Ageism and loneliness are two relevant public health phenomena because of their negative impact on the senior's mental health. With the increase in average life expectancy, these tend to co-occur, which may increase the psychological distress (PD) of seniors. Resilience has been shown to be an important protective factor of seniors mental health, although its potential buffering role of public health risk factors with cumulative impact on mental health, such as loneliness and ageism, needs to be more studied.
AimTo assess the potential mediator role of resilience between the effects of ageism and loneliness on PD in seniors.
MethodsA sample of 349 Portuguese seniors aged 60 years and over was collected through an online survey and during the COVID-19 pandemic period. Seniors completed the Kessler Psychological Distress Scale (K6), the Short-Form of UCLA Loneliness Scale (USL-6), the Ambivalent Ageism Scale (AAS) and the Connor-Davidson Resilience Scale (CD-RISC-10). A mediation analysis model was developed with resilience as a mediating variable.
ResultsThere were moderate to high levels of PD and moderate levels of ageism, loneliness and resilience. Resilience fully mediated the effect of ageism on PD and partially mediated the effect of loneliness on PD.
ConclusionsResilience was an important protective factor of mental health against the effects of ageism, and partially protected mental health from the effects of loneliness among seniors. It is suggested that resilience be considered as a factor to be integrated in future intervention programs for mental health. The practical applicability of this study is discussed.
The world population is aging due to low birth rates and increasing life expectancy (WHO, 2015). By 2050, the world's population aged 60 and over is expected to double to nearly two billion (22% of the world's population; Officer et al., 2016; WHO, 2015). These demographic changes highlight the need to promote health and well-being in older populations, contributing to as independent, comfortable and healthy aging as possible (von Humboldt & Leal, 2014; WHO, 2015). However, the levels of health are not aligned with the increase in longevity, and the latest global report on aging and health highlights great health inequities and difficulties among the senior population, particularly regarding mental health (Officer et al., 2016; WHO, 2015). In this sense, in recent decades the influence of psychosocial components on seniors' mental health has received increasing attention (Donovan & Blazer, 2020). The quantity and quality of human relationships and the importance of social relationships became so important that they became the main focus of research on the social determinants of mental health (Donovan & Blazer, 2020). Thus, within this extensive line of investigation, two constructs stand out as potential major public health pandemics worldwide among seniors as having a great negative impact on their mental health: loneliness and ageism (Donovan & Blazer, 2020; Holt-Lunstad, 2021; Officer et al., 2016).
The prevalence of loneliness has increased significantly across different generations in recent decades (Hawkley et al., 2019; Suanet & Tilburg, 2019). Among the senior population in particular, studies from several countries indicate that between 19% and 30% of people aged 60 years report feeling loneliness (Fakoya et al., 2020; Landeiro et al., 2017; Mehrabi & Béland, 2020; Ong et al., 2015; Yang & Victor, 2011). Meta-analyses have recently found that loneliness increases the risk of dementia by 50%, the risk of stroke by 30%, and the risk of overall mortality by 26% (Cacioppo et al., 2011; Donovan & Blazer, 2020; Holt-Lunstad et al., 2015; Valtorta et al., 2016). Further, loneliness has been very associated to various mental health conditions, such as depressive and anxiety symptomatology, and lower quality of life (Cacioppo et al., 2014; Landeiro et al., 2017; Malcolm et al., 2019). In addition, ageism is increasingly being recognized as a major threat to the well-being of seniors (Marques et al., 2020). World Health Organization data from more than 83,000 people in 57 countries indicate that 60% of general population respondents refers that seniors do not receive the respect they deserve (Marques et al., 2020; Officer et al., 2016). Further, current evidence showed that ageism increases the risk of mortality, slower recovery from illness, and mental health problems (Burnes et al., 2019; Levy, 2003). In fact, a recent systematic review evaluated the effects of ageism in 11 health dimensions from 45 countries, and with empirical evidence of 25 years, and found that in 95.5% of the studies ageism led to negative mental health outcomes (Chang et al., 2020). Particularly, ageism was significantly associated to lifetime depression, anxiety, suicidal ideation, and posttraumatic stress.
