Edited by: Andre R Brunoni, Marie-Anne Vanderhasselt, Leigh Chavert
More infoLow intensity transcranial electrical stimulation (tES) and meditation are two promising, yet variable, non-pharmacological interventions. Growing research is investigating combined effects of both techniques on one's cognitive, emotional, and physical health.
ObjectiveThis article reviews the current research that combines tES and meditation interventions in healthy and diseased participants. The review considers the intervention parameters and their effects in a well-organized manner.
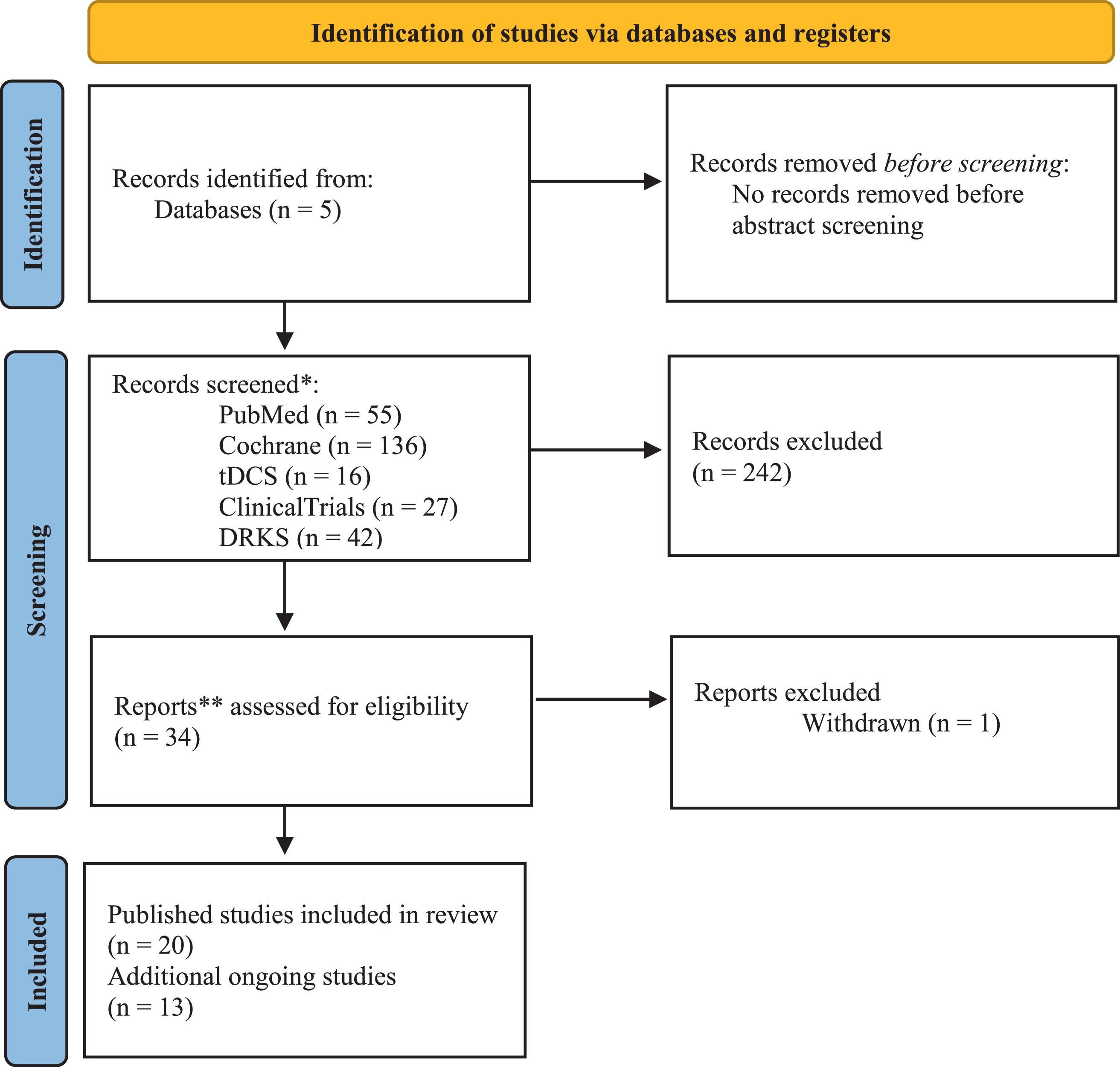
MethodA systematic search for clinical and experimental published studies was conducted in the PubMed, Cochrane, and transcranial direct current stimulation (tDCS) databases using common keywords for tES and for meditation techniques well defined by previous studies. Unpublished ongoing studies were identified with the ClinicalTrials.gov and DRKS.de clinical trial websites.
Results20 published studies and 13 ongoing studies were included for qualitative analysis. 13 published articles studied patients with chronic pain, psychological disorders, cognitive impairment, and movement disorders. Anodal tDCS was the only tES technique while mindfulness meditation was the most common meditation type. Eight studies had a main group effect, with outcome improvement in the active combined intervention. However, most published studies showed improvements after at least one combined intervention with variable effects.
ConclusionPairing anodal tDCS with meditation shows promising improvements of the physical, mental, and emotional aspects of daily life. Further studies are required to confirm the relevance of this combination in the clinic.
