Breast cancer causes high levels of anxiety and depression, deteriorating quality of life of patients. Several studies have found that group therapy reduces depression and anxiety also improves the quality of life. The aim of this study is to analyze group therapy effectiveness in emotional state and quality of life in women with breast cancer after finalized medical treatments.
MethodParticipants in this study were 100 adult women diagnosed of breast cancer non-mestastasic and were divided into two types of intervention groups (Self-esteem-Social Skills and Cognitive-Behavioral Therapy). Evaluation instruments were questionnaire Functional Assessment of Breast-cancer Therapy (FACT-B) and Hospital Anxiety and Depression Scale (HADS).
ResultsA statistically significant effect of group therapy in reducing anxiety and depression were observed. Quality of life and emotional well-being significantly improved. These effects remain three months after intervention.
ConclusionsThe results show that the psychological intervention group is efficient to improve emotional state and quality of life of women with breast cancer.
El cáncer de mama provoca niveles altos de ansiedad y depresión, empeorando la calidad de vida (CV) de las pacientes. En numerosos estudios se ha visto que la terapia grupal reduce la depresión y ansiedad además de mejorar la CV. El objetivo de este estudio es analizar la efectividad de la intervención de la terapia grupal en el estado emocional y la CV de mujeres con cáncer de mama localizado al finalizar los tratamientos médicos.
MétodoLa muestra consta de 100 mujeres diagnosticadas de cáncer de mama no metastásico, divididas en dos tipos de grupos de intervención (Autoestima-habilidades sociales y Terapia cognitivo-conductual). Los instrumentos de evaluación fueron el cuestionario Functional Assessment of Cancer Therapy-Breast y la Escala Hospitalaria de Ansiedad y Depresión (HADS).
ResultadosSe observa un efecto estadísticamente significativo de la terapia grupal en la reducción de la ansiedad y la depresión. Las medias de la CV y del bienestar emocional mejoran de manera significativa. Estos efectos se mantienen tres meses después de la intervención.
ConclusionesLos resultados muestran la efectividad de los grupos de terapia para mujeres con cáncer de mama mejorando el estado emocional y la CV.
Breast cancer is one of the oncological diseases in which the effect of this on quality of life (QL) has been most studied. Patients with breast cancer often experience high levels of anxiety and depression, thus worsening their QL (Tang et al., 2017). Several studies with women diagnosed with localized cancer have found high levels of psychiatric morbidity, in particular, anxiety and affective disorders (Gallagher, Parle, & Cairns, 2002; Kissane et al., 1998). In terms of mental distress, the comorbidity rate is between 22 and 43% for breast cancer (Gallagher et al., 2002; Zabora, Brintzenhofeszoc, Curbow, Hooker, & Piantadosi, 2001). There is evidence that patients with primary breast cancer will remain vulnerable to psychological disorders for many years (Antoni et al., 2017; Cohee et al., 2017; Schmidt, Wiskeman, & Steindorf, 2018).
Psychological intervention can facilitate the adaptation of patients to the diagnosis and treatment of breast cancer. Cognitive-behavioral techniques are effective in improving the control of symptoms, the affective state and coping with the disease (Cobeanu & David, 2018; Font & Rodríguez, 2007). This therapy is also effective in reducing levels of anxiety and depression and improving overall QL (Ye et al., 2018). The effects on the QL of cognitive-behavioral therapy tend to be prolonged in the medium and long term and after the intervention is over (McGregor & Antoni, 2009; Stagl, Lechner et al., 2015).
During the last decades it has been shown how cognitive-experiential group therapy is effective in learning to solve problems and cognitive restructuring for negative automatic thoughts (Kissane et al., 2003). Therapy based on relaxation training decreases levels of anxiety and depression during cancer treatment and hospitalization (Gudenkauf et al., 2015; Stagl, Antoni et al., 2015). In addition, cognitive-behavioural group therapy reduces the fear of recurrence, increasing optimism in patients, the feeling of personal growth and greater emotional well-being in surviving women (Antoni et al., 2006; Butow et al., 2013; Stagl, Bouchard et al., 2015). The application of cognitive-behavioral techniques in group therapy, with women survivors of breast cancer, produces a reduction in the levels of anxiety, stress and an improvement of the QL (Bellver, 2007; Syd, 2012). The benefits of group therapy are maintained both in the short term (Fukui et al., 2000) and up to 12 months after the intervention (Phillips et al., 2008). Group interventions have been carried out based on self-esteem and social skills with women with breast cancer, finding an improvement in the QL, due to its relationship with self-esteem (Sehati, Mirqhafourvand, Esfahani, & Amirzehni, 2018). In fact, this type of intervention has also proved very useful in other types of cancer (Barrera et al., 2017).