Loneliness and ageism, despite being independent factors, are generally associated among seniors (Shiovitz-Ezra et al., 2018). Contemporary studies establish three major relationships between them: the internalization of stereotypes of aging such as old age being a time of loneliness, the age-based discriminatory practices that increase the isolation and feeling of loneliness, and the chronic rejection that can cause social avoidance and vice-versa (Shiovitz-Ezra et al., 2018; von Humboldt et al., 2020). These factors enhance the occurrence of cumulative risk factors, potentially creating even more negative effects on the mental health of seniors (Burnes et al., 2019; Shiovitz-Ezra et al., 2018). Despite this evidence, little research has been done to assess the mental health effects of loneliness and ageism together, even though there are already effective and internationally tested instruments, particularly in indicators of mental health, through variables such as psychological distress (PD; Yiengprugsawan et al., 2014).
Despite being two adverse phenomena, loneliness and ageism are expected to increase in the coming decades due to the population aging trend and the absence of policies to address these problems efficiently (Burnes et al., 2019; Marques et al., 2020). Some external protective factors for loneliness and ageism have already been identified, namely social support (see, for example, a recent systematic review by Wang et al., 2018). However, there is very few research that seeks to understand the protective role of internal factors which, combined with social support and other external protective factors, may qualitatively change the way in which interventions against loneliness and ageism are carried out (Holt-Lunstad, 2021; Hu et al., 2020). In line with this evidence, the interest and relevance of protective variables such as resilience have increased significantly in recent years (Górska et al., 2021).
Resilience is the ability to find resources to act, manage, adapt, and recover in the face of and after adverse situations (Madsen et al., 2019). Current systematic reviews and meta-analyses present resilience as a modifiable factor with great protective potential for the general health of seniors, and particularly for their mental health (Ávila et al., 2016; Färber & Rosendahl, 2020). Resilience has been shown to be a protective factor against substance use (Van Gils et al., 2021), anxiety, depression, stress, post-traumatic stress symptoms, and other mental illnesses (Färber & Rosendahl, 2020); it also enhances general satisfaction with life and well-being (Färber & Rosendahl, 2020), happiness, hope, self-esteem, social support, longevity, and quality of life (Gallardo-Peralta et al., 2020; Lai et al., 2021; MacLeod et al., 2016). Further, resilience has shown positive results in the face of PD, which is one of the main indicators of mental health evaluated internationally (Kessler et al., 2002). PD is a state of suffering characterized by symptoms of anxiety, depression, and stress (Kessler et al., 2002; Santos et al., 2015). Studies have shown that resilience has strong negative associations with PD (Keyes et al., 2014; Upenieks, 2021). Among seniors, PD seems to be associated with several negative factors, namely, the occurrence of vulnerabilities (e.g., greater probability of physical dependence, limitation of freedoms and functional capacity, management of chronic diseases and comorbidities), worse socioeconomic conditions, poor psychosocial conditions, and weak social and family support network (Evandrou et al., 2017; Santos et al., 2015; Sterina et al., 2021). Nevertheless, an important research gap on the relationship between resilience and PD in senior populations remains (Antelo et al., 2021; Górska et al., 2021). Further, the COVID-19 period may become a particularly interesting context to assess the moderating role of resilience between loneliness and ageism and mental health indicators as, during the pandemic, seniors may have been exposed to greater levels of social isolation and loneliness (von Humboldt et al., 2022; Wu, 2020). Also, in the pandemic, seniors were one of the populations “labeled” as at-risk populations, quickly becoming severely restricted in their routines, in their social networks and in their well-being (Kornadt et al., 2021; Lebrasseur et al., 2021).