The prevalence for using non-pharmacological interventions in the treatment of diseases is high. This is strongly related to the potential that these interventions have on treating non-curable diseases and conditions in a less invasive and more suitable way (Herguedas, 2021; Lefaucheur et al., 2017; Terranova et al., 2019). Two such interventions are meditation and non-invasive brain stimulation.
Meditation finds its roots in most spiritual traditions of the world, especially Hinduism and Buddhism (Matko & Sedlmeier, 2019). Meditation is defined as a mind-body practice, which comprises at least one of many intentional awareness activities, such as observation, focus, release, production, imagination, and movement, which are reinforced and unified by meta-awareness in an informal or formal setting (Sparby & Sacchet, 2022). Meditation practice might lead to altered states of consciousness, scaling through different stages of development and finally end goals of the practice such as ‘awakening’ (Nash et al., 2013; Reddy & Roy, 2019). These meditation experiences, stages, and states may be explained within spiritual or secular frameworks (Sparby & Sacchet, 2022). A systematic review by Ospina et al. (2007) classifies the different types of meditation practices to five broad categories: 1) mindfulness meditation (Tang et al., 2015), 2) Yoga (Varambally & Gangadhar, 2016), 3) Tai Chi (Wayne & Kaptchuk, 2008), 4) mantra meditation (Lynch et al., 2018) and 5) Qi Gong (Feng et al., 2020) . Two further commonly used meditation techniques are loving kindness (Hofmann et al., 2011) and compassion meditation, and non-dual meditation (Dahl et al., 2015; Brandmeyer et al., 2019).
In a secular world, meditation offers multiple possibilities to improve symptoms, reduce pain and develop better disease coping and management strategies ranging from psychiatric disorders (Wielgosz et al., 2019) to chronic pain Hilton et al. (2016); Zeidan and Vago (2016) and even eye diseases, such as glaucoma (Dada et al., 2019). The benefits of meditation have been shown in different age groups of patients, ranging from children and adolescents to older adults (Nanthakumar, 2018; Perry-Parrish et al., 2016; Simkin & Black, 2014). Over the decades, meditation, especially mindfulness meditation (MM), has become a very popular method to reduce stress, develop resilience, and promote health and well-being (Huberty et al., 2019; Lemay et al., 2019; Zollars et al., 2019). Many studies implement a sham meditation group as a control group. The most commonly studied and used sham protocol for mindfulness meditation involves guided breathing exercises without any guidance on how to regulate breath or body awareness to control for relaxation and expectation effects. The body position, duration and eye state kept the same as experimental condition (Zeidan et al., 2010; Ahn et al., 2019; Noone & Hogan, 2018). In addition, sham yoga includes basic muscle stretching exercises (Sabina et al., 2005) while sham Qi Gong involves series of mild body movements without meditation and deep breathing guidance (Moon et al., 2020).
The exact mechanisms underlying the practice of meditation is still elusive, with different meditation types having different psychophysiological effects on the practitioner (Brandmeyer et al., 2019). It has been suggested that contemplative practices might improve well-being by modulating maladaptive self-referential thought patterns (Dahl et al., 2015). The practice of meditation including mindfulness may further lead to emotional regulation by bolstering prefrontal cognitive control enhanced amygdala top-down control (Bandmeyer et al., 2019). With most of the contemplative research focusing on mindfulness meditation, it has been proposed that this meditation type exerts its effects via improved self-regulation through enhanced self-awareness, attentional control and emotional regulation (Tang et al., 2015).
On the other hand, low intensity transcranial electric stimulation (tES) techniques are neurophysiological techniques used in both clinical practice and research for safe, effective, and non-invasive brain stimulation in humans (Nitsche & Paulus, 2011; Paulus, 2011). tES intends to directly alter brain function through passing weak currents (<4 mA) through at least two electrodes placed on the scalp (Antal et al., 2017). Two commonly used tES methods include transcranial direct current stimulation (tDCS) and transcranial alternating current stimulation (tACS), which includes transcranial random noise stimulation (tRNS). tDCS is the most frequently used method, it comprises the application of a weak direct current to the scalp (1–2 mA) delivered via at least two electrodes (Brunoni et al., 2011). This leads to a subthreshold change in the neuronal resting membrane potential by modulating the probability with which a neuron fires an action potential in response to input from another neuron (Antal & Herrmann, 2016; Bindman et al., 1964; Creutzfeldt et al., 1962). tDCS can lead to changes in brain activity at both local and network levels (Opitz et al., 2016; Paulus et al., 2012). Repeated tDCS can lead to long lasting changes in cortical excitability through long-term potentiation-like or depression-like mechanisms, which underlie associated behavioral effects (Stagg et al., 2009, 2018). The net effects of the tDCS depends on multiple factors such as polarity, intensity, and duration of the stimulation, the state of the brain, and what the participant is doing during the session, among others (Fregni et al., 2020). Clinical application of repeated tDCS reveals potential therapeutic effects in epilepsy, chronic pain, unipolar depression and stroke (Fregni et al., 2020; Lefaucheur et al., 2017). Furthermore, healthy elderly people demonstrated improved cognitive performance such as different types of memory and learning following a single or consecutive repeated tDCS sessions (Prehn & Flöel, 2015; Siegert at al., 2021). Meanwhile, tACS, including tRNS, is effective at modulating the amplitude, frequency and phase of brain oscillations which leads to behavioral effects (Antal et al., 2022). Recent tACS research has shown potential therapeutic effects on cognitive outcomes in psychiatric and neurodegenerative conditions. (Al Qasem et al., 2022).