On the other hand, support-expressive group therapy and positive psychology have been effective in improving the emotional well-being, anxiety and depression of patients with breast cancer (Cerezo, Ortiz-Tallo, & Cardenal, 2009; Classen et al., 2008; Ochoa, Casellas-Grau, Vives, Font, & Borràs, 2017). When comparing cognitive-behavioral group therapy, group therapy expressive support and a therapy resulting from the combination of both, it has been confirmed by scientific evidence that all three are effective (Boutin, 2007).
Psychological group therapy based on psycho-education improves the QL of survivors with breast cancer, producing an increase in emotional well-being and a reduction in anxiety and depression (Matsuda, Yamaoka, Tango, Matsuda, & Nishimoto, 2014; Wu, Chen, Huang, Chang, & Hsu, 2018).
The objective of the present study is to analyse the effectiveness of group therapy intervention in anxiety, depression and QL of women with localized breast cancer at the end of adjuvant medical treatments (chemotherapy/radiotherapy), comparing between two intervention groups: one works self-esteem and social skills (SS) and the other teaches patients cognitive-behavioral techniques (CBT). On the other hand, a series of hypotheses have been formulated:
- a)
It has been shown that group therapy for patients with breast cancer reduces depression, tension, confusion, mood disorders and improves QL. It is predicted that statistically significant differences will be found in the reduction of anxiety and depression means and QL in patients who have received group therapy.
- b)
There are studies that confirm the effectiveness of cognitive-behavioral therapies by reducing levels of depression, and improving optimism, emotional well-being and positive affect (Antoni et al., 2006), as well as reducing levels of depression, anxiety and stress (Syd, 2012). These improvements in the quality of life of the patients are related to the stress management learned during the therapy (Phillips et al., 2008). Therefore, it is expected to find an improvement in the levels of depression, anxiety and emotional well-being in the intervention group based on CBT.
- c)
Phillips et al. (2008) showed that the benefits of group therapy are maintained up to 12 months after the intervention. A maintenance of the positive results of the therapy is predicted at 3 months of follow-up, independently of the intervention group.
The study is part of a quasi-experimental pretest-posttest design, with two intervention groups without the existence of control group (Montero & León, 2007).
ParticipantsThe sample included 100 women with located breast cancer diagnosis. The mean age was 49.47 (SD = 8.42), with an age range between 31-74 years. The percentage of married women was 76%, single women was 7% and the others were separated or widowed. Of the 100 patients surgically treated for breast cancer, 60% received mastectomy (radical surgery) and 40% underwent quadratectomy or tumeractomy (conservative surgery). Regarding the two types of intervention groups, 51 patients were included in the self-esteem and social skills group, while the other 49 were included in the cognitive-behavioral therapy group.
InstrumentsThe instrument used to evaluate the QoL was the Functional Assessment of Cancer Therapy-Breast questionnaire (FACT-B; Brady et al., 1997) designed to measure multidimensional QoL in women with breast cancer. It consists of the FACT-General scale (FACT-G;Cella et al., 1993) plus the specific breast cancer subscales. It is an instrument of easy administration, brief and reliable, with guarantees of validity and sensitivity to change (Brady et al., 1997). It includes five subscales: Physical well-being, Emotional well-being, Functional well-being, Social/family well-being and Other Worries. The internal consistency (Cronbach's alpha coefficient) for the five subscales was from .82 to .89. The General QoL scale had an internal consistency of .86.
The anxiety and the depression were measured with the Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983). It was designed with the intention of developing an instrument for detecting depression and anxiety disorders in the setting of non-psychiatric hospital clinics. It was selected due to his good psychometric properties (Razavi, Delvaux, Farvacques, & Robaye, 1990; Thomas, Glynne, Chait, & Marks, 1997) and great use in studies with breast cancer samples (Watson et al., 1991); several studies confirm the psychometric properties in the Spanish oncology population (López-Roig et al., 2000). The internal consistency (Cronbach's alpha) for the anxiety subscale was .87 and .86 for the depression. The anxiety subscale is focused in its psychic manifestations (tension, nervousness, apprehension, worry, restlessness, anguish). The depression subscale is focused on anhedonia (enjoyment, laughter, happiness, awkwardness, interest in the personal appearance, illusion). Each item refers to symptoms experienced during the previous week. Subscale scores range from 0 (no distress) to 21 (maximum distress).
