Fibromyalgia is a chronic pain syndrome that depressive symptoms can aggravate. The aim of the present study was to test the efficacy of Personal Construct Therapy (PCT), an approach that emphasizes identity features and interpersonal meanings as the focus of the treatment of depressive symptoms, in women with fibromyalgia.
MethodWe compared PCT with Cognitive Behavioral Therapy (CBT) in a multicenter parallel randomized trial. Women with fibromyalgia and depressive symptoms (n = 106) were randomly allocated to CBT (n = 55) or PCT (n = 51) in individual and modular formats to adjust to their needs. Analysis was by linear mixed-effects models.
ResultsParticipants in both conditions had significantly reduced depressive symptoms, and we found no significant difference when comparing groups both post-treatment (β = -0.47, t = -0.49, p = .63) and at follow-up (β = -1.12, t = -1.09, p = .28). Results were similar between conditions for anxiety, fibromyalgia's impact, and the distribution of clinically significant changes in depressive symptoms and pain.
ConclusionsPCT and CBT seem to be equally effective in the treatment of depressive symptoms, making PCT a viable alternative treatment.
La fibromialgia es un trastorno de dolor crónico que los síntomas depresivos agravan. El objetivo del estudio es probar la eficacia de la Terapia de Constructos Personales (TCP), aproximación que enfatiza las características identitarias y los significados personales como foco de la intervención, para el tratamiento de síntomas depresivos en mujeres con fibromialgia.
MétodoComparamos la TCP con la Terapia Cognitivo-Conductual (TCC) en un ensayo multicéntrico paralelo aleatorizado. Mujeres con fibromialgia y síntomas depresivos (n = 106) fueron aleatorizadas a TCC (n = 55) o TCP (n = 51), en formato individual y modular para ajustarse a las necesidades de las pacientes. Los datos se analizaron usando modelos lineales de efectos mixtos.
ResultadosAmbas condiciones redujeron significativamente los síntomas depresivos sin encontrarse diferencias significativas después del tratamiento (β = -0,47, t = -0,49, p = 0,63) ni en el seguimiento (β = -1,12, t = -1,09, p = 0,28). Resultados similares se encontraron para la ansiedad, el impacto de la fibromialgia, la distribución del cambio clínicamente significativo para los síntomas depresivos y el dolor.
ConclusionesLa TCP y la TCC parecerían ser igualmente efectivas para el tratamiento de los síntomas depresivos, postulando la TCP como una alternativa de tratamiento.
Fibromyalgia is a chronic and disabling pain syndrome affecting the musculoskeletal system that has a worldwide prevalence of approximately 1.78% and a higher prevalence among women than men (3.98% vs 0.01%; Heidari et al., 2017). Depressive symptoms occur significantly more often in fibromyalgia than in other chronic pain diseases, having a life-time prevalence of 63% to 65% (Kleykamp et al., 2021; Løge-Hagen et al., 2019), and some studies suggest a bidirectional relationship (Aguilera et al., 2019; IsHak et al., 2018; Sarzi-Puttini et al., 2020). Patients with fibromyalgia who experience depressive symptoms have more sleep disturbances, poorer sexual health, lower levels of physical functioning, and poorer quality of life (Carta et al., 2018; Galvez-Sánchez et al., 2019; Steiner et al., 2017). The economic burden of comorbid fibromyalgia and depression is also larger than the additive costs for each diagnosis alone (Robinson et al., 2004). Everything considered, it seems relevant to include the treatment of depressive symptoms in the management of fibromyalgia.
Strong evidence underpins various treatments for fibromyalgia, including medication, moderate physical exercise, and psychological interventions (Clauw, 2014; Fitzcharles et al., 2013; Pardos-Gascón et al., 2021). Regarding the psychological interventions, meta-analyses indicate effect size ranging from small to moderate for the most researched therapy, cognitive behavioral therapy (CBT; Bernardy et al., 2018). Given the complexity of the therapeutic response in patients with fibromyalgia, recommendations also favor customizing psychological treatments to patient needs (Morley et al., 2013), placing a special focus on physical functioning and psychological symptoms (especially depressive), and adjusting treatment duration to achieve long-term effects.
The Theory of Personal Constructs (Kelly, 1955) has an eminently idiographic approach in which the aspects related to self-identity and interpersonal perception are fundamental. Personal construct therapy (PCT) has moderately favorable evidence in several meta-analyses (Metcalfe et al., 2007), with support for its use in the treatment of depression (Feixas et al., 2016, 2018) and some preliminary support for its use in the treatment of fibromyalgia (Aguilera et al., 2018). This therapy benefits from emphasizing working with the person's own meanings rather than building the intervention upon prespecified diagnostic labels or clinical criteria, which many fibromyalgia patients report to be ambiguous (Mengshoel et al., 2018). In addition, some studies (e.g., Compañ et al., 2011; Turner et al., 2021) suggest that the way self and pain are construed plays an important role in fibromyalgia, and this is precisely the focus of PCT (rather than targeting symptoms and behaviors).
The aim of the present study was to test the efficacy of PCT for treating depressive symptoms in women with fibromyalgia, using CBT, a well-established treatment, for comparison. First, we tested the hypothesis that PCT was more statistically and clinically efficacious than CBT for reducing depressive symptoms among women with fibromyalgia; and second, that PCT was more efficacious than CBT for reducing anxiety symptoms and improving health status.
MethodStudy design and randomizationThis multicenter randomized study had two parallel groups into which we allocated women who met the eligibility criteria. A staff member of the Universitat de Barcelona not involved in the trial and blinded to treatment conditions, performed randomization (1:1 for CBT:PCT) by computer-generated allocation permuted block sequence. We included stratification by the public health service (two mental health centers and eight primary care centers) from which we recruited participants and delivered treatment (Paz et al., 2020). The clinical trial was registered in Clinicaltrials.gov (NCT02711020) in March 2016 prior to participant recruitment. The Bioethics Committee of the Barcelona University (IRB00003099) and the ethics committees of each recruiting center have approved this trial.