Over the years, there has been a growing interest in the development and application of novel and low-cost non-pharmacological therapies to prevent and treat diseases in the clinic or to improve quality of life in non-patient groups. Both meditation and tES have individually shown their ability to relieve symptoms, predominantly in the short term but also long-term. They are also attractive for the low cost and the possibility of home-based intervention when proper training is provided (Herguedas, 2021; Terranova et al., 2019). However, there are also limitations for each strategy. For example, it can be difficult to control whether someone is properly meditating and to see its effects without significant training (Badran et al., 2017). Meanwhile, tES can vary drastically depending on the stimulation parameters, such as intensity, duration, montage, and number of sessions performed, which the latter influences the effects after the stimulation (Bikson et al., 2019). For both techniques, the subject's current emotional and physical state can also influence the efficacy of the intervention (Fregni et al., 2020).
It has been recently hypothesized that these techniques may provide greater feasibility and efficacy when combined, either simultaneously or subsequently. Currently, there are no systematic reviews for such a topic available. Therefore, this review aims to systematically organize, analyze, and compare the overall effects of studies that implement combined tES and meditation interventions in both patients and healthy individuals, with consideration of the parameters of each technique and their influence on each other. In order to assess the effectiveness of tDCS protocols in combination with meditation, we consider outcomes in healthy individuals and patients separately in the results sections. We also consider clinical and experimental studies irrespective of indication for tES and meditation. We aim to provide an overview of successes and drawbacks of combining these two non-pharmacological methods, either in a concurrent or consequent manner in research. This review also illustrates the variability in both meditation parameters (type, duration) and tDCS parameters (duration, intensity, stimulation site) and their indications for use. Moreover, we also summarize the ongoing clinical studies in this review to demonstrate the current scientific interest in combining tES and meditation in clinical populations, with respect to disease condition, type of tDCS protocol and meditation type.
MethodsDatabasesIn September 2022, a literature database search for published studies involving both tES and meditation techniques was conducted in the PubMed, tDCS database, Cochrane Library databases. PubMed was primarily used due to its easy navigation and high number of available studies to collect a large amount published studies (U.S. National Library of Medicine n.d.). Meanwhile, the Cochrane Library and tDCS Database were used to find additional studies that were not included in the initial PubMed searches (John Wiley & Sons, Inc, n.d.; TDCS database, n.d.). On the other hand, the tDCS Database (Grossman et al., 2018) was used to search additional studies that were not present in the previous searches that involved tDCS specifically. In addition to published studies, a search for ongoing clinical studies was conducted in Cochrane, ClinicalTrials.gov (NIH U.S. National Library of Medicine, n.d.), and the Deutsches Register Klinischer Studien (DRKS, n.d.; German Clinical Trials Register) databases. The same keywords were used for all databases.
Keyword searchThe database search was first done in PubMed, then Cochrane, tDCS database, ClinicalTrials.gov and DRKS. For all appropriate keyword searches, see Supplementary Materials Table 1. All abstracts were screened for relevance. For the ongoing studies that were listed as completed, but without study data posted, the registration code was searched on Google to determine if the study was published. The following terms were used for the tES intervention: “transcranial electrical stimulation”, "transcranial direct current stimulation", “tdcs”, "transcranial alternating current stimulation", “tacs”, “transcranial random noise stimulation”, and “trns”. Meanwhile, the following terms were used for meditation techniques: “meditation”, “mindfulness”, “mindful”, “mantra”, “yoga”, “taichi/tai chi”, “qigong/qi gong”, “mindfulness based stress reduction", “breathing exercises", “non dual”, “transcendental” and “loving kindness”. These meditation keywords were chosen based on the five broad categories of meditation defined by Ospina et al. (2007), and the various meditation techniques listed by Brandmeyer et al. (2019). Supplementary Materials Table 1 describes the search process and the search results for each appropriate database.
Study design, population, intervention characteristics, and database(s) of which it was found of the selected published studies. For the participants, the listed items are in the following order: N = # total subjects analyzed, # of female/male, age [mean ± SD], condition, n = # of subjects in the active and combined group. Witkiewitz et al. (2019), Brown et al. (2020), and Gibson et al. (2022) all used the same participants for different experiments. In addition, Ahn et al. (2019) and Pollonini et al. (2020) also used the same participants with different analyses. The * on “mean ± SD” number represents those studies that did not include an overall mean ± SD for all subjects combined, and instead was calculated by taking the averages of the means and SD across the included groups. The ** represents the total number of subjects in both active and combined groups. The *** represents the subjects that were dropped from the previous analysis. The intervention column uses “Arm” for cross over studies and “Group” for parallel studies. If not at the same time, the timing of the meditation + tES technique is stated in the parentheses following the condition. Those that have **** mean that the intervention order and type was not clearly stated. The following acronyms are used: tDCS = transcranial direct current stimulation, MM = mindfulness meditation, LKM = loving kindness meditation, MBCT = mindfulness based cognitive training, MBRP = mindfulness-based relapse prevention, MBSAT = mindfulness-based substance abuse treatment, MBSR = mindfulness based stress reduction. For sham meditation techniques type, see Table 3 and 4, and for definitions, see Supplementary Materials Table 2.