ProcedureThe participants with breast cancer surgery intervention were included in two types of therapy groups consecutively until they were completed, at the same time as the adjuvant medical treatments (chemotherapy/radiotherapy) were ending. Therefore, a non-random convenience sampling was used for each of the two types of group therapy, with non-control group. The inclusion criteria were: age older than 18 years, surgically operable and with diagnosis of breast cancer in stages I through III of the disease, having completed the adjuvant medical treatments (chemotherapy/radiotherapy), reading and writing levels that would allow them to complete the tests and follow the contents of the group therapy. We excluded patients with evidence of metastases (stage IV), with serious psychopathological disorders (severe mental disorders or dementia).
The two intervention groups consisted of six weekly sessions each one. The frequency of the meetings was weekly and lasted for an hour and a half. One of them was based on the intervention in self-esteem and social skills, with three first sessions in which the concept of self-esteem, self-concept and self-perception that they had of themselves was addressed, working the cognitive distortions related to underestimation. The other three sessions focused on communication, introducing the elements of communication, both verbal and non-verbal. Furthermore, the differentiation of the three communication styles was approached: assertive / passive / aggressive. Assertiveness training was carried out through the representation of roles. The group of cognitive-behavioral techniques consisted of four sessions focused on the learning of cognitive strategies encompassed in Beck's cognitive therapy, self-instruction training, McCaul's distraction techniques, thought stop and stress inoculation training. In the remaining two sessions a behavioral intervention was made, they consisted in relaxation techniques: Jacobson's progressive muscle relaxation, guided imagery and visualization techniques, breathing patterns and planning of pleasurable activities.
The two self-rating Scale were completed by all the women before the start of the group therapy, at six weeks at the end of the group therapy and three months after of the therapy.
The patients were informed of the group therapy and they were agreed to participate in it. At the same time that the informed consent was obtained, the confidentiality in the treatment of the data was explained to them. The study was part of a clinical intervention in the healthcare setting and it was approved by the hospital ethics committee.
Statistical analysisIn this study, Mixed ANOVA model for repeated measures have been chosen because the temporary measurements are balanced and no type of loss has occurred in relation to the subjects in the three measurement moments. One of the assumptions of this model corresponds to the sphericity. Regarding the size of the effect, the indicator that has been used in this study is the partial η2. The values that have been considered in the effect size are: 0.01-0.059 small, 0.06-0.139 medium, and ≥ 0.14 large. The data analysed have been carried out through the SPSS 22.0 program.
ResultsFirst, we were analysed the differences between the two intervention groups in the different variables depending on each type of group therapy. Secondly, the evolution of the different dependent variables in the three measuring moments was studied, independently of the therapy group. Finally, we analysed the evolution of these variables in the three measurement moments considering the two intervention groups.
Also we considered the differences between the intervention groups in the several variables depending on the type of therapy group.
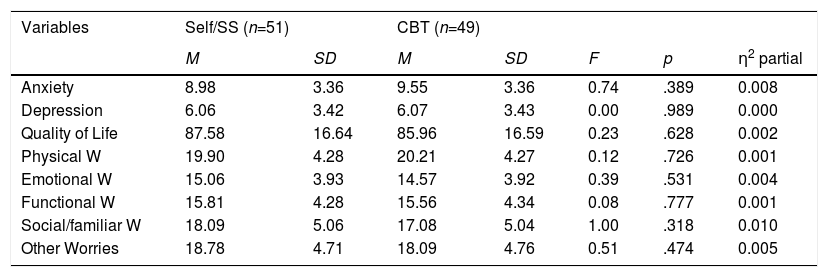
From the statistical analysis, no statistically significant differences were found in the means of the eight dependent variables analysed (see Table 1): depression [F (2, 99)=0.00; p=.989], anxiety [F (2, 99)=0.74; p=.389], social/familiar well-being [F (2, 99)= 1.00; p =.318], emotional well-being [F (2, 99)=0.39; p=.531], QoL [F (2, 99)=0.62; p=.628], functional well-being [F (2, 99)=0.08; p=.777], physic well-being [F (2, 99)= 0.12; p=.726] and other worries [F (2, 99)= 0.51; p=.474].