ParticipantsOnly women diagnosed with fibromyalgia were included due to the low reported prevalence among men (Gayà et al., 2020; Heidari et al., 2017). Other inclusion criteria were: (1) age 18–70 years, (2) and current depressive symptoms, as evidenced by scores > seven on the Hospital Anxiety and Depression Scale (HADS-D; Zigmond & Snaith, 1983). Exclusion criteria included: (1) current or past severe mental disorder, intellectual disability, or organic brain dysfunction; (2) current psychological treatment; (3) inability to communicate in Spanish or Catalan; and (4) substantial visual, hearing, or cognitive deficit.
We estimated a required sample size of 90 patients (45 per condition) by considering an effect size ≥ 0.30, a statistical power of 0.80, and a Type 1 error level of 5% (one-sided). Given an expected drop-out rate of 20%, we planned to recruit 112 patients (56 per condition).
ProcedureRecruitment started in March 2016. Medical staff from recruiting centers explained the nature of the study to potentially eligible patients. Those who agreed to take part gave written consent. We assessed eligible participants in two sessions of approximately 90 minutes each (see Paz et al., 2020), followed by assessments after treatment ended and follow-up assessments six months later. The study ended in December 2019. The evaluators were always blinded to the therapeutic condition.
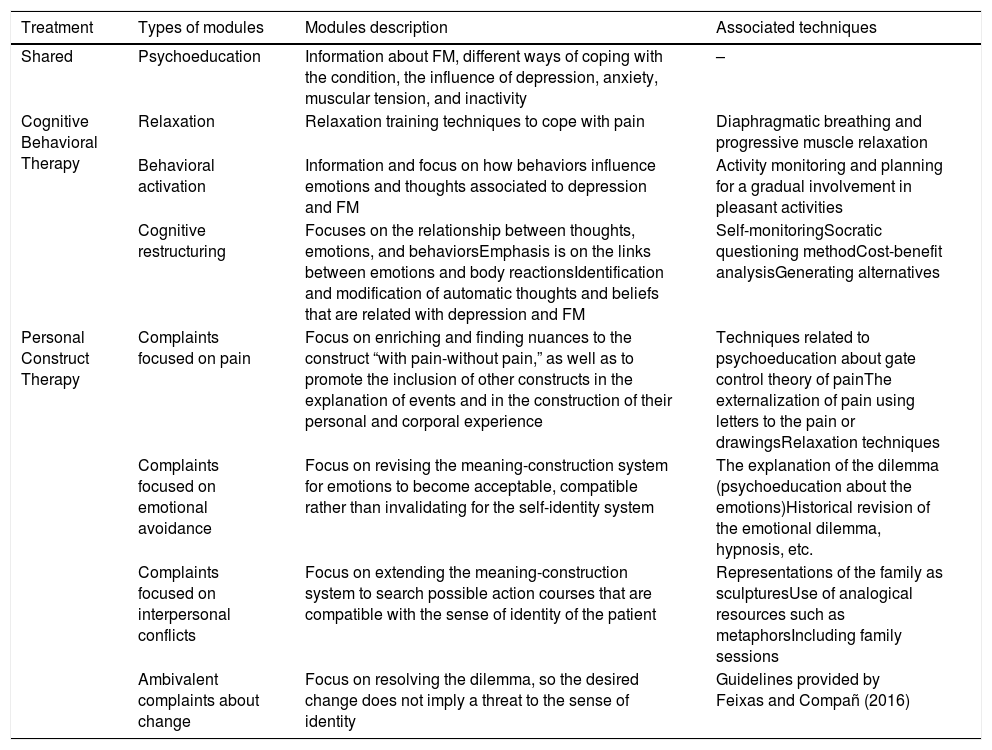
Thirteen therapists trained in psychotherapy (i.e., who completed at least the first year of a master's degree related to CBT or PCT) delivered therapy (n = 13) under weekly supervision by senior mentors who specialized in each therapy approach. We limited the two psychological treatments to 18 sessions that lasted 1 hour each and including a family member if relevant. In the 3–5 months after treatment ended, the therapist or patient could seek a maximum of three booster sessions (one hour each) based on need. Both treatments were offered in modular format based on the clinical formulation of cases and shared a common psychoeducational component. The order in which therapists applied modules could vary with patient need (see Table 1).
Types of modules in Cognitive Behavioral and Personal Construct Therapies for depressive symptoms in fibromyalgia.
| Treatment | Types of modules | Modules description | Associated techniques |
|---|---|---|---|
| Shared | Psychoeducation | Information about FM, different ways of coping with the condition, the influence of depression, anxiety, muscular tension, and inactivity | – |
| Cognitive Behavioral Therapy | Relaxation | Relaxation training techniques to cope with pain | Diaphragmatic breathing and progressive muscle relaxation |
| Behavioral activation | Information and focus on how behaviors influence emotions and thoughts associated to depression and FM | Activity monitoring and planning for a gradual involvement in pleasant activities | |
| Cognitive restructuring | Focuses on the relationship between thoughts, emotions, and behaviorsEmphasis is on the links between emotions and body reactionsIdentification and modification of automatic thoughts and beliefs that are related with depression and FM | Self-monitoringSocratic questioning methodCost-benefit analysisGenerating alternatives | |
| Personal Construct Therapy | Complaints focused on pain | Focus on enriching and finding nuances to the construct “with pain-without pain,” as well as to promote the inclusion of other constructs in the explanation of events and in the construction of their personal and corporal experience | Techniques related to psychoeducation about gate control theory of painThe externalization of pain using letters to the pain or drawingsRelaxation techniques |
| Complaints focused on emotional avoidance | Focus on revising the meaning-construction system for emotions to become acceptable, compatible rather than invalidating for the self-identity system | The explanation of the dilemma (psychoeducation about the emotions)Historical revision of the emotional dilemma, hypnosis, etc. | |
| Complaints focused on interpersonal conflicts | Focus on extending the meaning-construction system to search possible action courses that are compatible with the sense of identity of the patient | Representations of the family as sculpturesUse of analogical resources such as metaphorsIncluding family sessions | |
| Ambivalent complaints about change | Focus on resolving the dilemma, so the desired change does not imply a threat to the sense of identity | Guidelines provided by Feixas and Compañ (2016) |
Note. FM = Fibromyalgia.
