Edited by: Óscar F. Gonçalves
More infoMental health disorders pose a significant challenge to society. The Bayesian perspective on the mind offers unique insights and tools that may help address a variety of mental health conditions. Psychopathological dysfunctions are often connected to altered predictive and active inference processes, in which cognitive and physiological pathogenic beliefs shape the clinical condition and its symptoms. However, there is a lack of general empirical models that integrate cognitive beliefs, physiological experience, and symptoms in healthy and clinical populations. In this study, we examined the relationship between altered predictive mechanisms, interoception, and pathological bodily distortions in healty individuals and in individuals suffering from anorexia nervosa (AN). AN patients (N=15) completed a Virtual Reality Full-Body Illusion along with interoceptive tasks twice: at hospital admission during an acute symptomatological phase (Time 1) and after a 12-week outpatient clinical weight-restoring rehabilitative program (Time 2). Results were compared to a healthy control group. Our findings indicated that higher levels of interoceptive metacognitive awareness were associated with a greater embodiment. However, unlike in healthy participants, AN patients' interoceptive metacognition was linked to embodiment even in multisensory mismatching (asynchronous) conditions. In addition, unlike in healthy participants, higher interoceptive metacognition in AN patients was related to prior abnormal bodily distortions during the acute symptomatology phase. Prediction errors in bodily estimates predicted posterior bodily estimate distortions after the illusion, but while this relationship was only significant in the synchronous condition in healthy participants, there was no significant difference between synchronous and asynchronous conditions in AN patients. Despite the success of the rehabilitation program in restoring some dysfunctional patterns in the AN group, prediction errors and posterior estimate distortions were present at hospital discharge. Our findings suggest that individuals with AN prioritize interoceptive metacognitive processes (i.e., confidence in their own perceived sensations rather than their actual perceptions), disregarding bottom-up bodily inputs in favour of their prior altered top-down beliefs. Moreover, even if the rehabilitative program partially mitigated these alterations, the pathological condition impaired the patients' ability to coherently update their prior erroneous expectations with real-time multisensory bottom-up bodily information, possibly locking the patients in the experience of a distorted prior top-down belief. These results suggest new therapeutic perspectives and introduce the framework of regenerative virtual therapy (RVT), which aims at utilizing technology-based somatic modification techniques to restructure the maladaptive priors underlying a pathological condition.
Mental health issues are a widespread burden of our society, notwithstanding there is a substantial disparity between those who require mental health care and those who can access effective therapeutic solutions (Pender, 2022). This gap in mental health care has led to intense debate regarding diagnostic and prognostic relevance in health practices, resulting in a paradigmatic crisis (Rose, 2016) that forecasts two opposite interpretations (Glannon, 2020).
On the one hand, biological psychiatry is supporting the idea that mental illness can be described as nothing more than chemical imbalances within the brain, where psychoactive drug treatments that alter the chemical makeup of the brain represent the preferred choice for intervention (Pender, 2022). On the other side, psychotherapy suggests that the individual's environment and life experiences are inextricably linked to how the brain develops, copes, and interacts, as people's perceptions of their reality can result in pathological symptoms and, in the same manner, these perceptions can be altered to address the symptoms themselves (Mackay, 2003).
The concept of the Bayesian brain offers a possible solution to this conundrum, as it is presenting itself as an emerging new neuroscience paradigm (Huang and Rao, 2011; Friston, 2018; Smith et al., 2021). The fundamental assumption of this paradigm is that the brain functions as an active inference machine that actively learns the statistical patterns of the outside environment and develops predictions to improve the efficiency of information processing and sensorium comprehension. In this view, mental health is the outcome of an "embodied self" that (Putica et al., 2022): (1) anticipates the sensory input it will experience if one course of action or another is chosen, (2) acts upon the environment and changes it according to expectations and desires, (3) experiences the result of action selection, (4) modifies itself both at cognitive (subjective expectations) and bodily (proprioceptive and interoceptive states) levels, and (5) updates pre-existing models in response to unexpected results. This vision has led to the emergence of a new research field - clinical computational neuroscience (Smith et al., 2021) - that suggests how mental problems can be interpreted as the outcome of a dysfunction in the representations (predictions) of the inner and outer worlds generated by the brain. In this view, mental health disorders can therefore be the outcome of an impaired, overly precise, updating mechanism that cannot integrate new sensory inputs because it relies more on the weight of prior pathological beliefs.
Several clinical conditions might incorporate these prior pathological beliefs, and among these clinical conditions, Anorexia Nervosa (AN) seems to offer a functional field of study to better understand how perception, cognition, and a Bayesian account of the mind are related to psychopathological dysfunctions.
AN is a severe disease that incurs, among other diagnostic criteria, in “a disturbed view of one's own weight or body shape, undue influence of weight and shape on self-evaluation, or denial of the seriousness associated with current low body weight” (DSM-5, 2013). Recent systematic reviews and meta-analyses found higher consistency in the overestimation of body percept in AN (Gardner & Brown, 2014; Glashouwer et al., 2019). Patients suffering from AN often report distortions in their bodily experiences and representations (Cash and Deagle, 1997; Dakanalis et al., 2016). Similar findings have been found also by Keizer and colleagues (Keizer et al., 2013), who concluded that body representation disturbances in AN operate both at a conscious perceptual-cognitive level (i.e., body image) and at an unconscious motor level (i.e., body schema).
Notwithstanding, these frameworks missed perhaps the most crucial aspect of our wellbeing, which is the experience of our body from within – known as interoception. Interoception is defined as “the process by which the nervous system senses, interprets, and integrates signals originating from within the body, providing a moment-by-moment mapping of the body's internal landscape across conscious and unconscious levels” (Owens et al., 2018). In this regard, a recent systematic review highlighted the presence of interoceptive deficits in eating disorders, suggesting that interoception might play a role as a transdiagnostic feature of this specific clinical dimension (Martin et al., 2019). In support of this, several pieces of evidence found interoceptive alterations in patients suffering from AN. Neuroimaging evidence identified white matter abnormality and altered resting-state functionality (Gaudio et al., 2015; Gaudio et al., 2017) in AN subject's interoceptive network, moreover Kerr et al. (2016) found altered insula activity in weight restored AN patients. Furthermore, different studies (Pollatos et al., 2008; Fischer et al., 2016) reported interoceptive behavioural deficits in AN where patients were less accurate in detecting their interoceptive sensations (heartbeat) compared to healthy controls. Similarly, evidence from a single case study described a complete interoceptive axes dissociation in a patient suffering from AN where the detection of interoceptive inputs was completely absent but, at the same time, the patient's metacognitive confidence in these distorted perceptions was extremely high. This is as if the patient was disregarding bottom-up information, favouring top-down metacognitive beliefs leading to overconfidence in the erroneous altered bodily perceptions (Di Lernia et al., 2019).
In the present study, we sought to collect evidence of altered predictive mechanisms in a sample of patients suffering from AN, exploring how these alterations are connected to inner bodily perceptions (interoception) and to the pathological bodily distortions that characterize this clinical condition. To pursue this objective, we used a well-validated Virtual Reality (VR) Full-Body Illusion (Serino et al., 2016) along with interoceptive perception tasks to explore how inner bodily perception (interoception) is related to embodiment, bodily representations and multisensory integration distortions in individuals suffering from AN. Patients suffering from AN performed the evaluation two times; at hospital admission, during an acute symptomatological phase (Time 1) and after a 12-week outpatient clinical weight-restoring rehabilitative program (Time 2). Moreover, AN results were compared to a healthy control group.