| Study | Study design | Participants | Dropouts | Intervention | Database (s) |
|---|---|---|---|---|---|
| Badran et al. (2017) | Randomized, sham-controlled, double-blind, cross over, clinical, pilot | N = 15, 7/8, 28.2 ± 6.2, healthy, n = 15 | Notstated | Arm 1: real MM & active tDCS (1 mA);Arm 2: real MM & active tDCS (2 mA);Arm 3: real MM & sham tDCS; | PubMedCochranetDCS Database ClinicalTrials.gov |
| Hunter et al. (2018) | Randomized, double-blind, parallel | N = 29, 11/18, 27.5 ± 5.45*, healthy, n = 16 | 4 | Group 1: real MM & active tDCS;Group 2: sham MM & sham tDCS; | PubMedCochrane |
| Ahn et al. (2019) | Randomized, sham-controlled, double-blind, single center, parallel, clinical, pilot | N = 30, 18/12, 59.47 ± 6.91, knee osteoarthritis in older adults, n = 15 | 8 | Group 1: real MM & active home-based tDCS;Group 2: sham MM & sham home-based tDCS; | PubMedCochrane ClinicalTrials.gov |
| Hung (2019) | Randomized, sham-controlled, parallel, clinical, pilot | N = 26, 18/8, 47.85 ± 10.51, treatment resistant unipolar depression, n = 8 | Notstated | Group 1: mindfulness training**** & active tDCS;Group 2: active tDCS only;Group 3: sham tDCS only; | PubMedCochrane |
| Monnart et al. (2019) | Randomized, controlled, parallel, clinical, pilot | N = 31, 20/11, 50.16 ± 6.73*, treatment-resistant depressed patients, n = 15 | 15 | Group 1: real MBCT (2nd) & active tDCS (1st);Group 2: sham MBCT (2nd) & active tDCS (1st); | PubMedCochrane |
| Robinson et al. (2019) | Randomized, sham-controlled, double-blind, parallel, pilot | N = 87, 63/24, 20.16 ± 4.34, healthy college students, n = 26** | 4 | Group 1: real LKM & active tDCS (2 mA, F3);Group 2: real LKM & active tDCS (2 mA, CP6);Group 3: real LKM & sham tDCS (0.1 mA, F3);Group 4: real LKM & sham tDCS (0.1 mA, CP6);Group 5: sham LKM & active tDCS (2 mA, F3);Group 6: sham LKM & active tDCS (2 mA, CP6);Group 7: sham LKM & sham tDCS (0.1 mA, F3);Group 8: sham LKM & sham tDCS (0.1 mA, CP6); | PubMedCochranetDCS Database |
| Witkiewitz et al. (2019) | Randomized, sham-controlled, double-blind, parallel, clinical | N = 84, 34/50, 52.27 ± 13.00, older adults with alcohol use disorder, n = 47 | Notstated | Group 1: real MBRP & active tDCS;Group 2: real MBRP & sham tDCS; | PubMedCochrane |
| Clarke et al. (2020) | Randomized, sham-controlled, single blind, parallel | N = 97, 75/22, 22.12 ± 5.51*, healthy young adults, n = 25 | 2 | Group 1: real MM & active tDCS;Group 2: real MM & sham tDCS;Group 3: sham MM & active tDCS;Group 4: sham MM & sham tDCS; | PubMedCochrane |
| Brown et al. (2020) | Randomized, sham-controlled, double-blind, parallel, clinical, secondary analysis of Witkiewitz et al. (2019) | N = 68, 32/36, 52.16 ± 13.6, older adults with alcohol use disorder, n = 36 | 16 | Group 1: real MBRP & active tDCS;Group 2: real MBRP & sham tDCS; | PubMedCochrane |
| Pollonini et al. (2020) | Randomized, sham-controlled, double-blind, clinical, pilot study, secondary analysis of Ahn et al. (2019) | N = 19, 10/9, 60 ± 7.7, knee osteoarthritis in older adults, n = 11 | 11*** | Group 1: real MM & active tDCS;Group 2: sham MM & sham tDCS; | PubMedCochrane |
| Alizadehgoradel et al. (2021) | Randomized, sham-controlled, single-blind, parallel, clinical | N = 64, 0/64, 19.46 ± 1.15, youths with methamphetamine addictions, n = 17 | 16 | Group 1: real MBSAT (2nd) & active tDCS (1st);Group 2: active tDCS only;Group 3: real MBSAT only;Group 4: sham tDCS only; | PubMedCochrane |
| Brooks et al. (2021) | Randomized, sham-controlled, double-blind, two site parallel, clinical, pilot study | N = 26, 12/14, 68.65 ± 5.45*, cognitive complaints and symptoms of depression/anxiety in older adults, n = 12 | 9 | Group 1: real MBSR & active tDCS;Group 2: real MBSR & sham tDCS; | PubMedCochrane ClinicalTrials.gov |