The CBT protocol followed previous treatment programs for patients with fibromyalgia (Comeche Moreno et al., 2010), with three main modules: relaxation, behavioral activation, and cognitive restructuring. Regarding the PCT protocol, it was designed following in previous literature regarding case formulation (Winter & Procter, 2013), informed by experience in a pilot study (Aguilera et al., 2018). Common patient requests dictated four possible courses of action with specific objectives and techniques (see Paz et al., 2020). The repertory grid technique, a semi-structured interview, was used to assess self-concept, cognitive structure, and cognitive conflicts. The results from this assessment helped to determine the possible course of cation.
Treatment adherenceAll sessions were audio-recorded and 10 of these sessions were randomly selected and their contents was assessed by two independent researchers. We created a 50-item scale to evaluate treatment adherence. Kappa analyses revealed high levels of agreement between evaluators for both treatment conditions (kPCT = .69, kCBT = .67) and moderate levels of agreement for the common scale (kcommon = .52, p <.001).
MeasuresConcerning the primary outcome, depressive symptoms, assessment was by the Hospital Anxiety and Depression Scale (Terol-Cantero et al., 2015; Zigmond & Snaith, 1983). It has acceptable psychometric properties (Vallejo et al., 2012), and its exclusion of somatic symptoms made this scale useful for detecting depressive symptoms in patients with fibromyalgia (Cabrera et al., 2015; Veltri et al., 2012)
The following measures were used as secondary outcomes. The Hamilton Depression Rating Scale (HDRS; Hamilton, 1960; Ramos-Brieva, 1986) assessed the severity of depressive symptoms, as rated by a clinician, while the anxiety scale of the HADS (HADS-A) assessed anxiety symptomatology. The Fibromyalgia Impact Questionnaire (Burckhardt et al., 1991; Esteve-Vives et al., 2007), which is sensitive to change after treatment (Bennett, 2005), assessed the impact of fibromyalgia. The Visual Analog Scale for Pain (Price et al., 1983) assessed pain intensity.
After treatment, we asked participants to rate their satisfaction with treatment using a question extracted from the Consumer Reports Effectiveness Scale (Feixas et al., 2012).
Statistical analysesTo ensure homogeneity between treatment groups at baseline, we compared the clinical and sociodemographic characteristics using Student's t-tests for continuous variables and the Fisher exact probability test for categorical variables. The baseline and clinical characteristics of those who completed the intervention and those who dropped out were treated the same. Therapist adherence was analyzed by comparing the scores for PCT and CBT using non-parametric Mann-Whitney U tests.
To test the efficacy of therapy, we conducted a series of analyses for the primary and the secondary outcomes on an intention-to-treat basis among randomized participants. We assumed missing data was missing at random. Linear mixed-effect models, with parameters estimated using the restricted maximum likelihood method, were performed to account for the correlation between repeated measures in each participant. The regression coefficients and their 95% confidence intervals were calculated for the interaction of interest (treatment by time). We checked the assumptions of linearity and normality of the residuals visually in QQ plots for each model (all assumptions met). We calculated Hedges’ coefficient to express the within-treatment effect size from pre-treatment to post-treatment and from pre-treatment to follow-up, as well as between treatments. We replicated the analyses on a per-protocol basis, considering only those participants who completed treatment and at least the post-treatment assessment.
To assess the clinical significance of improvement in the primary outcome, we classified the change scores from pre-treatment to post-treatment and from pre-treatment to follow-up using the approach of Jacobson and Truax (1991). We used the data provided by Cabrera et al. (2015) and Terol-Cantero et al. (2015) to calculate the cut-off point for a clinically significant change using criterion C. We also identified those participants with reductions ≥ 20% and ≥ 30% in health symptoms measured by the FIQ and VAS, respectively (Pérez-Aranda et al., 2019). Chi-squared t-tests were used to compare the distribution of participants into categories by treatment condition. For all analyses, we set significance at p < .05 (one-tailed) and used R statistical software (R Core Team, 2020).