As a general model, we defined a Bayesian framework applied to bodily perception and VR Full-Body Illusion that comprises a prior estimate, namely an index of estimate distortion before the VR illusion, and a posterior estimate, namely an index of estimate distortion after the VR Full-Body Illusion. Under a Bayesian predictive account (Friston, 2010; Friston et al., 2014; Ondobaka et al., 2015; Friston et al., 2016) we, therefore, regarded (i) patients’ priors (expectations) as the degree of distortion between their perceived body and their real body before a multisensory VR Full-Body Illusion, (ii) posterior estimations, as the degree of distortion between their perceived body illusion and their real body after a VR Full-Body Illusion, (iii) the likelihood as the plausibility of the virtual body (avatar) in relationship to the patient's real body, and (iv) the prediction error has the distance between expectation (priors) and reality (likelihood). With these terms, we were able to describe a Bayesian model of bodily estimation adapted to VR Full-Body Illusions that allows estimating priors, posteriors and the prediction error of bodily perception, weighting both the actual bodily dimensions of the participant taking part in the illusion and the dimension of the avatar used in the VR Full-Body Illusion. As body illusions involve both a synchronous and an asynchronous (control) stimulation of the participant's visual and tactile systems, literature indicated a reduced perception of embodiment in the asynchronous condition compared to the synchronous condition (Keizer et al., 2014). However, Keizer et al. (2016) utilizing a VR Full-Body Illusion also showed that individuals suffering from AN based their bodily estimations on the most recent available visual inputs, rather than their afferent (proprioceptive) bodily signals, as results were found both in the synchronous and the asynchronous conditions. Authors, therefore, suggested that individuals suffering from AN might disregard afferent proprioceptive inputs, favoring top-down perceptions.
Following these premises and previous literature evidence on interoceptive dissociation in patients suffering from AN (Di Lernia et al., 2019), the study has the following hypotheses.
Regarding the relationship between interoceptive processes and embodiment in AN we would hypothesize that i) interoceptive metacognitive beliefs rather than actual interoceptive perception (i.e., detection) would predict the extent to which patients suffering from AN experienced embodiment over a virtual body. Conversely, we do not expect that interoceptive perception will play a role in healthy control participants, as recent literature indicated no role of heartbeat detection in embodiment processes (Crucianelli et al., 2018; Horváth et al., 2020).
Regarding the relationship between interoceptive processes and bodily distortion estimates in AN, we would hypothesize that ii) interoceptive metacognitive beliefs would predict the extent of prior bodily distortions in AN.
For both these hypotheses, we would hypothesize that the contribution of interoceptive variables will not depend on the synchronous or asynchronous (control) condition, as individuals suffering from AN might disregard bottom-up bodily inputs in favour of top-down perceptions, in line with previous results on the proprioceptive domain (Keizer et al., 2016), as opposed to healthy participants.
Regarding the predictive Bayesian account of the relationship between multisensory bodily illusions and bodily distortions in AN, we would hypothesize that (iii) multisensory body prediction errors would predict the extent of posterior bodily distortions, such as the larger the bodily prediction error, the larger the perceived bodily distortions.
Lastly, as the severity of symptoms in individuals suffering from AN is linked to alterations in bodily processing, we would hypothesize that the pathologically altered bodily processes in individuals suffering from AN, will be also moderately improved due to the rehabilitative clinical intervention.
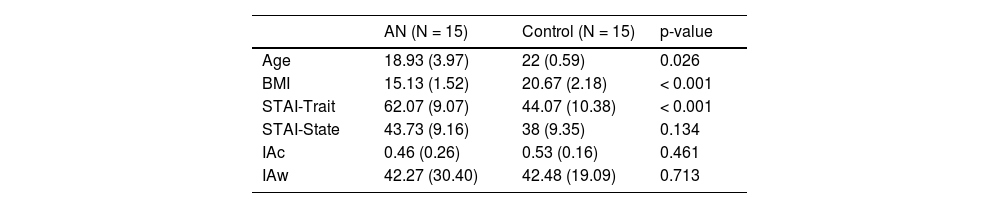
MethodsParticipantsFifteen patients affected by Anorexia Nervosa (AN) took part in the study. The mean age at the beginning of the study was 18.93 (SD = 3.97) with a mean BMI of 15.13 (SD = 1.52), At the beginning of the study mean Trait Anxiety was 62.07 (SD = 8.74), State Anxiety was 43.73 (SD = 9.16). Patients suffering from AN were recruited from the Outpatients Rehabilitative Service of the Eating Disorders Centre, Division of Endocrine and Metabolic Diseases, San Luca Hospital (Milan, Italy). AN diagnosis was performed according to the clinical criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fight Edition (DSM-V) (APA, 2013) were carried out based on clinical interviews completed by clinical staff. All patients were recruited at hospital admission during an acute symptomatological phase (Time 1), and the experimental procedure was repeated at hospital discharge (Time 2), after a 12-week weight-restoring rehabilitative program. The rehabilitative program provided a multidisciplinary approach, including several different experts (i.e., endocrinologists, psychiatrists, psychologists and dietitians) for delivering a personalized outpatient service, focused primarily on weight and dietary rehabilitation and education. The program lasted typically 12 weeks, and it was specifically customized according to the clinical needs of every single patient in terms of frequency and clinical activities - see Di Lernia et al. (2019). In addition, 15 healthy young females, with no active or past diagnosis of AN and with healthy BMI, were recruited and assessed as a control group. The mean age was 22 (SD = 0.59) with a mean BMI of 20.67 (SD = 2.18), The mean State Anxiety was 38 (SD = 9.35) and Trait Anxiety was 44.07 (SD = 10.38). Participants did not receive money nor any form of compensation for their participation in the study. Table 1 reports the descriptive and clinical characteristics of the samples included. Written informed consent was obtained from all participants (or their parents, in the case of a minor) to be included in the study. The study was conducted in compliance with the Helsinki Declaration (of 1975, as revised in 2008), and was approved by the Ethics Review Board of the Istituto Auxologico Italiano.
.
Note: Wilcox test was used to assess sample characteristics. Mean and SD are reported.
After entering the experimental room, patients and healthy control participants received instructions about the procedure and were familiarized with the settings. After signing the informed consent, patients were connected to a three-lead ECG sampling at 1000Hz (biosignalplux.com) to perform a complete interoceptive assessment for interoceptive accuracy (IAc) measured with an HCT (Schandry, 1981), and interoceptive metacognitive confidence (IAw) measured with a VAS on the performance at the HCT (Garfinkel et al., 2015). Patients also took time to compile questionaries for self-reported state and trait anxiety measures with the STAI (Spielberger et al., 1970). After that, they completed a first pre-illusion estimation of their body size with the Body Part Size Estimation Task. Subsequently, they were invited to wear a head-mounted display (Oculus Rift DK2, connected to a portable computer HP TRUE VISION with CPU Intel® Core™i7) to experience the VR Full-Body Illusion. In a randomized order, they experienced the synchronous (i.e., experimental condition) and the asynchronous (i.e., control condition) visuotactile stimulation. After both stimulations, patients were asked to complete the Embodiment Questionnaire (Serino et al., 2016) to measure the strength of the illusion and to complete the Body Size Estimation Task. At the end of the entire procedure, their actual body measures were collected. This procedure was performed at hospital admission (Time 1) and after the 12 weeks rehabilitative program (Time 2). Healthy control participants performed the same procedure, in a single experimental session.