Scientific evidence has shown that resilience is a decisive resource to the mental health of seniors. Resilience has had an important positive role on the mental health of seniors in adverse situations, as in context of disasters (Timalsina & Songwathana, 2020), pandemics (Sterina et al., 2021), and long chronic illness (Johnson et al., 2019). Further, the lifelong development process may bring with it a serious of adverse events, including exposure to highly stressful events (e.g., death of a family member and other loved ones), chronic diseases, and reduced functional capacity (Tomás et al., 2018; Lekalakala-Mokgele, 2018). Thus, resilience in seniors is associated with emotional regulation in the face of adversity, which allows greater ability to resort to social support, a sense of self-efficacy, use of proactive coping strategies, ability to adapt to stressful events, greater adaptation of the immune system, and greater satisfaction with life (Fontes & Neri, 2015; Southwick et al., 2014). Moreover, seniors constitute an ideal population to understand the resilience process, as they have been potentially exposed to a greater amount of stressful states accumulated in adversity experiences throughout their lifecycle (Serrano-Parra et al., 2013). Based on this evidence, the main objective of this study is to examine the potential mediator role of resilience between the effects of ageism and loneliness on the PD of seniors.
MethodParticipantsA non-probabilistic convenience sample of 349 seniors was collected. Inclusion criteria for this study were as follows: (1) being community-dwelling seniors; and (2) being at least 60 years of age. Participants’ ages ranged from 60 and 87 years old (M = 68.09; SD = 5.91), and just over half of them (57.3%) were men. The vast majority of participants reported having children (92.6%) and grandchildren (78.2%), just over a third (39.8%) lived with a partner and just under a third (30.4%) lived alone. Just over half of the participants lived in urban areas (53.3%) and were married/in a civil partnership (57.3%). In addition, most had at least a high school diploma (35.5%), 48.4% were retired, 41.4% were employed, and 48.7% had an annual income of up to two national minimum wage (see Table 1). All participants self-identified as heterosexual cisgender.
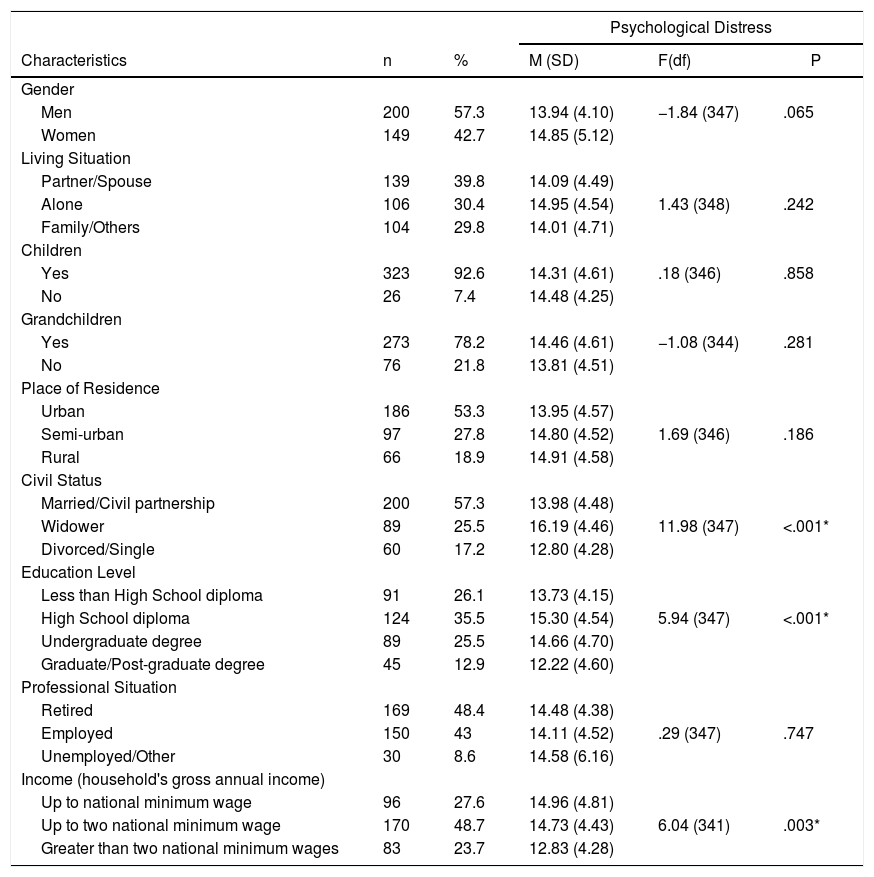
Sociodemographic characteristics by psychological distress.