| Danilewitz et al. (2021) | Randomized, sham-controlled, double-blind, cross over | N = 22, 14/8, 29.05 ± 4.56, healthy, n = 22 | 2 | Arm 1: real yoga (2nd) & active tDCS (1st);Arm 2: real yoga (2nd) & sham tDCS (1st); | PubMedCochrane |
| Liao et al. (2021) | Randomized, sham-controlled, double-blind, parallel, clinical | N = 20, 13/7, 72.85 ± 4.35*, older adults with mild cognitive impairments, n = 10 | 1 | Group 1: real tai chi & active tDCS;Group 2: real tai chi & sham tDCS; | PubMedCochrane |
| Nishida et al. (2021) | Randomized, sham-controlled, double-blind, parallel, clinical | N = 56, 34/22, 39.80 ± 10.06, healthy to subclinical, n = 27 | 2 | Group 1: real TW-FM (MM) & active tDCS;Group 2: real TW-FM (MM) & sham tDCS; | PubMedCochrane |
| Park et al. (2021) | Randomized, sham-controlled, double-blind, cross over | N = 5, 2/3, 52 ± 4, clinically definite functional movementdisorder, n = 5 | Notstated | Arm 1: real yoga (2nd) & active tDCS (1st);Arm 2: real yoga (2nd) & sham tDCS (1st); | PubMedCochrane |
| Pimenta et al. (2021) | Randomized, sham-controlled, double-blind, parallel, clinical, pilot | N = 24, 24/0, 32.91 ± 9.96*, females with chronic migraine, n = 12 | 7 | Group 1: real MM & active tDCS;Group 2: real MM & sham tDCS; | PubMedCochrane |
| Gibson et al. (2022) | Randomized, sham-controlled, double-blind, parallel, clinical, secondary analysis of Witkiewitz et al. (2019) | N = 84, 34/50, 52.27 ± 13.00, older adults with alcohol use disorder, n = 47 | Notstated | Group 1: real MBRP & active tDCS;Group 2: real MBRP & sham tDCS; | PubMedCochrane ClinicalTrials.gov |
| Ramasawmy et al. (2022) | Randomized, sham-controlled, placebo-controlled, double-blind, parallel, clinical, pilot | N = 30, 28/2, 53.60 ± 9.48,adults with fibromyalgia syndrome, n = 10 | 6 | Group 1: real MM & active tDCS;Group 2: real MM & sham tDCS;Group 3: no intervention; | CochraneDRKS.de |
| Sefat et al. (2022) | Randomized, sham-controlled, double-blind, cross over | N = 18, 5/13, 27.04 ± 4.51, healthy, n = 18 | 4 | Arm 1: real yoga (1st) & active tDCS (2nd);Arm 2: real yoga (1st) & sham tDCS (2nd); | PubMedCochrane |
The process of identifying, screening, and assessing for eligibility of studies is summarized in a PRISMA flow diagram (Fig. 1). Studies were included if they met the following criteria: 1) included at least one arm of intervention where there was combination of tES (tDCS, tACS, or tRNS) and one of the following meditation types, such as mindfulness meditation, mantra meditation, yoga, tai chi, qigong, non-dual meditation, transcendental meditation, loving kindness meditation or meditation involving breathing exercises, 2) randomized design, and 3) human participants, part of either healthy or clinical groups.
Studies were excluded if they: 1) contained transcranial magnetic stimulation (TMS), transcutaneous electrical stimulation, cranial electrical stimulation, neuro- or bio-feedback, theory of mind therapy, physical therapy, behavioral therapy, electroacupuncture, and/or motor/guided imagery as an intervention, 2) were designed as a review or meta-analysis, 3) were not completed or accessible (i.e. abstracts only, poster abstract, no abstract or complete paper available, or not able to be translated) and/or 4) were designed as a case study. The blinding status of the studies was not an exclusion factor.