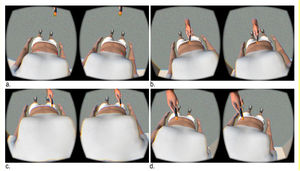
MaterialsVirtual reality full-body illusionThe VR Full-Body Illusion (Fig. 1.) utilized the avatar of a young female girl (approximately 20-25 years old) with a thin body (waist circumference: 73.94 cm, hips circumference: 96.72 cm) immersed in a stimulus-free room. The virtual room was developed with the software Unity3D (www.unity3d.com), while the avatar was modelled using the software MakeHuman (http://www.makehuman.org/). To induce the illusion of being the owner of the avatar, patients suffering from AN and healthy controls were asked to visualize in first-person perspective the avatar through the head-mounted display, while receiving a multisensory stimulation involving the visual system (i.e., what they saw on the virtual body) and the tactile proprioceptive system (i.e., tactile stimulation to their own actual body). In the “synchronous visuotactile stimulation” (i.e., experimental condition), participants felt a touch on their abdomen for 90 s while synchronous stimulation was provided in VR to the avatar's abdomen. This was achieved using a brush attached to a motion-tracking device (i.e., Razer Hydra). In the “asynchronous visuotactile stimulation” (i.e., the control condition) the same visuotactile stimulation was provided on the participants' abdomen for 90 s, but there was a temporal delay between the visual and tactile stimulation (i.e., absence of a synchronous match between tactile and visual stimulation). In the asynchronous condition, the experimenter recorded the tactile stimulation by pressing a button on the Razer Hydra at the beginning of the movement, which paused the image seen by participants. The tactile stimulation was later replayed in VR at the end of the movement, thus inducing a mismatched multisensory stimulation between what participants felt and what participants saw in the VR scenario.
Virtual Reality Full-Body Illusion: (a) a calibration procedure identifies four markers on the avatar's abdomen. The markers are matched with the corresponding bodily locations of the participant's real body, creating a virtual plane on the participant's abdomen to allow the visuotactile stimulation to adhere to the participant's bodily morphology, without colliding (e.g., trespassing) the avatar; (b.) the researcher can therefor move hand-tracked virtual brush, movements are mapped in the VR scenario in real-time; (c.) the researcher can perform a visuotactile stimulation of the participant's body moving the virtual brush from side to side, touching the participant's real body at the same time. In the sync condition, tactile and visual stimulation are performed synchronously. In the async condition, the participant feels the touch on the abdomen but sees the movement in the virtual scenario with a 30s delay.
Before the illusion was induced (i.e., baseline), after both the synchronous (i.e., experimental condition) and the asynchronous visuotactile stimulation (i.e., control condition), patients suffering from AN and healthy control participants were asked to estimate the width and circumference of three body parts (shoulders, waist and hips) as in Serino and colleagues (Serino et al., 2016). In the current study, we focused on two different body estimates, namely the circumference of two different body parts: the waist and hips. These specific body parts were selected to allow comparison with the avatar's body part for which precise measures were defined, i.e., the avatar's body was built with a waist circumference of 73.94 cm and the hips circumference of 96.72 cm. In particular, participants were provided with a piece of rope, and they were asked to draw a circle/oval on the floor representing the perceived size of the same body parts. At the end of the entire experiment, the experimenter measured the actual width and circumference of the targeted body parts. For each body part, we calculated the delta of misestimation between real and estimated measures.
Embodiment questionnaireAfter both conditions, patients suffering from AN and healthy control participants were required to fill out the Embodiment Questionnaire, adapted from (Piryankova et al., 2014) and previously used in (Serino et al., 2016). It consists of 20 items on a 7-point Likert scale. This self-report questionnaire measures the strength of the illusion in terms of 1) body ownership (i.e., the sense of being the owner of the virtual body); 2) self-location (i.e., the sense of being in the same spatial location of the virtual body); and 3) sense of agency (i.e., the sense of being in control of virtual body’ actions). The three subscales were calculated by averaging the responses from the corresponding items.
Interoceptive measuresFollowing previous literature (Di Lernia et al., 2019), we performed a detailed interoceptive assessment, collecting both interoceptive accuracy (IAc) and interoceptive metacognitive awareness (IAw), at the beginning (Time 1) and at the end of the rehabilitative program (Time 2).
Specifically, IAc measured with the HCT (Schandry, 1981) is a behavioural index that reports the patients’ ability to correctly perceive inner bodily cardiac sensations. The task asks participants to silently count their heartbeat focusing only on inner bodily sensations, without taking the pulse and without making an inference based on time perception. Participants have to count their heartbeats in a specific time span marked by two audio cues and report only the heartbeats they felt, without guessing or estimating the number of beats (Desmedt et al., 2020). The reported heartbeat count is compared to the real heartbeat number measured through an ECG and a global performance index is calculated according to the following formula: 1/3∑(1–(|recorded heartbeats – counted heartbeats|) / recorded heartbeats). Index scores can vary between 0 and 1, where lower values indicate poorer performances. In our study, patients were connected to a portable ECG unit sampling at 1000 Hz with Ag/AgCl electrodes and they were instructed to count their own heartbeats in specific intervals time intervals of 25, 35, and 45 s. Adjusted instructions were used following recent literature guidelines (Corneille et al., 2020).
Interoceptive confidence refers to the construct of IAw originally developed by Garfinkel et al. (2015) that assesses participants’ confidence in the answers to the accuracy task. In Garfinkel et al. (2015) participants were invited to report their confidence regarding the responses to the HCT without any feedback on the actual performances. Responses were given on a VAS that ranged from 0 (Not Confident at All) to 100 (Fully Confident). The metacognitive index was originally calculated as the within-participant Pearson correlation between confidence and accuracy (Garfinkel et al. 2015). Nonetheless, Garfinkel et al. (2015) utilized a modified version of the heartbeat counting task, while this study utilized the original Schandry task (Schandry, 1981) since the original task has already been utilized in several studies (Di Lernia, Serino et al., 2016; Di Lernia et al., 2020) thus allowing comparison of results across the literature. Considering the structure of the original Schandry task, the within-participant correlation would have not provided reliable statistical information, therefore raw VAS confidence scores are reported as a proxy of interoceptive confidence. It has also been suggested, in predictive coding terms, that confidence may index the ‘precision’ of interoceptive sensations (Allen et al., 2019).
Bayesian embodiment and bodily prediction error in virtual avatarsIn the present study, we describe a Bayesian model of bodily estimation adapted to virtual reality bodily illusions that allow estimating the prediction error of bodily perception, weighting both the actual bodily dimensions of the participant taking part in the illusion and the dimension of the avatar used in the virtual illusion.