Note: All analyzes were performed using ANOVAs, and Bonferroni correction was used when the results were significant; * Highlights significant statistical differences.
The online survey consisted of a sociodemographic questionnaire and four standardized scales measuring PD, loneliness, ageism, and resilience in seniors. All measures were administered in Portuguese.
Sociodemographic questionnaireParticipants were asked about their age, gender, sexual orientation, living situation, having children and grandchildren, place of residence, civil status, education level, professional situation, and income. Age was measured as continuous variable and gender and sexual orientation were presented as open-ended questions, and categorized aposteriori. Having children and having grandchildren were measured in a dichotomic format (yes or no). The remaining variables were measured using ordinal scales with different response options (Table 1).
Psychological distress (PD)PD was measured using the Kessler Psychological Distress Scale (K6; Kessler et al., 2002), adapted to Portuguese population (Pereira et al., 2019). The K6 measures the degree of nonspecific PD, one of the main indicators of mental health. It is composed of six items in a unidimensional scale (e.g., Item 5 – “During the past 4 weeks, how often did you feel like everything was an effort?”) measured in a 5-point Likert scale (from 0 - none of the time to 4 - all of the time). Cronbach's alpha for this study was high (α = .83). Higher scores reflect higher levels of PD.
LonelinessLoneliness was measured using the Short-Form of UCLA Loneliness Scale (USL-6; Russell, 1996), adapted to the Portuguese context (Neto, 2014). The USL-6 measures feelings of loneliness in a unidimensional scale. It is composed of six items (e.g., Item 3 – “I feel left out”), measured in a 4-point Likert type scale (from 1 - never to 4 - frequently). Cronbach's alpha for this study was high (α = .85). Higher scores reflect higher levels of loneliness.
AgeismAgeism was measured using the Ambivalent Ageism Scale (AAS; Cary et al., 2016), adapted to the Portuguese context (Barroso, 2018). The AAS measures age-related discrimination in a two-dimensional structure, a subscale of benevolent ageism (e.g., item 6 – “Older people need to be protected from the harsh realities of society”) and a subscale of hostile ageism (e.g., item 13 – “Old people are a drain on the health care system and the economy”). The AAS is composed by 13 items, measured in a 7-point Likert type scale (from 1 - Strongly Disagree to 7 - Strongly Agree). Cronbach's alpha for this study was high (α = .86). Higher scores reflect higher levels of ageism.
ResilienceResilience was measured using the Connor-Davidson Resilience Scale (CD-RISC-10; Campbell-Sills & Stein, 2007), adapted to the Portuguese context (Almeida et al., 2020). The CD-RISC-10 measures resilience in a unidimensional scale. It is composed of ten items (e.g., Item 8 – “I am not easily discouraged by failure”), measured in a 5-point Likert type scale (from 0 - not true at all to 4 - true nearly all of the time). Cronbach's alpha for this study was high (α = .85). Higher scores reflect higher levels of resilience.
ProceduresThis study was part of a larger project called Pro-PSISexES, presented as a study aimed at assessing health and well-being among seniors in Portugal. A convenience and intentional sampling procedure was used, and participants were recruited across the country. Data were collected between May 2020 and July 2021 through an online survey available on Qualtrics plataform. Although the data collection was pursued during the two lockdowns in Portugal, the collection rate decreased during these times (7.6% of data was collected during lockdowns). Firstly, the survey was advertised through different electronic means, namely, through online social network groups (e.g., facebook groups), blogs, and websites of interest to seniors. The dissemination of the study was also requested in two senior universities. The invitation to potential participants included a brief description of the study and a link to the online survey. The first page of the online survey included an informed consent, which all participants were asked to accept before completing the survey. All procedures were in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards, and the research project was approved by the Ethics Committee of [Institutional name] (D/028/04/2020). No compensation was offered to participants.