AnalysisStudies were first given priority of review if they had healthy participants or patients. Then, the studies were selected for analysis if they included an arm of intervention where tES and a form of meditation were applied at the same time or in a sequential manner. Finally, these studies were analyzed and discussed based on the efficacy of the combination of the two techniques.
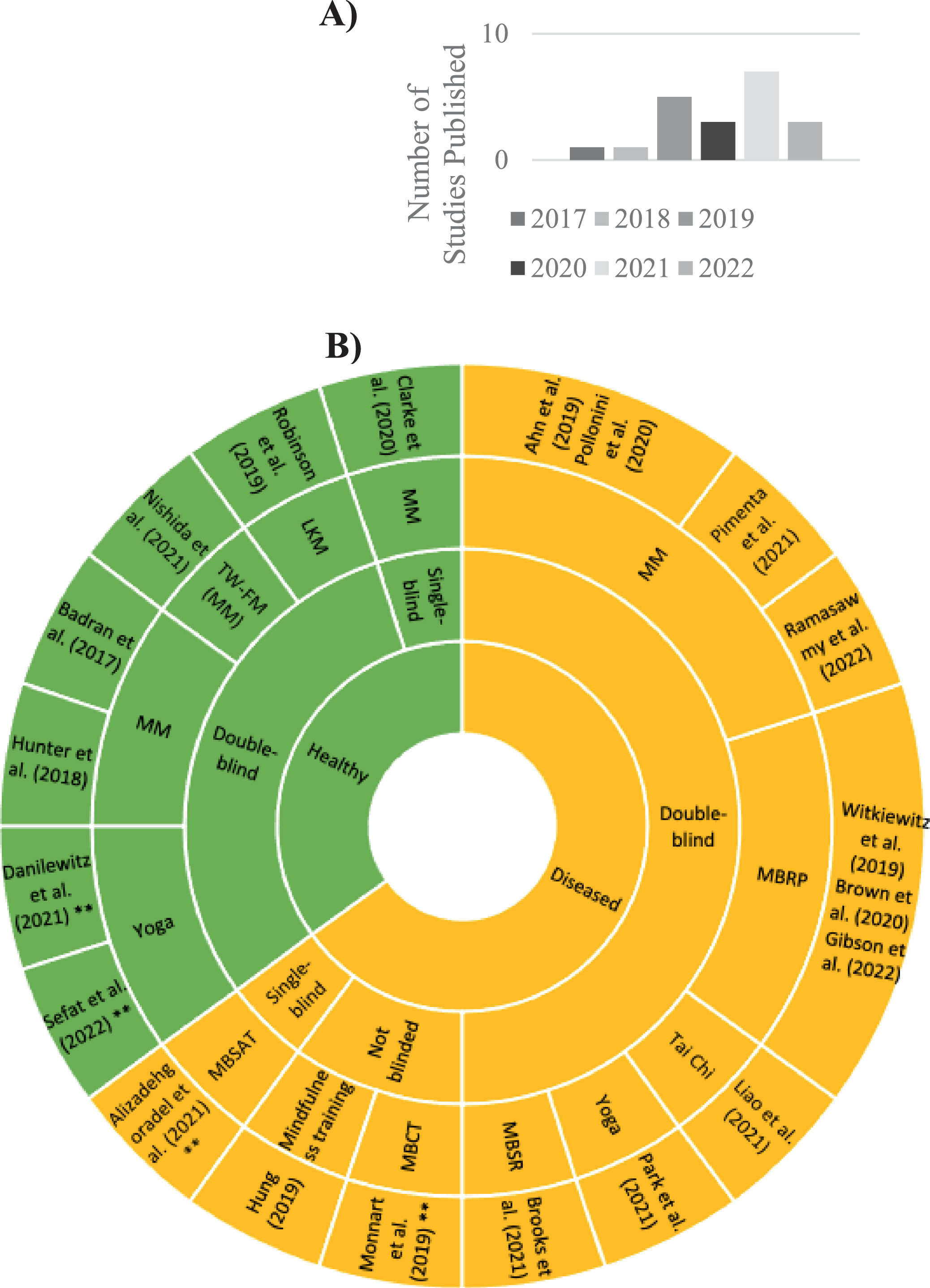
ResultsStudy designOut of the 276 studies searched, 20 studies published between 2017 and 2022 (Fig. 2A) and 13 ongoing studies met all inclusion criteria. All the included studies, whether published or ongoing, included tDCS as the tES technique and no studies were or are being performed with tACS or tRNS (Table 1 & 2). Out of the published articles, there were only 17 unique studies as Brown et al. (2020) and Gibson et al. (2022) were secondary analyses for Witkiewitz et al. (2019), and Pollonini et al. (2020) was the secondary analysis of the Ahn et al. (2019) study. The published studies included 664 participants, after correcting for secondary analyses publications using the same participants, comprising of 56.93% females and 43.07% males (Table 1). Seven out of the 20 studies were conducted in healthy individuals (Badran et al., 2017; Clarke et al., 2020; Danilewitz et al., 2021; Hunter et al., 2018; Nishida et al., 2021; Robinson et al., 2019; Sefat et al., 2022), while the remaining studies tested the combination of tDCS and meditation in patient groups diagnosed with conditions such as chronic pain (Ahn et al., 2019;Pimenta et al., 2021; Pollonini et al., 2020; Ramasawmy et al., 2022), psychological disorders (Alizadehgoradel et al., 2021; Brooks et al., 2021; Brown et al., 2020; Gibson et al., 2022; Hung, 2019; Monnart et al., 2019; Witkiewitz et al., 2019), mild cognitive impairment (Liao et al., 2021), and movement disorders (Park et al., 2021). All the ongoing studies test the combined intervention in diseased populations (Table 2). For a list of the published and ongoing studies and their respective or anticipated study details (design, population/patient information, & intervention) and source information (title, authors, & year published/expected), see Tables 1 and 2, respectively.
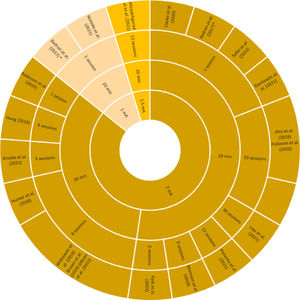
Characteristics of the published studies. A) Number of studies published according to year. B) Hierarchical representation the characteristics of the published studies. The order of significance from the inside-out is the condition of the participants, whether it is double-blinded, and the meditation technique. The outer most layer is the study itself. All studies included tDCS as the tES technique. MM = mindfulness meditation, MBCT = Mindfulness-Based Cognitive Therapy, MBRP = Mindfulness-Based Relapse Prevention, MBSAT = Mindfulness-Based Substance Abuse Treatment, MBSR = Mindfulness-Based Stress Reduction, TW-FM = Treadmill Walking with Focused Meditation. The * represents the studies that have a cross over design. The ** represents the studies where tES and meditation technique are not implemented concurrently.
Title, study design, population, intervention characteristics, and database(s) of which it was found of ongoing studies. For the participants, the listed items are in the following order: condition, age target, and expected enrollment (N). The − represents the ongoing studies that do not have a year of expected completion listed. For the meditation techniques specified, the following acronyms are used: MM = mindfulness meditation, MBCT = mindfulness based cognitive training, MBSR = mindfulness based stress reduction, BAT = Breathing and Attention Training. In addition, tDCS = transcranial direct current stimulation, DLPFC = dorsolateral prefrontal cortex, rTMS = repetitive transcranial magnetic stimulation.