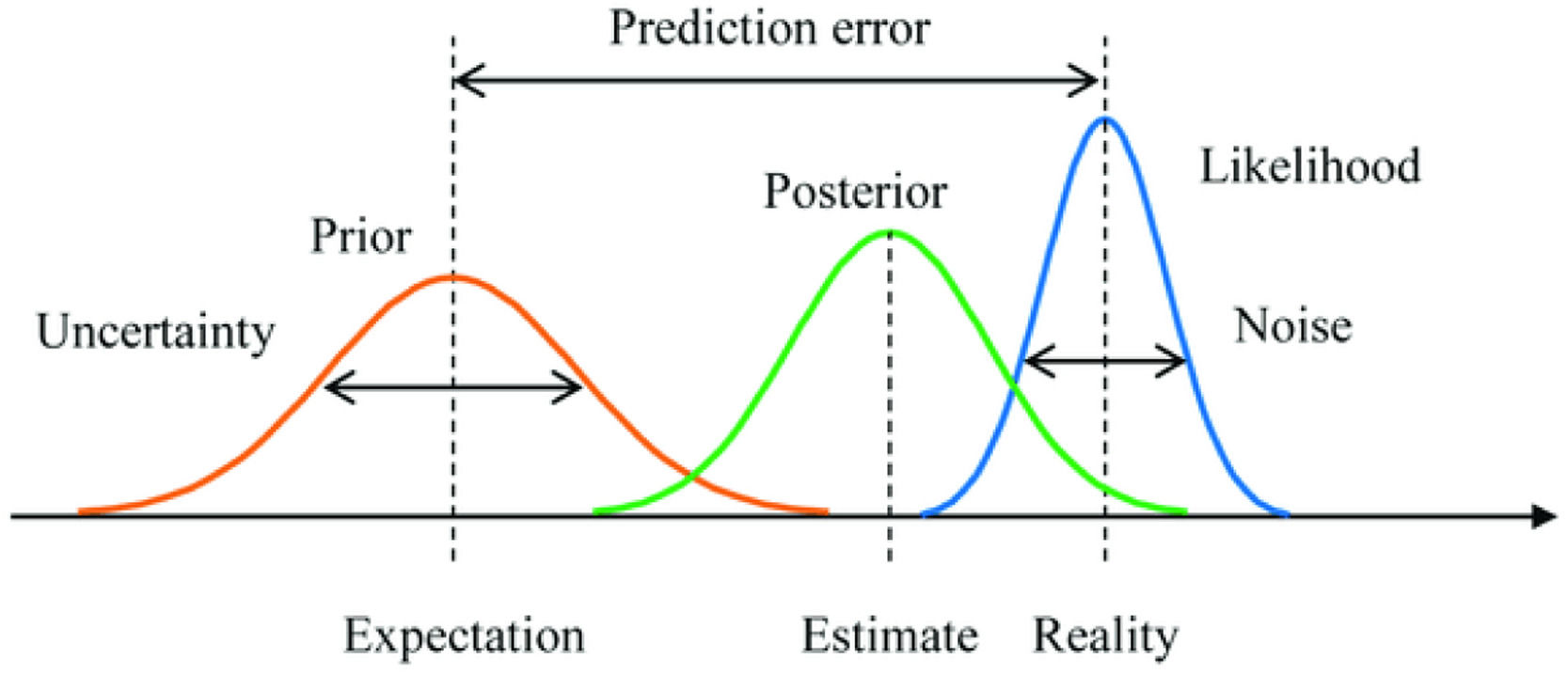
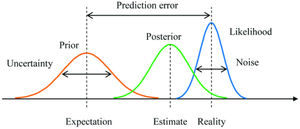
According to the Bayesian framework, four core elements describe the probabilistic inference process: the likelihood as the distribution of the observed data marginalized over the parameter(s) (i.e., reality). The prior is the distribution of the parameter(s) before any data is observed (i.e., expectation or belief). The posterior is the distribution of the parameter(s) after considering the observed data (i.e., estimation). Lastly, the prediction error, which in this case is described as the distance between reality (likelihood) and expectation (prior). See Fig. 2.
Example of Bayesian inference with a prior distribution, a posterior distribution, and a likelihood function (Yanagisawa et al., 2019).
In the context of a body virtual reality illusion, these parameters can be adapted to extract fundamental estimate distortion indexes, in the context of an experimental design that requires the participant to estimate their bodily size perceptions, before (prior) and after (posterior or estimation) a given experimental procedure in virtual body avatar. In this case, the posterior factor can be represented by the estimation of the body (Body Size Estimation Task) in relation to the actual dimension of the participant's real body, according to the formula:
This factor represents a distortion estimation index that reports how much patients suffering from AN can accurately estimate a given dimension of their body (e.g., hips circumference), after (post) each stimulation. Similarly, the prior factor represents the participants’ perceptual belief regarding the dimension of their own body, namely their expectation regarding a given dimension of their body prior to any stimulation. The prior factor can therefore be represented by the formula:
This factor represents a distortion estimation index that reports how much patients suffering from AN can accurately perceive a given dimension of their body (e.g., hips circumference), before (pre) any stimulation, therefore presenting their perceptual expectations about their own body. Lastly, the likelihood factor can be described as the plausibility of the virtual body (avatar) in relationship to the patient's real body. The likelihood factor can therefore be represented by the formula:
This factor represents a distortion estimation index that reports how much the avatar is similar to the participants’ real body, therefore providing a likeness index of the avatar in comparison to the real body. Given these terms, and accordingly, to the Bayesian framework, the prediction error of a bodily illusion can be described as the distance between reality and expectation, represented by the following formula: Prediction Error = Likelihood - Prior or, in our terms:
In this case, the prediction error represents a distortion estimation index that reports how much the plausibility of the avatar in relation to the real body is different from the participants' perceptual beliefs (expectations) in relation to their own real body. Ultimately, given these terms, we can describe a Bayesian embodiment model that predicts posterior bodily estimations for a given parameter:
The model proposed can work as a generic predictive model for Bayesian embodiment and bodily prediction error in virtual avatars. For this study, we divided for each level of time (Time 1 and Time 2), stimulation (Condition: synchronous and asynchronous), and Group (Control and AN)
Statistical analysesWe used R version 3.6.3 for the analyses (R Core Team, 2014). In particular, we used linear mixed-effects ANOVA (Luke, 2017) for the pre-post effect model and robust linear regression for the Bayesian model to evaluate the significance of each predictor. The mixed-effects ANOVA models were run with lme4 package (Bates et al., 2015) and Bobyqa optimizer was applied (Brown, 2021). To account for intra-participants variability, we put patients ID as random factor with random intercept (R formula: outcome ∼ fixed effects + (1|ID). Models’ assumptions of normality of residuals and homoscedasticity were verified by visual inspection. As the control group was only assessed once (no rehabilitative intervention was administered to healthy controls), we used this as baseline to assess any changes in the AN group with separate models for Time (Time1 and Time2 models). One AN patient dropped-out at Time2. Missing values were not imputed as mixed-effects model handles missing values without removing the case but rather the missing observation. Partial eta squared (η2p) was interpreted (small = 0.01, medium = 0.06, and large = 0.14) according to Richardson (Richardson, 2011). The significance level for all the analyses was set to 0.05.
ResultsAs a preliminary check, we evaluated changes in BMI before and after the 12-week rehabilitative program (one-way within ANOVA) between the admission – start of the rehabilitative program (Time 1) and the hospital discharge - end of the rehabilitative program (Time2). We found that the rehabilitation program significantly improved patients’ BMI (F1,44 = 45.23, p < 0.001, η2p = 0.51 95% CI[0.29,0.65]). At Time1 the mean BMI was 15.13 (SD = 1.54) whereas at Time2 was 16.64 (SD = 1.34), which however was still below normative values for a healthy BMI suggesting that patients suffering from AN were still not fully clinically recovered after the rehabilitative program.
In order to check if age significantly affected our results we ran the models with age as a covariate, this did not alter our results, so we provided the models without age as a covariate. Descriptives for all the relevant variables are reported in Tables 2–4.
Descriptive statistics for Anorexia Nervosa group at Time 1.
Descriptive statistics for Anorexia Nervosa group at Time 2.
Descriptive statistics for the Healty participants group.
To check if the VR Full-Body Illusion was effective, we analysed the effect of the Illusion with separate models for Time1 and Time2 (2 × 2 mixed ANOVAs, within factor: Condition: Synchronous Vs Asynchronous visuotactile stimulation; and Group factor: AN Vs controls). Here we focused only on avatar ownership and agency (see supplementary materials for self-location). In the ownership Time1 model, we found a main effect of Condition (F1,27 = 11.57, p = 0.002, η2p = 0.3). In the synchronous condition, the ownership was higher (M = 3.91, SD = 0.98) than in the asynchronous condition (M = 3.26, SD = 0.93). No other main or interaction effects were found, suggesting that patients suffering from AN experienced the full bodily illusion similarly to healthy control participants, regarding the avatar's embodiment.
In the ownership Time2 model, we found a main effect of Condition (F1,26 = 9.39, p = 0.005, η2p = 0.27). In the synchronous condition, the ownership was higher (M = 3.85, SD = 1.02) than in the asynchronous condition (M = 3.2, SD = 0.94). No other main or interaction effects were found, confirming findings at Time 1.
In the agency Time1 model, we found a main effect of Condition (F1,27 = 13.05, p = 0.001, η2p = 0.33). In the synchronous condition the agency was higher (M = 4.14, SD = 1.51) than in the asynchronous condition (M = 3.16, SD = 1.32). Moreover, we found a main effect of Group (F1,27 = 5.97, p = 0.021, η2p = 0.18). In the control group, the agency was higher (M = 4.33, SD = 1.46) than in the AN group (M = 2.91, SD = 1.17). No interaction effect was found.