Data analysisThe data underwent three types of statistical analysis: descriptive statistics, including percentage analysis of sociodemographic variables, measures of central tendency and dispersion and bivariate correlations between the main variables; univariate inference statistical analyses, ANOVAs; and Structural Equation Models (SEM). Missing values were treated using the average imputation method when the missing data represented less than 15%, and only for continuous variables. SPSS Statistics (v. 27, SPSS an IBM company, Chicago, IL) was used to carry out the descriptive and inference statistics. Analysis of Moment Structures (v. 27, AMOS an IBM company, Chicago, IL) was used to carry out the SEM. A mediation model was developed to assess the impact of loneliness and ageism on PD, and the mediating effect of resilience. Model fit was assessed using the Chi-Square test, the Comparative Fit Index (CFI; Bentler, 1990), the Goodness of Fit Index (GFI; Joreskog & Sorbom,1996), and the Root Mean Square Error of Approximation (RMSEA; Steiger, 1990). Values above .90 on the CFI and GFI and below .10 on the RMSEA were indicators of an acceptable model fit; and values above .95 on the CFI and GFI and below .05 on the RMSEA were indicators of good model fit (Hair et al., 2006). The magnitude and significance of the mediated and direct effects were estimated using bootstrap procedures generated from 1000 samples, as recommended for mediation analysis (Preacher & Hayes, 2008). All variables were introduced as observed variables, and an alpha level of 0.05 was used to determine statistical significance.
ResultsIndividual differences on psychological distressAnalyzes were carried out in order to assess whether sociodemographic characteristics would significantly affect the levels of PD (Table 1). It was found that widowed seniors had significantly more PD than married/in a civil partnership (p <.001) or divorced/single individuals (p <.001). Further seniors with higher education levels (Graduate/Post-graduate) had significantly less PD than seniors with lower education levels [High School (p <.001) or Undergraduate (p <.05)], but had no significant differences in distress when compared to the group with lowest education (less than high school diploma - p <.257). Moreover, seniors with higher annual incomes (greater than two national minimum wages) had significantly lower levels of PD than seniors with lower incomes (p <.05).
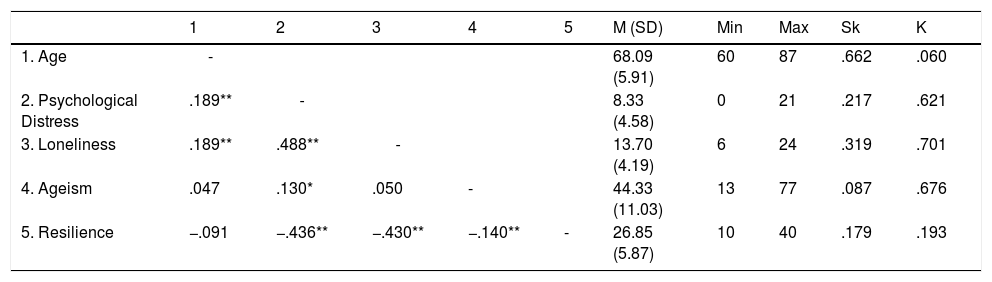
Descriptive analysis and levels of PDIn order to evaluate the relationships between the variables under study, bivariate Pearson correlations were performed for the following variables: PD, age, loneliness, ageism, and resilience. As shown in Table 2, PD was significatively correlated with all other variables. Further, resilience had significant negative correlations with ageism and loneliness. Loneliness was significantly and positively associated with age.
Means, standard deviations and Pearson's correlation among the variables under study.
Note: Benevolent Ageism Subscale - M = 23.59, SD = 7.23; Hostile Ageism Subscale - M = 20.74, SD = 6.31; * p < .05; ** p < .01.
In the absence of Portuguese cutoff scores, considering the cutoff scores proposed by Kessler and Prochaska (Kessler et al.,2002; Prochaska et al., 2012) we found moderate to high levels of PD in our sample; Specifically, 23.2% of the sample showed low levels, 58,2% showed moderate levels, and 18,6% showed severe levels of PD (Prochaska et al., 2012). Based on previous studies in the Portuguese senior population, there were also moderate levels of loneliness (Neto, 2014) and ageism (Barroso, 2018), as well as moderate levels of resilience (Almeida et al., 2020).