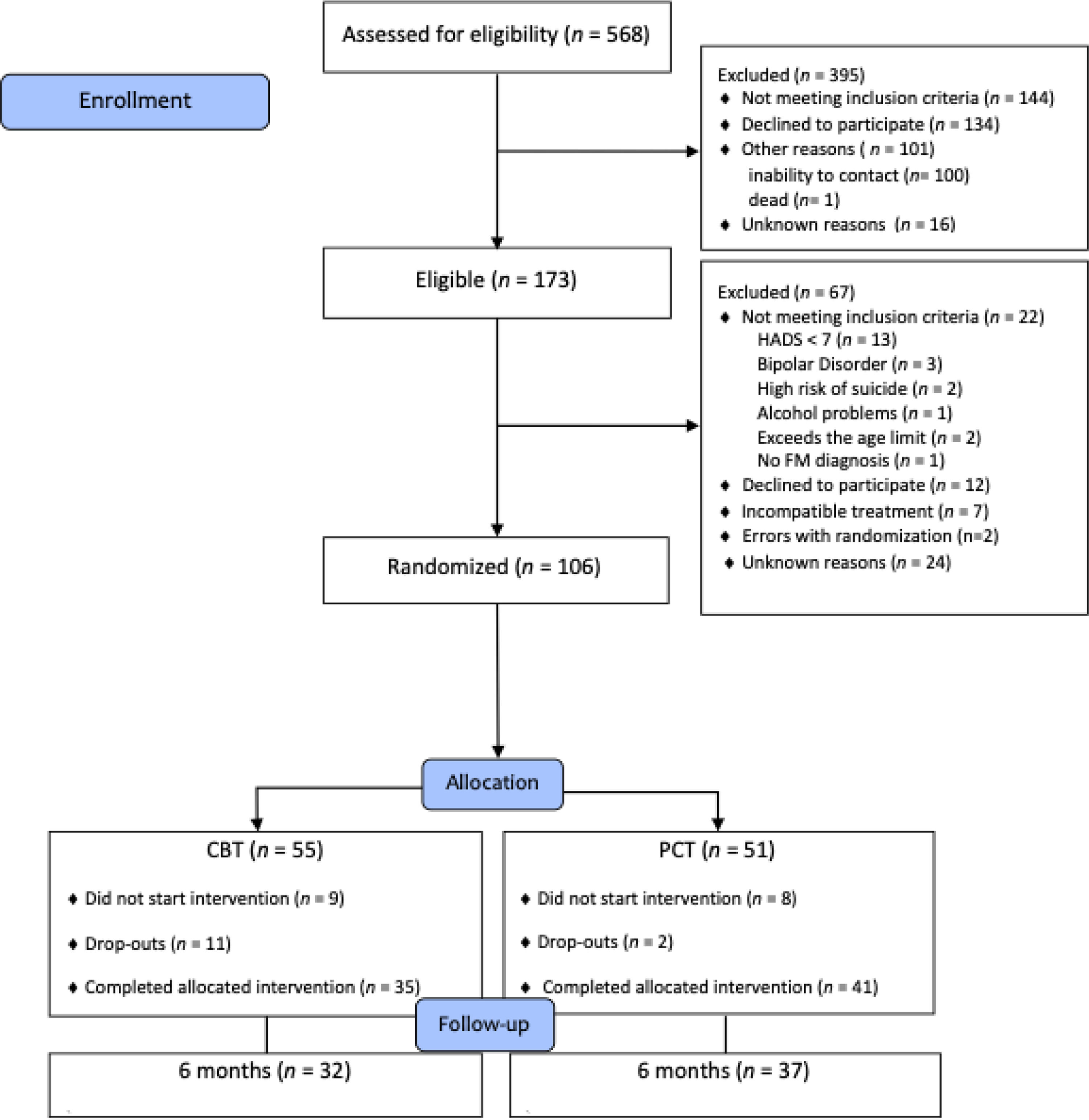
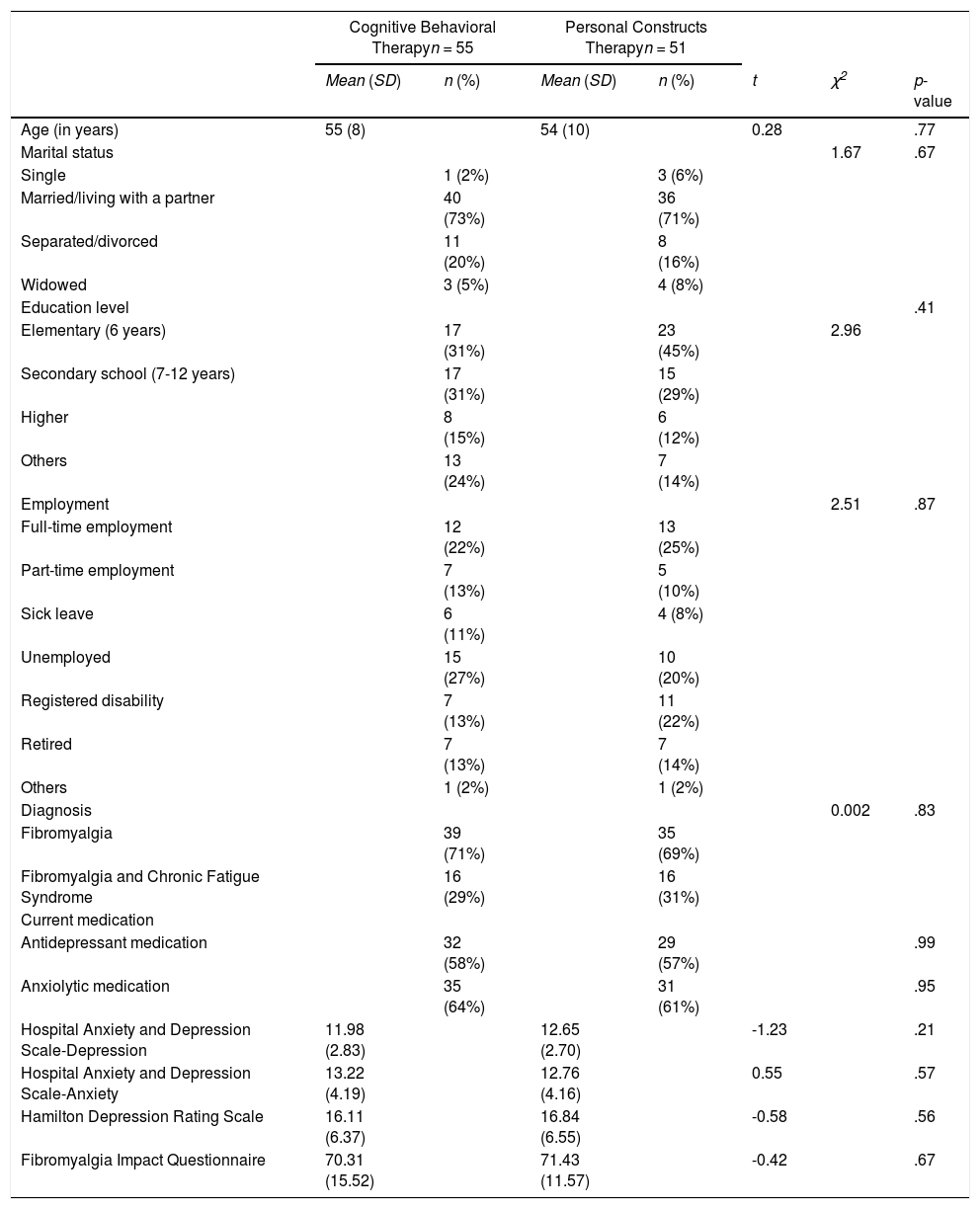
ResultsThe CONSORT diagram presented in Figure 1 shows the participant flow from the eligibility assessment to the follow-up assessment. The drop-out percentages were higher for CBT (36.3% vs. 19.6.3%) but the difference did not reach statistical significance (χ2 (1, N = 106) = 2.88, p = .08, V = 0.18). Also, there were no significant differences in sociodemographic or clinical variables in relation to treatment allocation, demonstrating effective randomization (see Table 2).