In the agency Time2 model, we found a main effect of Condition (F1,26 = 12.78, p = 0.001, η2p = 0.33). In the synchronous condition, the agency was higher (M = 4.31, SD = 1.42) than in the asynchronous condition (M = 3.25, SD = 1.32). Any other main or interaction effects were found.
Relationship between interoceptive processes and embodiment in ANWe evaluated IAc and IAw at Time1 and Time2 (one-way within ANOVA) and we found no changes in IAc (F1,44 = 1.48, p = 0.229, η2p = 0.03 95% CI[0, 0.19]) and IAw (F1,44 = 0.265, p = 0.609, η2p = 0 95% CI[0, 0.12]) in relation to Time, suggesting no impact of the rehabilitative program (which was focused primarily on weight and dietary rehabilitation) on interoception.
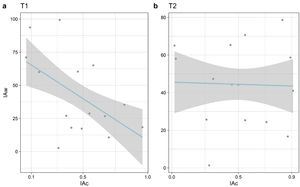
To better understand the relationship between IAc and IAw in patients suffering from AN, we conducted three separate Pearson's correlations for IAc and IAw scores at Time1 (Fig. 3 part a) and Time2 (Fig. 3 part b). We found a significant negative correlation at Time1 (r = - 0.54 95% CI[-0.75, -0.26], p = 0.002) but this correlation was neither significant nor negative at Time2 (r = - 0.03 95% CI[-0.38, 0.33], p = 0.873). Correlations are shown in Fig. 3.
In the control group, we did not find a significant association between IAw and IAc (r = 0.46 95% CI[-0.07, 0.79], p = 0.086). The correlations between IAw/IAc and all the other synchronous/asynchronous embodiment measures were not significant (p-values > 0.05). These results suggest that at hospital admission, during an acute pathological phase, patients’ perception of inner bodily sensation was detached from the metacognitive process. After the rehabilitative program, at hospital discharge, the relationship between interoceptive perception and interoceptive metacognition was partially restored, as no negative correlation was found similarly to the healthy control participants.
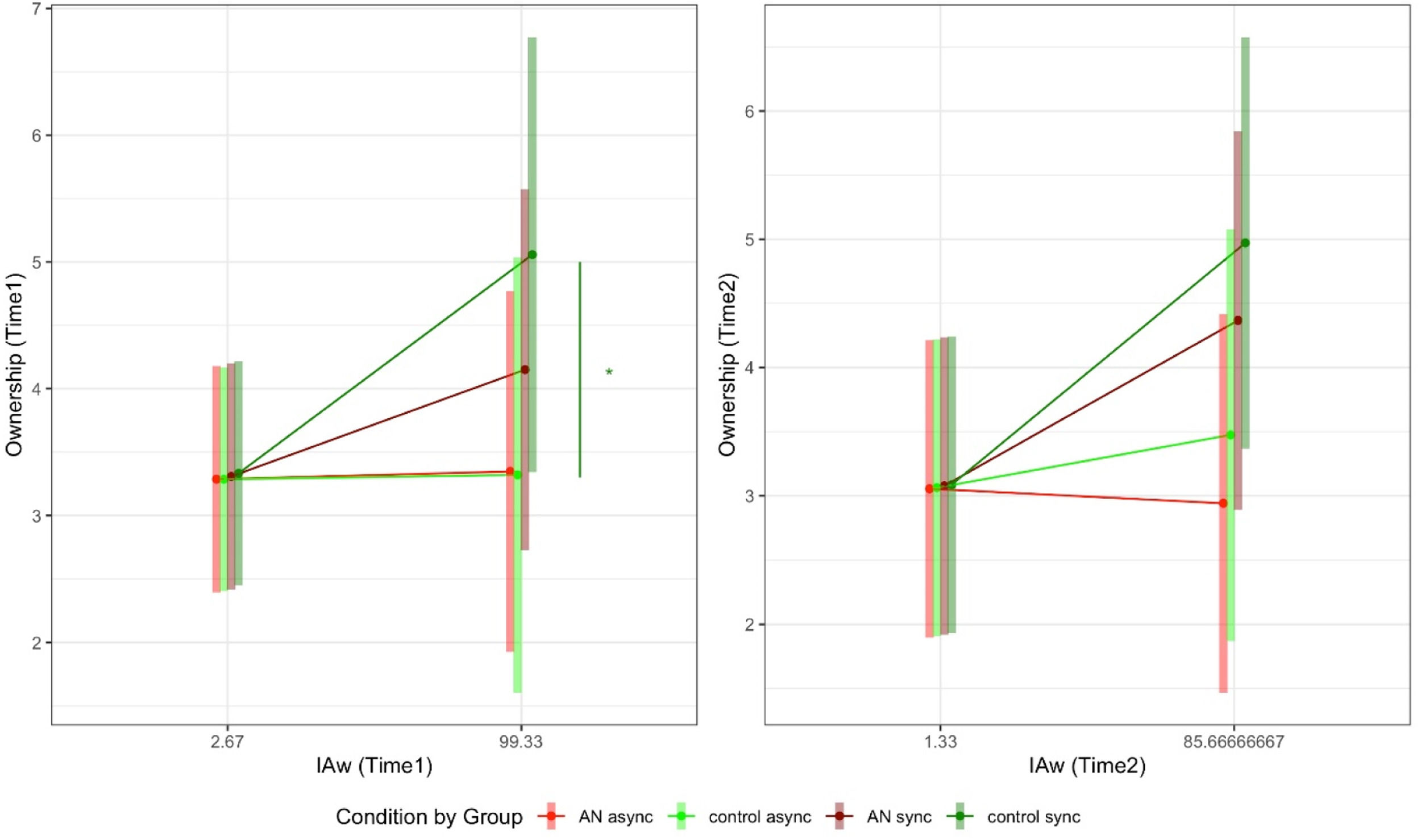
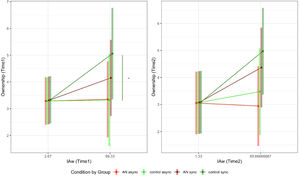
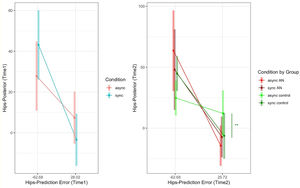
In order to study the impact of interoception in interaction with the Group and Condition on embodiment processes, we performed separate mixed ANCOVAs for IAc and IAw at Time1 and Time2. Post-hoc contrasts of interest were the comparison between the levels of Condition within the groups and the contrast between Groups for each level of Condition. See Fig. 4 for the results mentioned below. Agency and self-location results are reported in the supplementary materials. Regarding ownership at Time1 for the IAc model, we found that the IAc by Group by Condition interaction was not significant. Similarly, we found that the IAc by Group by Condition interaction was not significant at Time 2. These results suggest that IAc does not contribute to the embodiment in patients suffering from AN and in healthy control participants. Regarding ownership at Time1 for the IAw model, we found that IAw by Group by Condition interaction was significant (F1,26 = 3.04, p = 0.035, η2p = 0.31). Post-hoc slope moderation analyses adjusted for Bonferroni correction showed that only in the control group the slopes of the asynchronous and synchronous conditions were statistically significant (est. diff. = -0.02, SE = 0, p = 0.026). In particular, the slope of IAw in the synchronous condition was 0.02 (SE = 0.01), whereas in the asynchronous condition was 0 (SE = 0.01). No other contrast was significant. In the ownership Time2 IAw model, we found that IAw by Group by Condition interaction was significant (F1,26 = 3.8, p = 0.015, η2p = 0.37). However, post-hoc did not show significant contrasts.