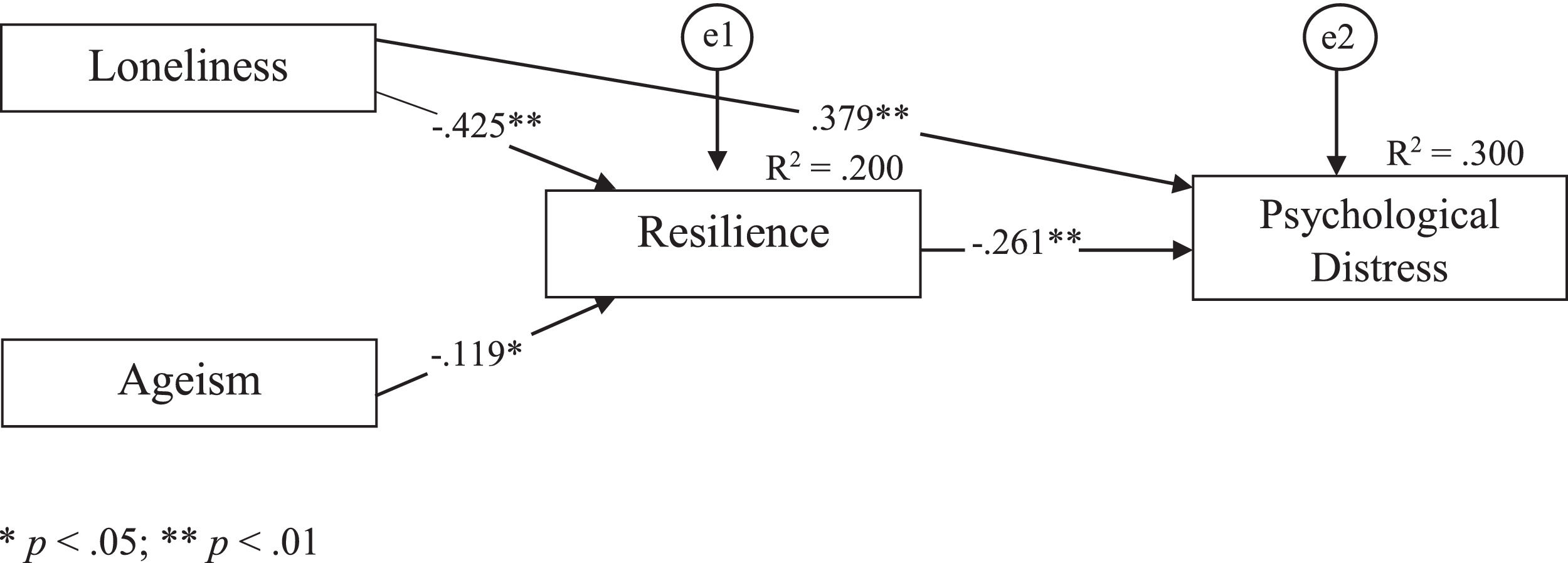
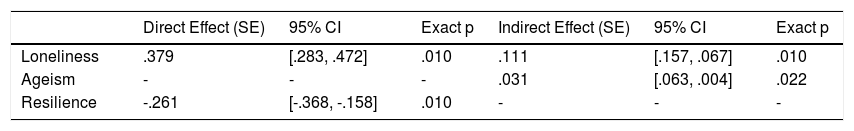
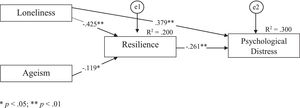
Mediation analysisA mediation model was developed in order to assess the effects of loneliness and ageism on PD, and the mediating role of resilience between the effects of loneliness and ageism on PD. The initial model included both direct and indirect effects. Ageism had no significant direct effect on PD. This trajectory was thus constrained to zero. This model showed an excellent fit to the data χ2 (2) = 3.576, p = .167, CFI = .992, GFI = .995, RMSEA = .048 90% CI [.000, .126] (Figure 1). No evidence of violations to the normal distribution was found (Kline, 2010).
Loneliness and ageism were significantly associated with PD, although these effects were partially and fully mediated by resilience, respectively (Table 3). These results partially confirm our main assumption that resilience has a buffering effect factor between the impact of loneliness and ageism on seniors' mental health.