Out of the seven published studies with healthy participants, one study (Clarke et al., 2020) had a double-blinded study design, where both the participants and the experimenters were blinded to the intervention (Table 1). In the patient groups, ten studies were double-blinded, while Alizadehgoradel et al. (2021) was single blinded and Monnart et al. (2019) and Hung (2019) were not blinded (Table 1, Fig. 2B). In addition, four studies had a cross over design, with all participants receiving both sham and real tDCS protocols (Badran et al., 2017; Danilewitz et al., 2021; Park et al., 2021; Sefat et al., 2022), while the remaining studies followed a parallel design (Table 1).
Meditation parametersThe most common type of meditation used mindfulness techniques (Mindfulness Meditation (MM)), accounting for 15 out of the 20 published studies (75%) and 12 out of the 13 ongoing studies (92%). Mindfulness was used in this review as an umbrella term for any intervention that included some aspect of MM. In this review, MM was used to describe an audio-guided mindfulness meditation while sitting (n = 6) or walking (n = 1). Treadmill walking focused meditation (TW-FM) is a type of MM practiced during walking. Some meditative interventions included psychoeducation aspects to it and other tasks, such as mindfulness-based stress reduction training (MBSR; n = 1), mindfulness-based relapse prevention (MBRP; n = 3), mindfulness-based substance abuse treatment (MBSAT; n = 1), mindfulness based cognitive therapy (MBCT; n = 1). Hung (2019) was the only study that lacked information on the nature of the mindfulness training. In the published studies, the rest of the studies used yoga (n = 3), tai chi (n = 1), and loving kindness meditation (LKM; n = 1) as meditation interventions (Table 3 & 4). As for the ongoing studies, one study is using a type of MM which is called breathing and attention training (BAT; Table 2). The technique, duration, number of sessions and timepoints in respect to tDCS is listed in Tables 3 & 4, where the tables differ according to their participant population information. The detailed description of the meditation technique used in each published study is summarized in Supplementary Materials Table 2.
Intervention parameters for selected published studies with healthy participants. Meditative characteristics and transcranial direct current stimulation (tDCS) parameters are listed according to each study. The * represents the studies with cross over designs. For the meditation techniques, the following acronyms are used: MM = mindfulness meditation, LKM = loving kindness meditation, TW-FM = treadmill walking with focused meditation. The positions of the electrodes are based on the standard 10–20 EEG system and the other locations are listed as: vlPFC = ventrolateral prefrontal cortex, IFG = inferior frontal gyrus, dlPFC = dorsolateral prefrontal cortex, tPJ = temporoparietal junction. The montage of the tDCS electrode is listed as anode first then cathode location. Concerning the electrode size, wherever the shape of the electrode was stated, it is written in parentheses. In the tDCS intensity column, the current density is inside parentheses. The ** represents the ramp information for the tDCS stimulation was not clearly stated in the study but implied to have occurred due to specification of sham ramping method and therefore, the details of the ramp are elaborated on.
| Study | Meditation Characteristics | tDCS Parameters | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Technique | Duration | No. of sessions | Timepoint | Montage | Size of electrode | tDCS Duration | Intensity | Sham conditions | No. of sessions | Timepoint | |
| Badran et al. (2017)* | MM | 20 min | 3 (2) | Each condition only once a week separated by a week;Same time as tDCS; | -F8 (right vlPFC);-Left supraorbital; | 25 cm2 | 20 min;No ramp stated; | 1 mAor 2 mA | Yes;No intensity stated;No ramp stated; | 3 (2) | Each condition only once a week separated by a week;Same time as meditation; |
| Hunter et al. (2018) | MM | 30 min | 20 (8) | Once every weekday for four weeks;Same time as tDCS for two of the weekdays;Immediately after baseline EEG; | -F10 (right IFG);-Left upper arm; | 11 cm2 | 30 min;No ramp stated; | 2 mA | Yes;0.1 mA;No ramp stated; | 8 | Two nonconsecutive days a week for four weeks;Same time as training; |
| Robinson et al. (2019) | LKM and relaxing podcasts (sham LKM) | 30 min | 1 | Same time as tDCS; | -F3 (left dlPFC)or CP6 (right tPJ);-Contralateral tricep; | 25 cm2 | 30 minNo ramp stated | 2 mA | Yes;0.1 mA;No ramp stated; | 1 | Same time as meditation; |
| Clarke et al. (2020) | MM and Mind-wandering (sham MM) | 14 min | 1 | Same time as tDCS; | -F3 (left dlPFC);-Left superior trapezius muscle (reference); | 30 cm2 | 20 min;30 s ramp up at the beginning and 30 s ramp down at the end | 2 mA(0.07 mA/cm2) | Yes;0 and 1.0 mA;30 s ramp to 1 mA for 1 min at beginning with 30 second ramp down to 0 mA for the remaining 18 min | 1 | Same time as meditation/mind-wandering; |
| Danilewitz et al. (2021)* | Traditional Hatha Yoga | 40 min | 2 (1) | Once a week for two weeks;Immediately after tDCS; | -F3 (left dlPFC);-F4 (right dlPFC); | 35 cm2 | 20 min;30 s ramp up at the beginning and 30 s ramp down at the end; | 2 mA(0.08 mA/cm2) | Yes;0 and 2 mA;30 s ramp up to 2 mA and immediate 30 s ramp down to 0 mA for the remaining time; | 2 (1) | Each condition only once a week separated by a week;Immediately before Yoga; |
