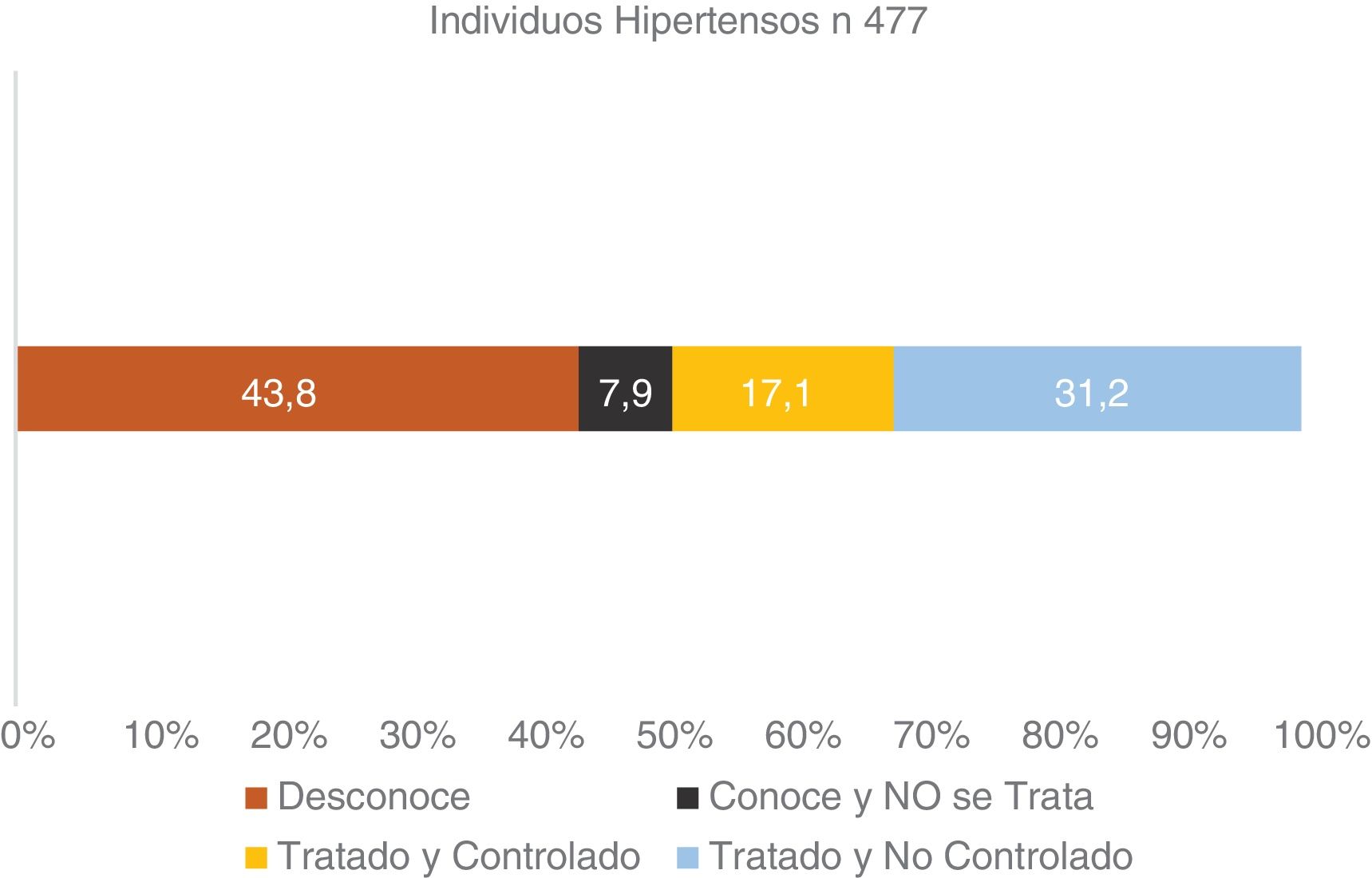
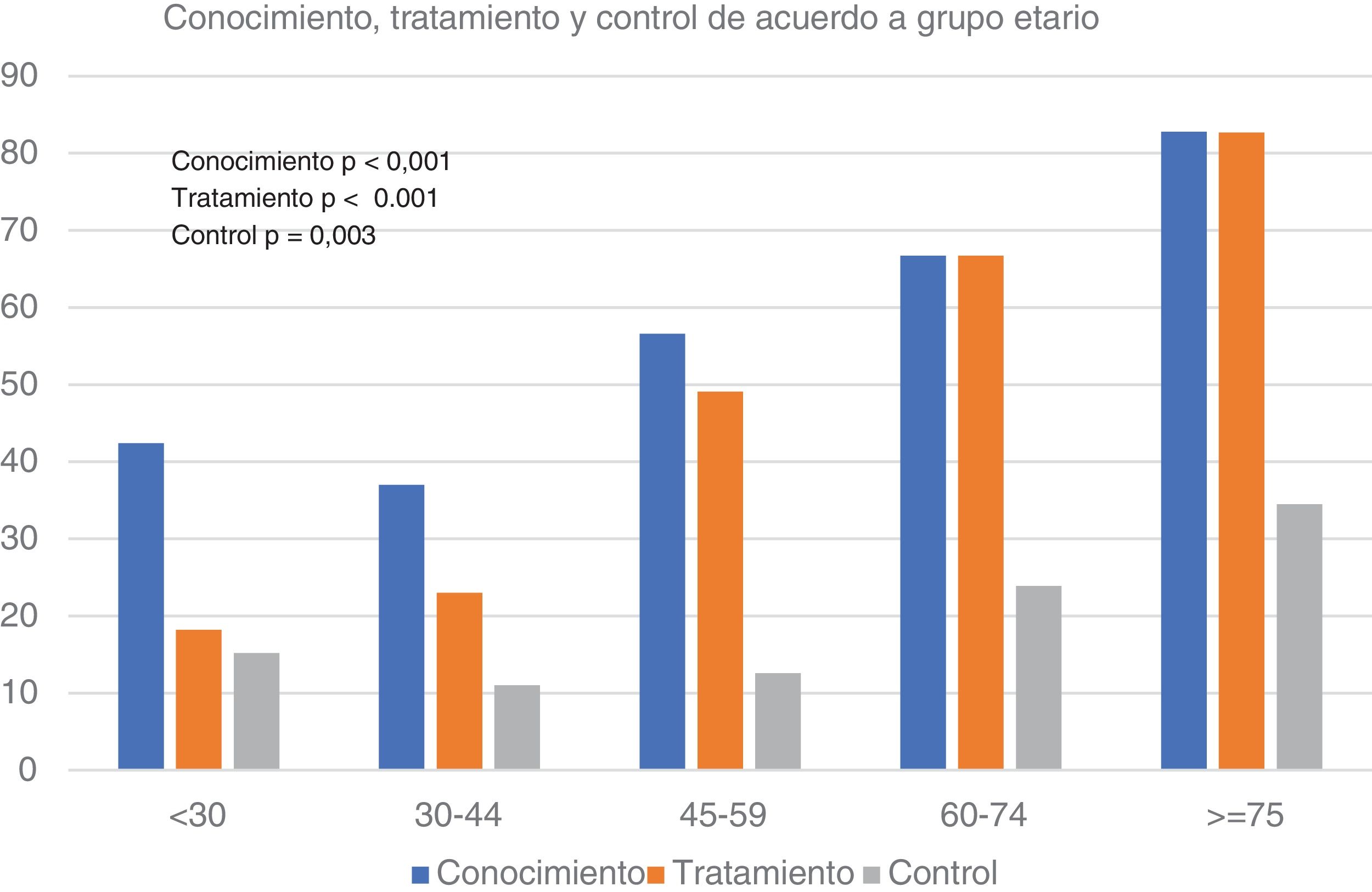
De los hipertensos, 44% desconocían su padecimiento y solo en 17,2% estaba controlado, asociándose esto a tener obra social (OS) y mayor nivel educativo. Únicamente 24% estaban bajo tratamiento combinado.
ConclusiónLa prevalencia de HTA en barrios vulnerables es elevada, superando a la de otros estratos sociales con niveles de conocimiento, tratamiento y control de la HTA bajos, similar a otras poblaciones. Se detectó un uso insuficiente de la terapia combinada.
Hypertension (HTN) represents the primary individual risk factor, contributing significantly to the global burden of cardiovascular diseases (CVD). In our country, epidemiological research has highlighted substantial variations in the prevalence of these risk factors across different populations. However, there is a lack of epidemiological studies assessing exclusive cardiovascular risk factors within vulnerable neighborhoods characterized by extremely limited economic resources, sociocultural challenges, and inadequate healthcare access.
MethodsA multicenter cross-sectional observational study was conducted among individuals residing in economically deprived and marginalized communities, including informal settlements and underprivileged neighborhoods. Simple random sampling of households was employed.
Blood pressure measurements, anthropometric assessments, and epidemiological, economic, and sociocultural questionnaires were administered.
Results encompass prevalence rates, awareness levels, and blood pressure control across diverse regions. Logistic regression was utilized to identify independent variables influencing primary outcomes.
ResultsA total of 989 participants were analyzed. The overall prevalence of hypertension was 48.2%. About 82% had a body mass index (BMI) >25. Approximately 45.3% had less than 6 years of formal education. Independent association was established between education levels below 6 years and higher hypertension prevalence.
Among hypertensive individuals, 44% were unaware of their condition, with only 17.2% achieving control, correlated with having health insurance and a higher educational background. Merely 24% were receiving combined therapy.
ConclusionThe prevalence of hypertension within vulnerable neighborhoods is alarmingly high, surpassing rates in other social strata. Knowledge, treatment, and control levels of hypertension are suboptimal, comparable to other populations. Inadequate use of combination therapy was observed. This study underscores the urgent need for targeted interventions addressing cardiovascular risk factors in poor areas to mitigate the burden of CVD.