DiscussionThe main objective of this study was to evaluate the potential mediator role of resilience between the effects of ageism and loneliness on PD among Portuguese seniors. Additionally, the levels of PD in this senior sample was also examined, according to individual differences, and the intensity of the relationship between these variables.
It was found that widowed seniors had higher levels of PD than seniors with other marital status. This evidence is in line with previous research, systematic reviews, and meta-analyses (e.g., Kristiansen et al., 2019), which have highlighted the strong relationship between widowhood and lower levels of mental health, particularly in the manifestation of anxious and depressive symptoms. Widowhood is a phenomenon closely associated with loneliness and lack of social support, as well as dysfunctional coping and avoidance strategies, which also contributes to worse levels of mental health (Boora & Jain, 2020; Carr, 2018). In contrast, seniors with higher educational levels and incomes had lower levels of PD than other seniors. Several studies support this finding (Bakkeli, 2019; Sperandei et al., 2021). Whereas low levels of income and education are associated with poorer lifestyles and worse levels of mental health and well-being, good economic and educational conditions in seniors are associated with more and better access to resources (e.g., social, care, quality of life) and more favorable conditions to solve inconveniences or needs associated with aging, which, in turn, contribute to better health in general, particularly mental health (Gildner et al., 2016; Sperandei et al., 2021; Wippold et al., 2020).
Regarding the overall levels of psychological distress, moderate to high levels of PD were found in this study. Studies from several countries that measured PD in seniors using the Kessler scale (K-6; e.g., Kikuchi et al., 2013; Prochaska et al., 2012; Won & Hae, 2015) showed that significant levels of PD in senior population is prevalent. However, our findings showed particularly high levels of PD, which we argue that, at least to some extent, this may be due to the fact that the data collection was carried out during the COVID-19 pandemic – including two separate lockdowns and several restrictions- since studies developed during this period in other countries also showed levels of PD closer to those found in this study (e.g., Hayashi et al., 2022). However, the literature is unequivocal in that it indicates that the occurrence of PD has been a worrying phenomenon in recent years in the senior population, independently of the pandemic context (Kikuchi et al., 2013; Li et al., 2021).
We also found moderate levels of loneliness and ageism. A large body of research corroborates this finding, indicating the high prevalence of these two phenomena that holistically affect mental health, especially in the occurrence of anxious and depressive symptoms (Cacioppo & Cacioppo, 2018; Mikton et al., 2021). Some studies associate this unusual occurrence of loneliness in seniors in recent decades to factors such as the lack of post-retirement and post-widow's social resources, changes in family configurations and family support, and changes in socialization resulting from digitalization (Cacioppo & Cacioppo, 2018; Chawla et al., 2021). Whereas ageism appears associated with the persistence of collective social beliefs of fragility/dependence in aging and disinvestment in the role of seniors as active agents in society (Chang et al., 2020; Mikton et al., 2021). Despite this evidence, it was also found that the seniors in this study showed moderate levels of resilience, as previous studies have reported (Färber & Rosendahl, 2020). Studies show that higher levels of resilience are associated with life satisfaction and positive affect, as well as lower levels of mental problems (Färber & Rosendahl, 2020). Further, resilience is a protective factor for mental health that is modifiable, which means that resilience in seniors can be enhanced and improved even in adverse contexts, including among older seniors (Färber & Rosendahl, 2020; Fontes & Neri, 2015).
It was found that seniors with higher levels of resilience may be more likely to prevent ageism from having a direct impact on their mental health. In fact, literature shows that resilience has several characteristics that can be essential in responding to ageism experiences, particularly by increasing the ability to respond to the demands of the environment by improving adaptability, promoting the creation of solid support networks, and promoting optimism and patience even under adverse conditions (Ayed et al., 2018; Mikton et al., 2021). Further, ageism tends to negatively impact seniors' self-concept and sense of usefulness and purpose, while resilience is characterized by promoting increased self-esteem, confidence, and personal reinvention, contributing to a sense of need for continuous personal adjustment and learning (Ayed et al., 2018; Chang et al., 2020). Despite this important protective role of resilience on mental health, the scarcity of literature that addresses the potential of resilience against ageism in seniors is alarming (Ayed et al., 2018; Hardy et al., 2004). This finding emphasizes the need for more research in this promising area, reinforcing the importance of decentering research from themes focused on the negative consequences of ageism, and investing more in individual characteristics and competences that can combat it and improve mental health, such as resilience (Hardy et al. al., 2004; Hu et al., 2020). Recent research suggests that resilience is dynamic and can be trained, which gives it even greater potential in possible interventions for mental health in seniors, particularly in the most isolated and stigmatized people (Linz et al., 2019).