Differences between the two intervention groups in the different variables depending on the type of psychological treatment.
| Variables | Self/SS (n=51) | CBT (n=49) | |||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | F | p | η2 partial | |
| Anxiety | 8.98 | 3.36 | 9.55 | 3.36 | 0.74 | .389 | 0.008 |
| Depression | 6.06 | 3.42 | 6.07 | 3.43 | 0.00 | .989 | 0.000 |
| Quality of Life | 87.58 | 16.64 | 85.96 | 16.59 | 0.23 | .628 | 0.002 |
| Physical W | 19.90 | 4.28 | 20.21 | 4.27 | 0.12 | .726 | 0.001 |
| Emotional W | 15.06 | 3.93 | 14.57 | 3.92 | 0.39 | .531 | 0.004 |
| Functional W | 15.81 | 4.28 | 15.56 | 4.34 | 0.08 | .777 | 0.001 |
| Social/familiar W | 18.09 | 5.06 | 17.08 | 5.04 | 1.00 | .318 | 0.010 |
| Other Worries | 18.78 | 4.71 | 18.09 | 4.76 | 0.51 | .474 | 0.005 |
Note. Self/SS= Intervention in Self-esteem and Social Skills, CBT= Intervention Group in Cognitive-Behavioral Therapy.
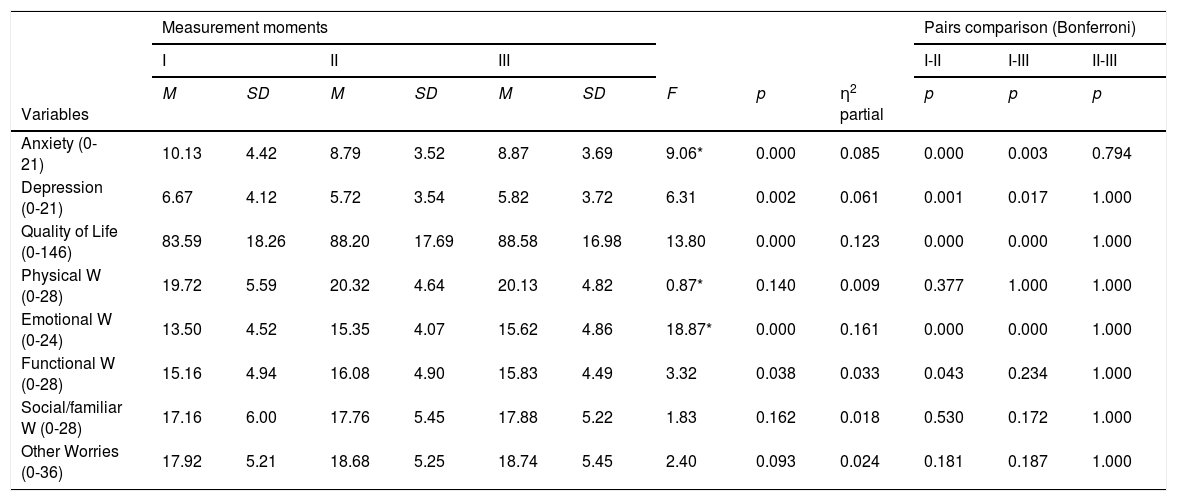
A statistically significant evolution was observed in five of the eight variables (see Table 2). In emotional well-being there was a significant increase in the means between the different moments of measurement with a large effect size [F (1.67, 99) = 18.84; p = .000; partial η2 = 0.161], showing differences between moment I and II, and moment I and III. Regarding the group of variables with a medium effect size, we found anxiety, depression and QoL. In anxiety, statistically significant differences were observed in the different measurement moments [F (1.82, 99) = 9.06; p = .000; partial η2 = 0.085], observing a greater difference between moments I and II, and I and III. The means of the variable anxiety had been decreasing throughout the intervention. Another variable with a medium effect size is the QoL, in which statistically significant differences were observed in terms of the different measurement moments [F (2, 99) = 13.80; p = .000; partial η2 = 0.123]; his score improved significantly between the moment I and II, there was almost no difference between moments II and III. And, finally, in depression significant differences were observed [F (2, 99) = 6.31; p = .002; partial η2= 0.061], whose means throughout the intervention had decreased, being significant the differences between I and II, and I and III. Among the variables that present a small effect size was functional well-being [F (2, 99) = 3.32; p = .038; partial η2 = 0.033]; the mean of this variable had increased between I and II, but decreases in III.