Baseline demographic and clinical characteristics of the participants by treatment allocation.
Therapists adhered closely to their respective treatments. When delivering PCT, they scored significantly more on PCT items (Md = 4, n = 10 sessions) than when delivering CBT (Md = 2.5, n = 10), U = 16, z = -2.62, p < .01, r = .59), with the converse being true when delivering (CBT: Md = 7, n = 10; PCT: Md = 1, n = 10, U = 5,5, z = -3.39, p < .001, r = .76) but with a larger effect size. In the common scale, we found non-significant results suggesting that both treatments equally used non-specific cognitive interventions (U = 44.5; p = .64).
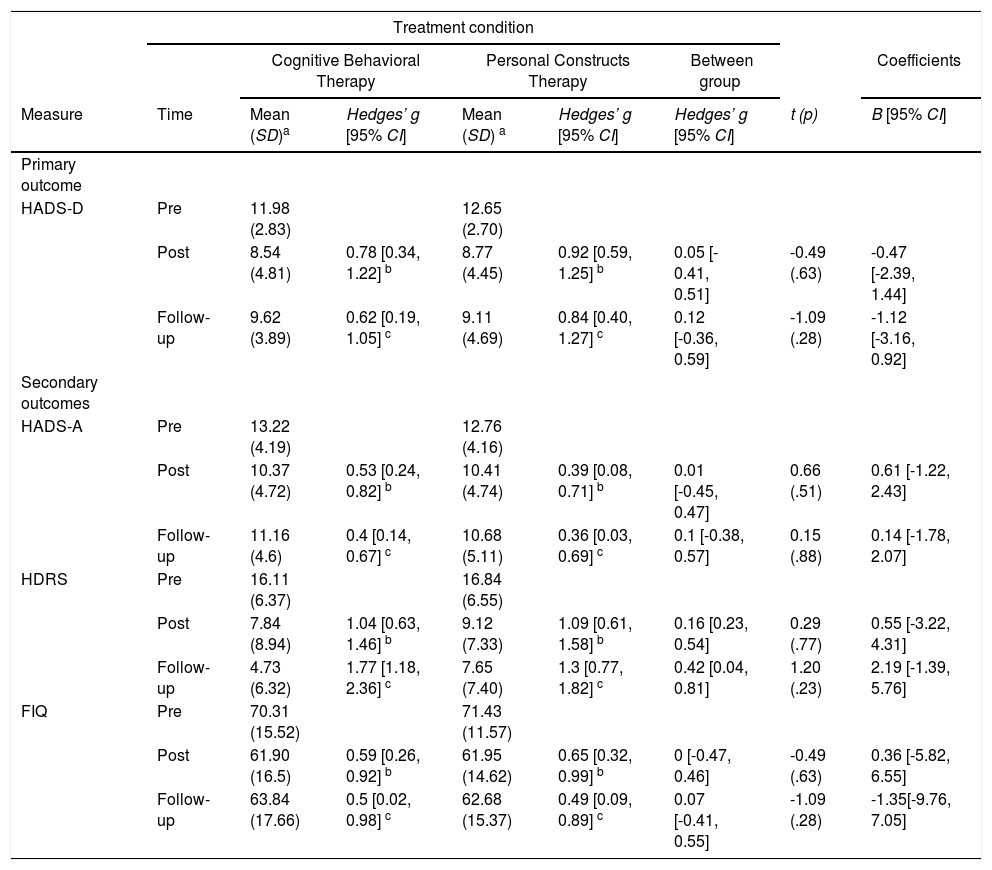
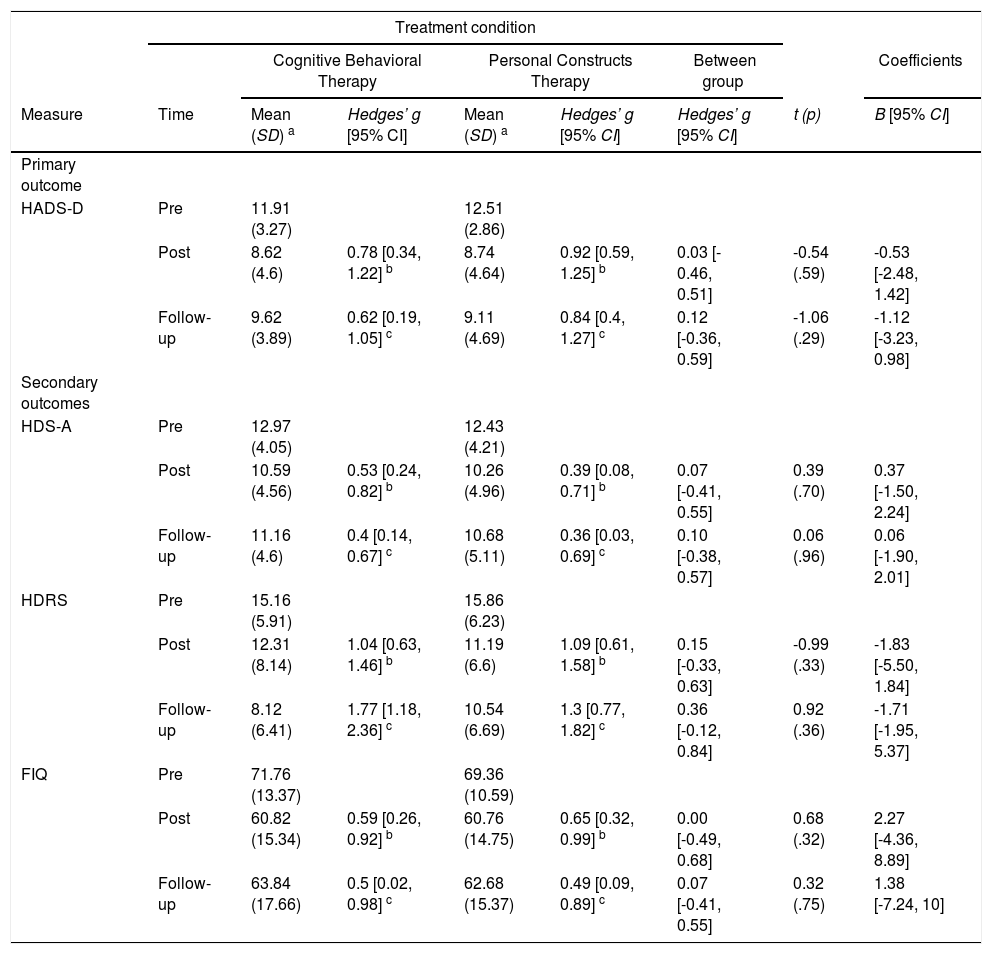
On the intention-to-treat basis (n = 106), the results indicated that both treatments significantly reduced symptoms on the primary outcome measure (HADS-D) after treatment (β = -3.35, t = -4.76, p < .001) and at follow-up (β = -2.35, t = -3.12, p < .001). For depression measured by the HDRS, there were also significant symptom reductions after treatment (β = -8.27, t = -6.25, p < .001) and at follow-up (β = -11.38, t = -9,04, p < .001). For anxiety (HADS-A), symptoms reduced significantly after the intervention (β = -2.59, t = -3.86, p < .001) and at follow-up (β = -1.94, t = -2.74, p = .01). Similar results were obtained for the FIQ after treatment (β = -3.35, t = -4.76, p < .001) and at follow-up (β =-2.35, t = -3.12, p < .001). The effect sizes for the reduction of symptoms in both groups ranged from medium to large, except for some comparisons with the HADS-A. However, we found no significant differences between treatments (see details for comparisons between treatments in Table 3).
Descriptive statistics by outcome scores at all assessment points, effect sizes with 95% confidence intervals within and between groups, and regression coefficients and 95% CI for the interaction (time x treatment), intention-to-treat approach.