In addition, seniors with high levels of resilience may be more likely to significantly reduce the impact of loneliness on their mental health, but this was insufficient to annul the direct negative impact of loneliness. This result of partial mediation of resilience has already been verified in some studies that evaluated the impact of loneliness on specific dimensions of mental health, such as depressive symptoms (Zhao et al., 2018) or quality of life (Gerino et al., 2017). Effectively, resilience facilitates a sense of agency and an internal locus of control, stimulates social/relational involvement and promotes problem-solving skills among seniors, which highlights its protective role of mental health in the face of loneliness (Ayed et al., 2018; Fontes & Neri, 2015). However, resilience was more effective in protecting seniors' mental health against ageism than loneliness, and this may be due to the "continued" nature of loneliness (Cacioppo et al., 2014). One of the key characteristics of resilience is the ability to enable people to successfully recover after disruptive events, such as events of stigmatization of seniors due to age, be these unique or intermittent (Chang et al., 2020; Southwick et al., 2014). In contrast, loneliness is not characterized as an event, as it refers to a state, a continued feeling of disconnection, a low sense of belonging and isolation; thus, the isolated action of resilience may be more conditioned in the face of loneliness, and with a greater need for joint action with other protective variables (e.g., purpose-in-life, optimism, social connections) for a more effective response (Chang et al., 2020; Hawkley & Cacioppo, 2010; Musich et al., 2021; Southwick et al., 2014).
Lastly, it is important to point out that despite resilience having been an important protective factor of mental health for loneliness, and especially for ageism, recent research indicates the importance of considering mixed intervention approaches, with intrinsic and extrinsic factors, in order to intervene on the mental health of seniors (Zhao et al., 2018). That is, on the one hand can be integrated and adapted principles of resilience stimulation, namely the principles considered by Windle (2010) and the findings of Madsen and collaborators (2019), such as investment in sense of belonging and promoting a sense of agency, empowerment, and recognition of personal "strengths". On the other hand, it may be important to also integrate factors such as social support, which have been consistently shown as playing and important protective role for mental health against ageism and loneliness in the senior population (Hutten et al., 2021; Redman & Shane, 2006).
This article also has some limitations to should be acknowledged. The sampling process was non-probabilistic, which limits the generalization of the presented findings. Data collection was also carried out through an online protocol, which may have influenced the participation of more motivated and computer literate seniors. Furthermore, the robustness of the results could be greater if latent variables were used in the structural equations model. Lastly, the AAS was used to measure ageism, which is not a measure of direct experience of ageism, but rather a measure of perceived ageism, thus in this study the levels of ageism reported can be referred more to perceived ageism in the community or in social and personal life than the direct experience of ageism situations.
ConclusionThe literature leaves no doubt in identifying ageism and loneliness as two main global phenomena with important negative consequences on the mental health of seniors, especially on Psychological Distress. Resilience has consistently been shown to be one factor that may protect the mental health. Particularly, in the senior population resilience has the potential to be improved and increased. In this study, it showed remarkable potential in protecting mental health against ageism, and partial protection of mental health against loneliness. Therefore, it is suggested to integrate the principles of promoting resilience in interventions to improve well-being and mental health of seniors.
Compliance with ethical standardsAll procedures were in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the ethics committee of ISPA – University Institute with approval code n° D/028/04/2020.
Author contributionsJARG participated in the research design, data collection, data analysis, and manuscript elaboration and revision. PAC participated in the data analysis and manuscript revision. IL participated in the manuscript revision. All authors contributed to the article and approved the submitted version.
FundingThis work is funded with national funds from FCT – Fundação para a Ciência e Tecnologia, I.P., in the context of the project UID/04810/2020 and under grant SFRH/BD/143214/2019.