Simple slope post-hoc contrasts for Ownership regarding the interaction among Group Condition and interoception (IAw,) at Time1 and Time2. Green segments represent significant contrasts in the control group, the red segment represents significant contrast in the AN group. IAw: interoceptive awareness. *** = p < 0.001; ** = p < 0.01; * = p < 0.05.
In order to assess the effect of interoception and Group on prior estimation, we performed separate between-subjects ANOVAs by IAw and IAc at Time1 and Time2. As the mixed-effects ANOVAs failed to converge we used the analysis of variance with linear regression.
In the prior waist Time1 IAc model, we did not find any significant results. In the prior waist Time2 IAc model, we did not find any significant results.
In the prior hips Time1 IAc model, we only found a main effect of group (F1,56 = 10.86, p = 0.002, η2p = 0.16). AN group had reduced prior hips distortion (M = 20.35, SD = 13.83) compared to the control group (M = 33.57, SD = 17.07). In the prior hips Time2 IAc model, we only found a main effect of group (F1,54 = 20.2, p < 0.001, η2p = 0.27). AN group had reduced prior hips distortion (M = 14.53, SD = 14.9) compared to the control group (M = 33.57, SD = 17.07). In the prior waist Time1 IAw model, we did not find any significant results. In the prior waist Time2 IAw model, we did not find any significant results.
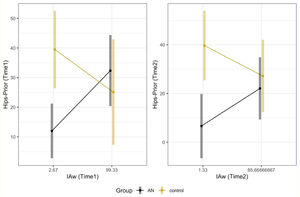
In the prior hips Time1 IAw model, we found a Group by IAw interaction (F1,56 = 4.18, p = 0.045, η2p = 0.07). Post-hoc slope moderation analyses adjusted for Bonferroni correction showed that the slopes of the AN and control group were statistically significant (est. diff. = 0.36, SE = 0.18, p = 0.047). In particular, the slope of IAc in the control group was -0.15 (SE = 0.15), whereas in the AN group was 0.21 (SE = 0.09). In the prior hips Time2 IAw model, we found a Group by IAw interaction (F1,56 = 20.61, p < 0.001, η2p = 0.28). However, post-hoc slope moderation analyses were not significant (p = 0.117). Fig. 5 shows these latter results.
Significant (left panel) post-hoc slope moderation analysis between IAw and Group at Time1 and non-significant post-hoc slope moderation analysis at Time2. IAw: interoceptive awareness; AN: anorexia nervosa. In healthy control participants, interoceptive metacognition was negatively related to bodily distortions. In this case, the more confident healthy control participants were regarding their bodily perceptions, the less they overestimated their bodies. However, patients suffering from AN exhibited an opposite pattern. At Time 1, during the acute symptomatological phase, higher interoceptive metacognition was positively related to prior bodily distortion estimate, indicating that higher interoceptive metacognitive confidence was connected to higher distortion at the body estimation task before the illusion. This pattern was partially restored after a clinical rehabilitation program. At Time 2, no significant differences were found between healthy controls and patients suffering from AN.
In order to study the impact of Condition, Group, and Prediction error on posterior hips estimation (as we did not find any significant results for prior waist estimation, we reported only hips estimation here), we performed mixed ANCOVAs divided by Time1 and Time2. Post-hoc contrasts of interest were the comparison between the levels of Condition within the groups and the contrast between Group for each level of Condition.
For the Time1 model, we found an interaction effect between Condition and Prediction Error (F1,26 = 6.03, p = 0.021, η2p = 0.19). Post-hoc slope moderation analyses adjusted for Bonferroni correction showed that the slopes of the asynchronous and synchronous condition were statistically significant (est. diff. = 0.29, SE = 0.12, p = 0.021). In particular, the slope of the Prediction Error in the synchronous condition was -0.51 (SE = 0.15), whereas in the asynchronous condition was -0.22 (SE = 0.15). We found also a negative association with the posterior estimate of the Prediction Error covariate (est. = -0.31, p = 0.011).
For the Time2 model, we found an interaction effect among Group, Condition, and Prediction Error (F1,24 = 9.56, p = 0.005, η2p = 0.28). Post-hoc slope moderation analyses adjusted for Bonferroni correction showed that only in the control group the slopes of the asynchronous and synchronous conditions were statistically significant (est. diff. = 0.43, SE = 0.12, p = 0.008). In particular, the slope of the Prediction Error in the synchronous condition was -0.51 (SE = 0.16), whereas in the asynchronous condition was -0.14 (SE = 0.16). We found also a negative association with the posterior estimate of the Prediction Error covariate (est. = -0.88, p < 0.001). No other contrasts of interest were found. Fig. 6 shows the significant interaction effects reported in this section.
Simple slope post-hoc contrasts regarding the interaction among Condition and Prediction error at Time 1 and Condition by Group and Prediction error at Time 2. Green segments represent significant contrasts in the control group. *** = p < 0.001; ** = p < 0.01; * = p < 0.05. Results at Time 1 showed that larger prediction error negative values (i.e., overestimation) were related to larger posterior bodily estimation distortions (i.e., overestimation of the real body) after the illusion. These results were true for both patients suffering from AN and healthy control participants at Time 1, during the synchronous condition. This suggests that bodily estimate prediction error was coherently merged with the multisensory integration processes underlying the illusion. Notwithstanding, this pattern was disrupted at Time 2 where significant results for the synchronous condition were found only in healthy control participants.
In this study, we aimed to investigate the relationship between interoception, embodiment, and body perception in a sample of patients suffering from anorexia nervosa (AN) and compare the results to a control group of healthy participants. We collected all relevant variables for the AN group twice: at hospital admission during an acute symptomatological phase (Time 1) and at hospital discharge after a 12-week outpatient clinical weight-restoring rehabilitation program (Time 2). Our results showed that the rehabilitation program, which aimed to improve weight and dietary recovery, was effective in leading to a significant increase in patients' BMI. Although patients remained clinically underweight, the assessment at hospital discharge allowed us to compare changes at two different symptomatological time points (i.e., acute phase versus partially recovered phase).
Several pieces of literature evidence reported deficits in interoceptive perception in AN (Martin et al., 2019), however, these results were often tied to interoceptive heartbeat perception tasks or questionaries and no data were available regarding interoceptive metacognition. Interestingly, but in line with some AN studies (Eshkevari et al., 2014; Ambrosecchia et al., 2017; Lutz et al., 2019), we did not find a significative difference between patients suffering from AN and healthy control participants in interoceptive accuracy or interoceptive metacognition. Moreover, no significant differences were found between before and after the rehabilitative program for the AN group. This indicates that, at least in our AN sample, interoceptive processes were not impaired. A possible explanation for these results might be that in our sample as the AN condition was still in the initial stage, due to the patients’ young age. Albeit clinically relevant, the pathological condition was far from being chronic, and some authors suggested that deficits in AN might be a prognostic evolution in the chronicization of the pathology (Riva & Dakanalis, 2018).
Nonetheless, our findings revealed an intriguing negative relationship between interoceptive accuracy and metacognition in individuals suffering from AN, implying that the less they perceived their inner body, the more confident they were of these erroneous perceptions. From an interoceptive perspective, these results indicate a complete dissociation between AN patients’ inner bodily perception and their metacognitive evaluation of these perceptions. This negative correlation was found only at Time 1 and it replicates the interoceptive axes dissociation found in a previous study (Di Lernia et al., 2019). After the rehabilitative program, no negative correlation was found. This suggests that the relationship between interoceptive perception and interoceptive metacognition was partially restored. In the healthy participants, a statistical trend suggested a strong positive relation between IAc and IAw, which probably did not reach significative levels due to the small sample size. However, the trend for a positive relation between interoceptive accuracy and metacognition in healthy participants was in line with previous literature on interoception (Garfinkel et al., 2015) further supporting the concept of interoceptive axes dissociation in patients suffering from AN (Di Lernia et al., 2019).