| Treatment condition | ||||||||
|---|---|---|---|---|---|---|---|---|
| Cognitive Behavioral Therapy | Personal Constructs Therapy | Between group | Coefficients | |||||
| Measure | Time | Mean (SD)a | Hedges’ g [95% CI] | Mean (SD) a | Hedges’ g [95% CI] | Hedges’ g [95% CI] | t (p) | B [95% CI] |
| Primary outcome | ||||||||
| HADS-D | Pre | 11.98 (2.83) | 12.65 (2.70) | |||||
| Post | 8.54 (4.81) | 0.78 [0.34, 1.22] b | 8.77 (4.45) | 0.92 [0.59, 1.25] b | 0.05 [- 0.41, 0.51] | -0.49 (.63) | -0.47 [-2.39, 1.44] | |
| Follow-up | 9.62 (3.89) | 0.62 [0.19, 1.05] c | 9.11 (4.69) | 0.84 [0.40, 1.27] c | 0.12 [-0.36, 0.59] | -1.09 (.28) | -1.12 [-3.16, 0.92] | |
| Secondary outcomes | ||||||||
| HADS-A | Pre | 13.22 (4.19) | 12.76 (4.16) | |||||
| Post | 10.37 (4.72) | 0.53 [0.24, 0.82] b | 10.41 (4.74) | 0.39 [0.08, 0.71] b | 0.01 [-0.45, 0.47] | 0.66 (.51) | 0.61 [-1.22, 2.43] | |
| Follow-up | 11.16 (4.6) | 0.4 [0.14, 0.67] c | 10.68 (5.11) | 0.36 [0.03, 0.69] c | 0.1 [-0.38, 0.57] | 0.15 (.88) | 0.14 [-1.78, 2.07] | |
| HDRS | Pre | 16.11 (6.37) | 16.84 (6.55) | |||||
| Post | 7.84 (8.94) | 1.04 [0.63, 1.46] b | 9.12 (7.33) | 1.09 [0.61, 1.58] b | 0.16 [0.23, 0.54] | 0.29 (.77) | 0.55 [-3.22, 4.31] | |
| Follow-up | 4.73 (6.32) | 1.77 [1.18, 2.36] c | 7.65 (7.40) | 1.3 [0.77, 1.82] c | 0.42 [0.04, 0.81] | 1.20 (.23) | 2.19 [-1.39, 5.76] | |
| FIQ | Pre | 70.31 (15.52) | 71.43 (11.57) | |||||
| Post | 61.90 (16.5) | 0.59 [0.26, 0.92] b | 61.95 (14.62) | 0.65 [0.32, 0.99] b | 0 [-0.47, 0.46] | -0.49 (.63) | 0.36 [-5.82, 6.55] | |
| Follow-up | 63.84 (17.66) | 0.5 [0.02, 0.98] c | 62.68 (15.37) | 0.49 [0.09, 0.89] c | 0.07 [-0.41, 0.55] | -1.09 (.28) | -1.35[-9.76, 7.05] | |
Note. SD = Standard Deviation; CI = Confidence Interval; HADS-D = Depression Items of the Hospital Anxiety and Depression Scale; HADS-A = Anxiety Items of the Hospital Anxiety and Depression Scale; HDRS = Hamilton Depression Rating Scale; FIQ = Fibromyalgia Impact Questionnaire.