Evolution of the different variables in the three measurement moments.
| Measurement moments | Pairs comparison (Bonferroni) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | I-II | I-III | II-III | |||||||
| Variables | M | SD | M | SD | M | SD | F | p | η2 partial | p | p | p |
| Anxiety (0-21) | 10.13 | 4.42 | 8.79 | 3.52 | 8.87 | 3.69 | 9.06* | 0.000 | 0.085 | 0.000 | 0.003 | 0.794 |
| Depression (0-21) | 6.67 | 4.12 | 5.72 | 3.54 | 5.82 | 3.72 | 6.31 | 0.002 | 0.061 | 0.001 | 0.017 | 1.000 |
| Quality of Life (0-146) | 83.59 | 18.26 | 88.20 | 17.69 | 88.58 | 16.98 | 13.80 | 0.000 | 0.123 | 0.000 | 0.000 | 1.000 |
| Physical W (0-28) | 19.72 | 5.59 | 20.32 | 4.64 | 20.13 | 4.82 | 0.87* | 0.140 | 0.009 | 0.377 | 1.000 | 1.000 |
| Emotional W (0-24) | 13.50 | 4.52 | 15.35 | 4.07 | 15.62 | 4.86 | 18.87* | 0.000 | 0.161 | 0.000 | 0.000 | 1.000 |
| Functional W (0-28) | 15.16 | 4.94 | 16.08 | 4.90 | 15.83 | 4.49 | 3.32 | 0.038 | 0.033 | 0.043 | 0.234 | 1.000 |
| Social/familiar W (0-28) | 17.16 | 6.00 | 17.76 | 5.45 | 17.88 | 5.22 | 1.83 | 0.162 | 0.018 | 0.530 | 0.172 | 1.000 |
| Other Worries (0-36) | 17.92 | 5.21 | 18.68 | 5.25 | 18.74 | 5.45 | 2.40 | 0.093 | 0.024 | 0.181 | 0.187 | 1.000 |
Note. * Huynh-Fel. Test.
No statistically significant differences were found between the different measurement moments in physical well-being [F (1.88, 99) = 0.875; p = .140; partial η2 = 0.009], social/family well-being [F (2, 99) = 1.83; p = .162; partial η2 = 0.018] and other worries [F (2, 99) = 2.40; p = .093; partial η2 = 0.024].
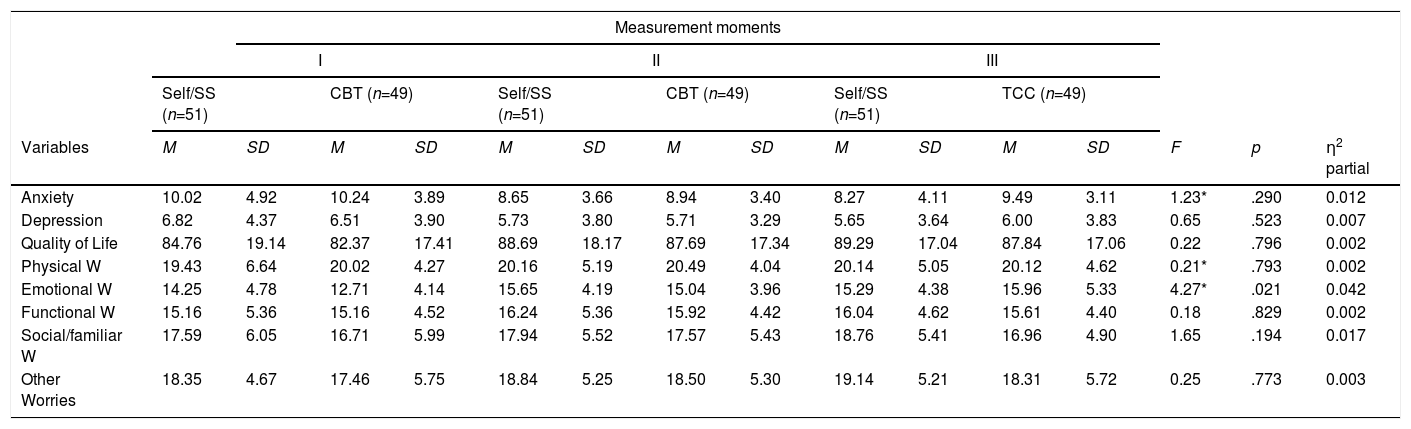
Evolution of the different variables in the three moments of evaluation depending on the type of group therapyFinally, the interaction between the time evolution in the three measurement moments and the two therapy groups (Self-esteem and SS group, and CBT group) in the different variables is presented. The only variable in which statistically significant differences were found with a small effect size (partial η2 = 0.042) was in emotional well-being [F (1.67, 99) = 4.27; p = .021]. See Table 3. The evolution of this variable was that patients who received intervention based on cognitive-behavioral therapy tended to increase their emotional well-being. This difference between the two intervention groups was observed throughout the intervention process and at the three-month follow-up. Patients who belonged to the intervention group focused on self-esteem and social skills also showed an increase in emotional well-being, although this improvement was not statistically significant.