Regarding the relationship between interoceptive processes and embodiment, literature on the healthy population provided contradictory results on the role of interoceptive perceptions on embodiment processes. Early evidence (Tsakiris et al., 2011) suggested a positive relationship between interoceptive accuracy and ownership, however recent studies with the RHI found no role for interoceptive accuracy in ownership processes (Crucianelli et al., 2018; Horváth et al., 2020). However, no data in the literature provided insight regarding the role of interoceptive perceptions, and especially interoceptive metacognitive beliefs, in AN embodiment process during a Full-Body Illusion. In this regard, our results suggest that higher levels of interoceptive metacognitive beliefs (i.e., patients’ confidence related to their interoceptive perception, regardless of the accuracy of these perceptions) lead to higher ownership. These results were not found for interoceptive accuracy indicating that body ownership seems to be primarily related to interoceptive metacognitive (top-down) processes, rather than actual inner bodily sensations, in line with recent literature (Crucianelli et al., 2018; Horváth et al., 2020).
During the acute symptomatological phase interoceptive metacognitive beliefs were positively related to the sense of ownership in individuals with AN regardless of the synchronous or asynchronous VR conditions. This suggests that interoceptive metacognitive processes did not coherently contribute to multisensory integration processes in the sense of ownership in AN. It is therefore possible to speculate that patients suffering from AN tend to prioritize top-down metacognitive processes (namely the confidence in their own perceived sensations rather than their actual perception) even in the presence of multisensory bodily afferent mismatching information, thus disregarding bottom-up bodily inputs in favour of their prior altered top-down beliefs, as per previous evidence on the proprioceptive domain (Keizer et al., 2016). These results were not found at hospital discharge, suggesting a rehabilitative effect of the clinical program.
Our further analyses showed that only the healthy control participants demonstrated the integration of interoceptive metacognition in the sense of ownership during the synchronous condition. Specifically, we found that the higher the interoceptive metacognition, the greater the ownership was experienced in the synchronous condition. These findings suggest that healthy participants possess intact multisensory integration processes and can coherently integrate interoceptive metacognition and bottom-up inputs into their sense of ownership.
So far, our results have shown that interoceptive metacognition plays a significant role in embodiment processes. Specifically, we found that in healthy participants, multisensory processes are coherently integrated with interoceptive metacognition. However, in individuals suffering from AN, the multisensory integration processes during the illusion appear to be overridden in favour of top-down metacognitive beliefs that are disconnected from actual bodily sensations, as the less the individuals suffering from AN perceived their inner body, the more confident they were of their wrong perceptions.
Regarding the relationship between interoceptive processes and bodily distortion estimates in AN, we analyzed the potential influence of embodiment and interoceptive processing on altered body perception in individuals suffering from AN. Our findings confirm that interoceptive metacognition has a distinct impact on distortions in prior bodily estimates between the two groups. In healthy control participants, a negative relationship was observed between interoceptive metacognition and bodily distortions. Specifically, higher levels of interoceptive metacognition were associated with lower levels of prior bodily overestimation. This suggests that the more confident healthy control participants were in their bodily perceptions, the less they overestimated their bodies. In contrast, individuals suffering from AN showed the opposite pattern. During the acute symptomatological phase, we found a positive relationship between interoceptive metacognition and prior bodily distortion estimate. This indicates that higher levels of interoceptive metacognitive confidence, which was detached from the detection of inner bodily sensations, were associated with higher distortions at the body estimation task before the illusion. This pattern was partially restored following the clinical rehabilitation program. Interestingly, patients suffering from AN were better at estimating their prior bodily dimensions compared to healthy control, at least in absolute terms. We suspect that this could be attributed to the regular medical evaluations that patients undergo as part of their treatments, which involve frequent measurements of their bodily dimensions. Nonetheless, this unexpected finding did not impair our main results which were focused on the radically different contribution that interoceptive variables had on the body estimation of healthy participants versus patients suffering from AN.
Lastly, regarding the predictive Bayesian account of the relationship between multisensory bodily illusions and bodily distortions in AN, we defined a Bayesian model of bodily estimation adapted to VR Full-Body Illusions that allows us to estimate the prediction error of a bodily perception by weighting both the participant's actual body and the dimension of the avatar used in the virtual illusion. The prediction error in this model represents how much the plausibility of the virtual avatar in relation to the participant's real body is different from the participant's altered expectations (priors) of their body, i.e., how distorted the participant's prior expectation is in comparison to the virtual body within the illusion.
Using this model to compare individuals suffering from AN and healthy control participants, we found that larger negative values for prediction error (i.e., distorted/overestimated prior bodily expectations compared to the virtual body) were associated with larger posterior bodily estimation distortions (i.e., overestimation of the real body) after the illusion. This suggests that prior erroneous beliefs (i.e., prediction errors) drove posterior bodily distortions after the illusion in both AN patients and healthy control participants. On the other hand, smaller or positive prediction error values (i.e., when participants had corrected prior bodily expectations) resulted in lower posterior bodily distortions for both AN patients and healthy control participants at Time 1, during the synchronous condition. These results suggest that prediction errors in bodily estimates were integrated coherently with the multisensory processes underlying the illusion. However, this pattern was disrupted at Time 2, where coherent integration of prediction error with the multisensory processes of the illusion was only observed in healthy control participants, while individuals suffering from AN did not show this coherent integration. This pattern is similar to the previously observed lack of coherent integration between interoceptive metacognition and ownership across multisensory processes during the illusion. Based on these findings, we may speculate that prediction error requires time to be internalized and may emerge in later stages of the pathology during chronicization processes (Brewerton & Dennis, 2016), thus effectively “locking” the patients in their prior overestimated (distorted) perception of their body without the ability to reduce their overestimation by coherently integrating bottom-up information (Riva & Gaudio, 2012; Riva, Gaudio et al., 2015, Riva & Dakanalis, 2018; Riva & Gaudio, 2018).
In conclusion, our results showed the crucial role of interoceptive metacognition in embodiment and bodily perceptive distortions. Interoceptive metacognition seems to function differently in individuals suffering from Anorexia Nervosa compared to healthy control participants. While in healthy control participants, interoceptive metacognition is coherently merged into multisensory integration processes and higher levels are linked to lower bodily perception distortions, this is not the case for individuals suffering from AN. During the acute symptomatological phase, AN patients’ interoceptive metacognitive belief seems to override multisensory integration processes and was positively related to bodily perception distortions. This suggests that AN patients prioritize top-down metacognitive beliefs about the body, disregarding bottom-up bodily perceptions and their multisensory integration. These pathological patterns were partially recovered after a 12-week rehabilitative program suggesting that – at least in early pathological phases – AN bodily perception deficits still exhibit a degree of plasticity and can be recovered. From a Bayesian perspective, prediction errors regarding bodily estimation drove posterior bodily perceptive distortions both in patients suffering from AN and healthy control participants. However, while healthy participants coherently merged these prediction errors with multisensory integration processes, patients suffering from AN failed to do so, suggesting that the progression of the disease compromised the ability of the patients to coherently integrate their prior expectations with multisensory bottom-up information, possibly locking their perception in a distorted prior top-down belief.
LimitationsMeasuring interoception is an extremely challenging task, and the scientific community is currently working on improving both procedures and theoretical frameworks to address the ontological problem of measuring inner bodily perceptions (Quigley et al., 2021).