The results of the per-protocol analysis (n = 69) were similar to those of the intention-to-treat analysis. This showed significant differences in the scores for all outcomes from before to after treatment (HADS-D: β = -3.28, t = -4.59, p < .001; HDRS: β = -2.84, t = -2.09, p = .04, HADS-A: β = -2.37, t = -3.46, p < .001, FIQ: β = -10.61, t = -4.35, p < .001) and from before treatment to follow-up (HADS-D: β = -2.28, t = -2.93, p < .001; HDRS: β = -7.03, t = -5.19, p < .001, HADS-A: β = -1.81, t = -2.51, p = .01, FIQ: β = -8.06, t = -2.52, p = .01). However, no significant differences were found when comparing both treatments (see Table 4).
Descriptive statistics by outcome score at all assessment points, effect sizes with 95% confidence intervals within and between groups, and regression coefficients and 95% CI for the interaction (time x treatment), complete cases.
| Treatment condition | ||||||||
|---|---|---|---|---|---|---|---|---|
| Cognitive Behavioral Therapy | Personal Constructs Therapy | Between group | Coefficients | |||||
| Measure | Time | Mean (SD) a | Hedges’ g [95% CI] | Mean (SD) a | Hedges’ g [95% CI] | Hedges’ g [95% CI] | t (p) | B [95% CI] |
| Primary outcome | ||||||||
| HADS-D | Pre | 11.91 (3.27) | 12.51 (2.86) | |||||
| Post | 8.62 (4.6) | 0.78 [0.34, 1.22] b | 8.74 (4.64) | 0.92 [0.59, 1.25] b | 0.03 [- 0.46, 0.51] | -0.54 (.59) | -0.53 [-2.48, 1.42] | |
| Follow-up | 9.62 (3.89) | 0.62 [0.19, 1.05] c | 9.11 (4.69) | 0.84 [0.4, 1.27] c | 0.12 [-0.36, 0.59] | -1.06 (.29) | -1.12 [-3.23, 0.98] | |
| Secondary outcomes | ||||||||
| HDS-A | Pre | 12.97 (4.05) | 12.43 (4.21) | |||||
| Post | 10.59 (4.56) | 0.53 [0.24, 0.82] b | 10.26 (4.96) | 0.39 [0.08, 0.71] b | 0.07 [-0.41, 0.55] | 0.39 (.70) | 0.37 [-1.50, 2.24] | |
| Follow-up | 11.16 (4.6) | 0.4 [0.14, 0.67] c | 10.68 (5.11) | 0.36 [0.03, 0.69] c | 0.10 [-0.38, 0.57] | 0.06 (.96) | 0.06 [-1.90, 2.01] | |
| HDRS | Pre | 15.16 (5.91) | 15.86 (6.23) | |||||
| Post | 12.31 (8.14) | 1.04 [0.63, 1.46] b | 11.19 (6.6) | 1.09 [0.61, 1.58] b | 0.15 [-0.33, 0.63] | -0.99 (.33) | -1.83 [-5.50, 1.84] | |
| Follow-up | 8.12 (6.41) | 1.77 [1.18, 2.36] c | 10.54 (6.69) | 1.3 [0.77, 1.82] c | 0.36 [-0.12, 0.84] | 0.92 (.36) | -1.71 [-1.95, 5.37] | |
| FIQ | Pre | 71.76 (13.37) | 69.36 (10.59) | |||||
| Post | 60.82 (15.34) | 0.59 [0.26, 0.92] b | 60.76 (14.75) | 0.65 [0.32, 0.99] b | 0.00 [-0.49, 0.68] | 0.68 (.32) | 2.27 [-4.36, 8.89] | |
| Follow-up | 63.84 (17.66) | 0.5 [0.02, 0.98] c | 62.68 (15.37) | 0.49 [0.09, 0.89] c | 0.07 [-0.41, 0.55] | 0.32 (.75) | 1.38 [-7.24, 10] | |
Note. SD = Standard Deviation; CI = Confidence Interval; HADS-D = Depression Items of the Hospital Anxiety and Depression Scale; HADS-A = Anxiety Items of the Hospital Anxiety and Depression Scale; HDRS = Hamilton Depression Rating Scale; FIQ = Fibromyalgia Impact Questionnaire.
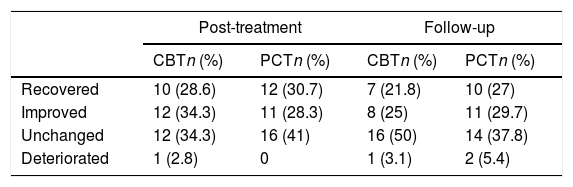
The Jacobson and Truax (1991) criteria were used to analyze changes in HADS-D scores, using a cut-off score of 10.8 to differentiate between the functional and the dysfunctional populations. Each participant was classified as either clinically recovered (significant change and the score moved from dysfunctional to functional population), improved (significant change toward improvement), unchanged (non-significant change), or deteriorated (significant change toward deterioration). The distribution of participants, that completed the posttreatment assessement in these categories was similar after treatment (χ2 (3, n = 74) = 1.59, p = .66, V = 0.15) and at follow-up (χ2 (3, n = 69) = 1.11, p = .77, V = 0.13). See Table 5 for the frequencies and percentages by sample.