Evolution of the different variables in the three evaluation moments according to the type of treatment.
| Measurement moments | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | |||||||||||||
| Self/SS (n=51) | CBT (n=49) | Self/SS (n=51) | CBT (n=49) | Self/SS (n=51) | TCC (n=49) | ||||||||||
| Variables | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | F | p | η2 partial |
| Anxiety | 10.02 | 4.92 | 10.24 | 3.89 | 8.65 | 3.66 | 8.94 | 3.40 | 8.27 | 4.11 | 9.49 | 3.11 | 1.23* | .290 | 0.012 |
| Depression | 6.82 | 4.37 | 6.51 | 3.90 | 5.73 | 3.80 | 5.71 | 3.29 | 5.65 | 3.64 | 6.00 | 3.83 | 0.65 | .523 | 0.007 |
| Quality of Life | 84.76 | 19.14 | 82.37 | 17.41 | 88.69 | 18.17 | 87.69 | 17.34 | 89.29 | 17.04 | 87.84 | 17.06 | 0.22 | .796 | 0.002 |
| Physical W | 19.43 | 6.64 | 20.02 | 4.27 | 20.16 | 5.19 | 20.49 | 4.04 | 20.14 | 5.05 | 20.12 | 4.62 | 0.21* | .793 | 0.002 |
| Emotional W | 14.25 | 4.78 | 12.71 | 4.14 | 15.65 | 4.19 | 15.04 | 3.96 | 15.29 | 4.38 | 15.96 | 5.33 | 4.27* | .021 | 0.042 |
| Functional W | 15.16 | 5.36 | 15.16 | 4.52 | 16.24 | 5.36 | 15.92 | 4.42 | 16.04 | 4.62 | 15.61 | 4.40 | 0.18 | .829 | 0.002 |
| Social/familiar W | 17.59 | 6.05 | 16.71 | 5.99 | 17.94 | 5.52 | 17.57 | 5.43 | 18.76 | 5.41 | 16.96 | 4.90 | 1.65 | .194 | 0.017 |
| Other Worries | 18.35 | 4.67 | 17.46 | 5.75 | 18.84 | 5.25 | 18.50 | 5.30 | 19.14 | 5.21 | 18.31 | 5.72 | 0.25 | .773 | 0.003 |
Note. Self/SS= Intervention in Self-esteem and Social Skills, CBT= Intervention Group in Cognitive-Behavioral Therapy; I (pre), II (post) III (3 months follow-up); * Huynh-Felt Test.
Concerning the other variables, there were no statistically significant differences between the different measurement moments and the two intervention groups: anxiety [F (1.82, 99) = 1.23; p = .290; partial η2 = 0.012], depression [F (2, 99) = 651; p = .523; partial η2 = .007], QoL [F (2, 99) = 0.22; p = .796; partial η2 = 0.002], physical well-being [F (1.88, 99) = 0.21; p = .793; partial η2 = 0.002], functional well-being [F (2, 99) = 0.18; p = .829; partial η2 = 0.002], social/family well-being [F (2, 99) = 1.65; p = .194;partial η2 = 0.017] and other worries [F (2, 99) = 0.258; p = .773; partial η2 = 0.003].
Discussion and ConclusionsThis study aimed to analyse the effectiveness of group therapy intervention in the emotional state and QL of women with localized breast cancer at the end of the adjuvant medical treatments (chemotherapy / radiotherapy), as well as knowing if this effectiveness is the same in two types of psychological intervention group and if it is maintained both at the end of the intervention and in the follow-up after three months.