From this point of view, the first limitation of the current study is the use of the HCT as a measure of cardiac interoceptive perception. The heartbeat counting task (HCT), originally developed by Schandry (1981), has been thoroughly used in interoceptive literature so far and, albeit several kinds of interoceptive accuracy do exist - e.g., respiratory, gastric, etc. (Garfinkel et al., 2016; van Dyck et al., 2016; Ferentzi et al., 2018), cardiac interoceptive accuracy remained the most diffused interoceptive measure even in recent literature with clinical and healthy populations (DeVille et al., 2021; Haruki & Ogawa, 2021; Manzoor et al., 2021; Moccia et al., 2021; Terasawa et al., 2021; Vig et al., 2021; Ferentzi et al., 2022). Notwithstanding, HCT validity has been recently questioned based on the argument that it is influenced by factors that are not an inherent part of the interoceptive domain. Specifically, the HCT has been criticised and it is currently at the centre of a dispute as several methodological limitations have been highlighted in the original task, such as the influence of top-down processes (Körmendi et al., 2021), time estimation mechanisms, and prior beliefs regarding the heartbeat rate (Desmedt et al., 2018; Desmedt et al., 2020). On the other hand, the HCT has been repeatedly validated (Ainley et al., 2020) and recent literature supported its convergent construct validity (Schulz et al., 2021). Albeit the dispute is still ongoing, authors partially converged on the notion that a strict set of instructions Desmedt et al. (2020) might improve HCT reliability. Following these recent suggestions (Ferentzi et al., 2022), we adopted the set of strict instructions (i.e., by encouraging to count felt heartbeats only and to report zero if no sensations were detected) to improve the reliability of the HCT task used in this study. Notwithstanding, the interpretation of the results should consider the intrinsic bias of the task from the perspective of the current interoceptive debate (Desmedt et al., 2022). In this regard, future studies could rely on more appropriate and solid measures of interoceptive perceptions (Ferentzi et al., 2022). As of today, several of these measures are being developed, however, they still need extensive validation.
In the second instance, future studies that rely on visuotactile stimulation could use wearable mechanical devices to standardize the synchronous and asynchronous stimulation, limiting the bias due to the procedure administered by the researcher.
Implications for treatment and future directionsThe results just discussed suggest that prior metacognitive beliefs and bodily prediction errors play a relevant role in the clinical symptomatological condition of patients suffering from AN, leading to the question of how it is possible to modify the precision of prior beliefs and/or sensory data of this clinical population. Several approaches offer insight into an effective pathway to modify prior belief and sensory processing. To briefly summarize, biological psychiatry suggests that pharmacological medications could play a relevant role in predictive and active inference processes. Different authors (Iglesias et al., 2013; Auksztulewicz & Friston, 2016) suggested that conventional neuromodulators including acetylcholine (ACh), serotonin and dopamine, and N-methyl-d-aspartate (NMDA) are involved in synaptic gain control mechanisms and therefore play a critical role in prediction error signaling. For example, a recent experimental study (Haarsma et al., 2021) demonstrated that dopamine plays a key role in the mechanisms underlying the precision weighting of unsigned prediction errors (the prediction errors that signal surprise). On the opposite side, psychotherapeutic frameworks imply a relevant role of cognition and environment in prior beliefs generation and updating. Both the Maudsley Anorexia Nervosa Treatment for Adults (MANTRA) and the Cognitive Behavior Therapy-Enhanced (CBT-E), two of the most effective psychological treatments of AN (Jansingh et al., 2020), share different techniques that may influence the precision of both prior beliefs and sensory data. The first technique called “correcting thinking styles”, involves identifying thinking styles (perpetuating cognitive models in AN), and alternative thinking styles. In the predictive coding framework, this technique should reduce the precision of beliefs about one's agency and capacity for control. A second technique is the “body image module”, which involves identifying overvaluation/overestimation processes and their consequences, enhancing the importance of other self-evaluation domains and reducing the importance of shape and weight. Again, in the predictive coding framework, this technique should reduce the top-down influence of prior bodily beliefs, increasing the bottom-up influences of “raw” sensations coming from the physical body. Nevertheless, both psychiatry and psychotherapy techniques do not directly modify the maladaptive prior beliefs but rather some of the variables that may influence their updating. As both frameworks also require that the intervention – pharmacological or psychotherapeutic – is followed by the new learning of a preferred behaviour different from the maladaptive one, i.e., counteractive learning. Unfortunately, this process creates a secondary belief (new behaviour) that competes with the existing maladaptive one, with the risk of relapse and/or a limited degree of symptom relief (Ecker & Vaz, 2022). As noted by different authors (Langkaas et al., 2018; Ecker & Vaz, 2022) mild, partial, incremental change has been the typical outcome in psychiatry and psychotherapy, both in general and in the treatment of AN (Zeeck et al., 2018).
To overcome these problems, we recently suggested a new therapeutical approach – regenerative virtual therapy (RVT) – that uses technology-based somatic modification techniques to restructure the maladaptive priors behind a pathological condition (Riva et al., 2019; Serino et al., 2020; Fernandez-Alvarez et al., 2021; Riva et al., 2021). The main goal of RVT is to allow a potential revision and de-weighting of maladaptive prior beliefs (Riva et al., 2017) through the integration of different technology-based somatic modification techniques with mindfulness and cognitive reappraisal. Specifically, RVT is based on the following steps:
- 1.
The creation of a synthetic full-body illusion in virtual reality that is synchronized with an interoceptive modulation, to update prior bodily beliefs.
- 2.
The use of brain stimulation techniques to lessen the impact of predictions errors made from the top-down distorted prior beliefs,
- 3.
The application of awareness techniques to increase the accuracy of the multisensory experience to foster bottom-up input integration.
- 4.
The re-elaboration of the emotional content of the overall multisensory experience to increase its level of reward using cognitive reappraisal.
Differently from the methods discussed before, RVT aims at directly targeting the pathological priors connected to the clinical condition, generating a transformational change (Riva et al., 2016; Langkaas et al., 2018) that modifies longstanding symptoms and the altered state of emotional activation associated to it. RVT is still a new perspective method based on the principles of computational neuroscience that need further validation. In this regard, future studies and clinical trials are required for considering RVT as a possible alternative to the methods used by psychiatry and psychotherapy.
ConclusionsAs underlined by Zeeck et al. (2018): “Although progress has been made in the understanding of psychosocial and biological mechanisms [of AN] that are responsible for the development of the illness and its maintenance, there is still an urgent need to optimize treatment approaches and demonstrate their efficacy.” In this paper, we have suggested that the emergence of a new neuroscience paradigm – predictive coding accounts of mental diseases – and its related research area – clinical computational neuroscience – may provide new insights for improving AN treatment.
Computational neuroscience has two critical advantages that are reflected in this paper (Smith et al., 2021): (i) it allows the development of mathematical models that enable researchers to simulate neurocomputational processes - to confirm how the brain works, and (ii) it allows the making of empirical predictions for testing which neurocomputational processes the brain uses. Using this approach, we found that in patients suffering from AN, actual bodily perceptions (both interoceptive and proprioceptive – as the ones needed for the body measure estimation task) have less relevance in the processes related to virtual reality embodiment and real bodily estimations. This enforces the idea that patients suffering from AN might disregard afferent (bottom-up) interoceptive and proprioceptive bodily inputs in favour of distorted metacognitive beliefs or altered prior expectations (prediction errors) regarding their body, where these distorted metacognitive beliefs and prediction errors drive both their ability to embody a virtual avatar and their distortions in perceiving their own body.
Unfortunately, existing treatments only partially target these issues. Given the promising new research avenues that were inspired by earlier predictive coding accounts of mental diseases (Smith et al., 2021, Liddle & Liddle, 2022, Putica et al., 2022), we think this perspective can also offer unique insights and study into the understanding of mechanisms of AN and into providing better treatment options.
Author contributionsConceiving: D.D.L., S.S.; Methodology: D.D.L., S.S., Data Collection: S.S., C.C., Data Analysis: C.T., Manuscript first draft: D.D.L., S.S., C.T.; Manuscript revision: D.D.L., S.S., C.T., C.C., N.P., G.R., Supervision: N.P., G.R.
FundingResearch funded by the Italian Ministry of Health (POSTECH).