Frequencies and percentages of clinically significant change by treatment condition.
Note. CBT = Cognitive Behavioral Therapy; PCT = Personal Construct Therapy.
In relation to the change in fibromyalgia health status, 71 patients completed the FIQ after treatment (CBT = 33; PCT = 38). Overall, 33.3% of the CBT patients and 23.6% of the PCT patients attained an improvement of ≥ 20% in their change scores from before to after treatment, but with no significant differences when comparing conditions (χ2 (2, n = 71) = 3.46, p = .17, V = 0.22). At follow-up, 68 participants completed the FIQ (CBT = 31 and PCT = 37), a change of ≥ 20% from before treatment to follow-up was achieved in 25.8% of the CBT group and 29.72% of the PCT group; again, there were no significant differences between treatment conditions (χ2 (2, n = 68) = 0.31, p = .850, V = 0.06).
We tested change in pain with the 73 patients who completed a VAS after treatment (CBT = 34; PCT = 39). In 23.5% of the CBT group and 15.4% of the PCT group, participants attained reductions of ≥ 30% in their experienced pain, but without significant differences between treatment conditions (χ2 (2, n = 73) = 1.18 p = .55, V = 0.13). At follow-up, 69 participants completed the VAS for pain (CBT = 32; PCT = 37), and 25% of the CBT group compared to 16.2% of the PCT group changed by ≥30% from before treatment to follow-up. Again, no significant differences were found between treatments (χ2 (2, n = 69) = 3.08, p = .21, V = 21).
Finally, 73 participants (CBT = 34; PCT = 39) answered the question about treatment satisfaction. Most were satisfied (96%, n = 70) with how the therapist dealt with the problem they wanted to solve during therapy (quite = 5, very = 23, completely = 42), but without significant differences between treatments (χ2 (5, n = 73) = 3.78, p = .44).
DiscussionThe main aim of this study was to test the efficacy of PCT in the management of depressive symptoms in women with fibromyalgia. Our results show PCT was as effective as CBT in significantly reducing symptoms of depression and anxiety, as well as the impact of the condition in women with fibromyalgia. These results are consistent with those in a clinical sample with depression in which a multicenter randomized controlled trial showed that CBT and a dilemma-focused intervention (based on PCT) had comparable results at three-month and one-year (Feixas et al., 2016, 2018)
Several reasons may explain the lack of significant differences between treatment conditions in the present study. Notably, the exhaustive literature on efficacy equivalence among psychotherapy approaches for depression is telling (Munder et al., 2019; Van Bronswijk et al., 2019), with most psychological interventions appearing to offer comparable efficacy. This invites scope to personalize treatments and consider patient preference (Cuijpers et al., 2021). However, a more nuanced consideration may be that both therapies share a focus on cognitive factors related to pain and psychological suffering. The therapies also both use modular formats that might promote symptom reduction in the same manner by adjusting to the needs of each person, as recommended for this population (Morley et al., 2013). This format also seems to be liked by patients, with most participants in both treatment groups satisfied with their treatment.
Despite pain reduction not being the primary aim of this study, when focusing on pain relief ≥ 30% on the VAS we found that 24 to 15% of the women in our study reported such reduction after treatment, and from 16 to 25% at follow-up. Although greater relief was experienced with CBT, we found no significant differences between the two psychological treatments. Concerning improvement of at least 20% in fibromyalgia -related quality of life (FIQ), similar impact of the fibromyalgia was found in CBT (reductions of 33% after treatment and 26% at follow-up) and PCT (reductions of 26% after treatment and 30% at follow-up). These results are similar to those in a recent review that suggested around 30% of patients achieve a ≥ 30% pain relief and that 44% achieve a quality of life improvement of ≥ 20% after CBT (Bernardy et al., 2018).
Limitations of this study are diverse . We want to highlight the dropout rates, which were 21% (expected) and 13% (lower than expected) from the CBT and PCT groups, respectively, these rates are comparable to those in other studies of CBT for depression (Fernandez et al., 2015). Moreover, another limitation to attain the desired number of participants was the difficulty in detecting fibromyalgia diagnoses at the collaborating centers. This hampered recruitment, forcing us to stop the trial without attaining the expected sample size and to reduce the number of sessions included in the planned adherence analyses (Paz et al., 2020). Thus, it was not possible to attain the expected number of treatment completers (45 by each group). Finally, around 30% of our patients had comorbid chronic fatigue syndrome, which adds to the heterogeneity in our sample features.
In summary, our study supports existing knowledge of the efficacy of the treatments for depressive symptoms in women with fibromyalgia, adding that they can improve pain and the illness' impact on quality of life. A strength of this study is that we provided psychotherapy in the health care centers where patients are usually monitored, increasing the applicability of these findings. Moreover, we recruited patients from different health care centers (primary and mental health), increasing the sociodemographic and clinical diversity. These factors improve the generalizability of our results. Overall, we conclude that PCT should be consider a viable treatment option for assessment in future studies.
FundingThe Ministry of Economy and Competitiveness of Spain supported this work (PSI2014-57957-R).
We want to acknowledge the contribution of all health centres involved in this project and previous pilot study: Nou Barris Nord Mental Health Center and Hospital de Mataró psychiatry service; CAP Guineueta (Institut Català de la Salut), CAP Manso (Institut Català de la Salut), CAP Les Hortes (EAP Poble Sec), CAP Sants (Grup Sant Pere Claver) and primary centers from Badalona Serveis Assistencials (CAP Nova Lloreda, CAP Montgat-Tiana, CAP Montigalà, ABS Martí Julià, ABS Progrès.