In relation to the results obtained, it can be affirmed that both intervention groups are associated with significant benefits, improving the QL and mood of women with breast cancer. This improvement in the reduction of anxiety and depression levels throughout the follow-up is significant, being somewhat greater in anxiety than in depression. As we indicated in our first hypothesis, we can conclude that both anxiety and depression have been reduced after finishing the group treatment. This confirms the results obtained in other studies with group therapy with women with localized breast cancer (Bellver, 2007; Taylor et al., 2003).
The proposed hypothesis describes that it is expected to find an improvement in the levels of depression, anxiety and QL in the intervention group based on CBT than in the self-esteem and SS group. Regarding the comparison between the two intervention groups, the results indicate that no significant differences have been found in the symptoms of anxiety and depression and in QL, so it can be inferred that both the intervention in self-esteem and SS and the intervention. Based on CBT are equally effective for the reduction of anxiety and depression and for the increase of the QL in patients surviving breast cancer. One of the reasons for this improvement in the QL in the intervention group based on self-esteem and SS is because it is closely related to self-esteem (Sehati et al., 2018). In fact, this type of intervention has also proved very useful in other types of cancer (Barrera et al., 2017). However, there does seem to be significant differences between the two intervention groups in emotional well-being throughout the follow-up. Patients who received treatment based on CBT tend to increase their emotional well-being with respect to the self-esteem group and SS. This difference between the two intervention groups is observed throughout the group intervention process and at the three-month follow-up. Therefore, we can partially confirm the second hypothesis, since there is an improvement in the emotional well-being dimension, but not in the rest of the variables. It is considered that CBT is the most effective technique in localized breast cancer, both in group interventions and in individual interventions (Boutin, 2007; Jassim, Whitford, Hickey, & Carter, 2015).
This benefit is maintained after three months in the variables anxiety, depression, QL and emotional and functional well-being. In relation to the symptoms of anxiety and depression, a greater difference can be observed between the beginning of the therapy and the three months of follow-up. The benefit provided by the two types of group intervention for these symptoms is maintained after three months at the end of therapy. Other studies have obtained benefits that tend to be prolonged in the medium term once the intervention is finished (McGregor et al., 2009). In terms of emotional and functional well-being, it also improves the group intervention process. After three months of follow-up, it is observed that the improvement in this variable is maintained. This is relevant since it indicates that the learning of the CBT and self-esteem and SS are maintained over time and that they continue to be put into practice in the daily life of the patients. However, in the rest of the areas of the QL group psychological therapy does not seem to have influenced significantly, confirming the third hypothesis rose where maintenance of the positive results of the therapy was expected after three months of follow-up, regardless of the group of intervention.
Psychotherapy groups have the advantage of being more beneficial if they are discussed in terms of cost-effectiveness than individual therapy, since it involves serving a larger number of patients. This generates a network of support with the group of equals (Spiegel, 1994).
The limitations of the study are that there is no control group with which to compare both types of group therapy used in this study; having a control group can pose ethical problems because you can not benefit from group therapy. However, a control group would be necessary to carry out a purely experimental study, in addition to forming the intervention groups with adequate randomization. Another limitation is that there is only a follow-up after three months of the group intervention, with what we believe is necessary in future studies to follow up in the long term.
Different studies have delved into the benefits that other less conventional or novel therapies can bring. It has been shown that hypnosis-based psychotherapy and CBT is beneficial, as it teaches patients in treatment and survivors to reduce fatigue, cancer-related pain and control sleep disturbances (Gregoire et al., 2017; Mendoza et al., 2016; Téllez et al., 2017). On the other hand, mindfulness based on stress reduction has been found to be effective in promoting QL for both patients (Haller et al., 2017; Johns et al., 2015; Sarenmalm, Martensson, Andersson, Karlsson, & Bergh, 2017; Lengacher et al., 2016; Park et al., 2018; Rosen, Paniagua, Kazanis, Jones, & Potter, 2018) and survivors (Gonzalez-Hernandez et al., 2018; Lengacher et al., 2016). Psychodynamic psychotherapy has resulted in a short-term improvement in patients’ depressive symptoms (Beutel et al., 2014). Finally, interventions based on physical activity promote an improvement of health in cancer survivors (Maxwell-Smith et al., 2018).