| Nishida et al. (2021) | MM:TW-FM | 20 min | 1 | Same time as tDCS;Encouraged to engage in walking mindfulness for 1 week; | -F5 (left dlPFC);-Left shoulder; | 35 cm2(circular) | 20 min;30 s ramp up at the beginning and 30 s ramp down at the end; | 1 mA | Yes;0 and 1 mA;Description of sham protocol is not clear; | 1 | Same time as meditation; |
| Sefat et al. (2022)* | Hatha yoga | 40 min | 2 (1) | Once a week for 2 weeks;Immediately before tDCS; | -F3 (dlPFC);-F4 (right dlPFC); | 25 cm2 | 20 min;No ramp stated**; | 2 mA(0.08 mA/cm2) | Yes;0 and 2 mA;30 s ramp up to 2 mA and then 30 s ramp down to 0 mA for the remaining time; | 2 (1) | Each condition only once separated by a week;Immediately after yoga; |
Intervention parameters for selected published studies with diseased participants. Meditative characteristics and transcranial direct current stimulation (tDCS) parameters are listed according to each study. The * represents the studies with cross over designs. For the meditation techniques, the following acronyms are used: MM = mindfulness meditation, MBCT = mindfulness based cognitive training, MBRP = mindfulness-based relapse prevention, MBSAT = mindfulness-based substance abuse treatment, MBSR = mindfulness based stress reduction. The positions of the electrodes are based on the standard 10–20 EEG system and the other locations are listed as: M1 = primary motor cortex, dlPFC = dorsolateral prefrontal cortex, IFG = inferior frontal gyrus, tPJ = temporoparietal junction. The montage of the tDCS electrode is listed as anode first then cathode location. Concerning the electrode size, wherever the shape of the electrode was stated, it is written in parentheses. In the tDCS intensity column, the current density is inside parentheses. The ** represents the ramp information for the tDCS stimulation was not clearly stated in the study but implied to have occurred due to specification of sham ramping method and therefore, the details of the ramp are elaborated on.
| Study | Meditation Characteristics | tDCS Parameters | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Technique | Duration | No. of sessions | Timepoint | Montage | Size of electrode | tDCS Duration | Intensity | Sham conditions | No. of sessions | Timepoint | |
| Ahn et al. (2019) | MM | 20 min | 10 | Once every weekday for two weeks;Same time as tDCS; | -M1 of the hemisphere contralateral to the affected knee;-Supraorbital region ipsilateral to the affected knee; | 35 cm2 | 20 min;10 s ramp up at the beginning and 10 s ramp down at the end; | 2 mA | Yes;0, 2, 0 mA;10 s ramp up to 30 s of 2 mA then 10 s ramp down at beginning only; | 10 | Once every weekday for two weeks;Same time as meditation; |
| Hung (2019) | Mindfulness training (lack of information about nature of training) | 1 hr | 6 | One session a week for six weeks;Same time as tDCS (timing not clearly stated); | -F3 (left dlPFC);-F4 (right dlPFC); | Notstated | 30 min;No ramp stated**; | 2 mA | Yes;0 and 2 mA;2 mA current only at beginning and end, duration of current(initial current and ramp not stated); | 12 (6) | Ten working days and then one day on the following 4th and 6th week;Same time as mindfulness training (timing not clearly stated); |
| Monnart et al. (2019) | MBCT and Jacobson Relaxation (sham MBCT) | 2 hr (30 min sham) | 9 | Eight consecutive days with one session two weeks later;Immediately following tDCS; | -F3 (left dlPFC);-F4 (right dlPFC); | 35 cm2 (rect-angular) | 20 min;15 s ramp up at the beginning and 15 s ramp down at the end; | 2 mA | No sham | 9 | Eight consecutive days with one session two weeks later;Immediately before MBCT/relaxation; |
| Witkiewitz et al. (2019) | MBRP | 2 hr | 8 | Once a week for eight weeks;First 30 mins of guided meditation practice at the same time as tDCS and the following 90 min of discussions of mindfulness; | -F10 (right IFG);-Left upper arm; | 15 cm2 | 30 min;30 s ramp up at the beginning and 30 s ramp down at the end; | 2 mA | Yes;0 and 2 mA;30 s ramp up to 2 mA then 30 s ramp down to 0 mA at the beginning and end;0 mA for 28 min; | 8 | Once a week for eight weeks;Rolling group sessions;Same time as guided meditation practice; |
| Brown et al. (2020) | MBRP | 2 hr | 8 | Once a week for eight weeks;First 30 mins of guided meditation practice at the same time as tDCS and the following 90 min of discussions of mindfulness; | -F10 (right IFG);-Left upper arm; | 15 cm2 | 30 min;30 s ramp up at the beginning and 30 s ramp down at the end; | 2 mA | Yes;0 and 2 mA;30 s ramp up to 2 mA then 30 s ramp down to 0 mA at the beginning and end;0 mA for 28 min; | 8 | Once a week for eight weeks;Rolling group sessions;Same time as guided meditation practice; |
| Pollonini et al. (2020) | MM | 20 min | 10 | Once every weekday for two weeks;Same time as tDCS; | -M1of the hemisphere contralateral to the affected knee;-Supraorbital region contralateral to the affected knee; | 35 cm2 (rect-angular) | 20 min;10 s ramp up at the beginning and 10 s ramp down at the end; | 2 mA | Yes;0, 2, 0 mA;10 s ramp up to 30 s of 2 mA then 10 s ramp down at beginning only; | 10 | Once every weekday for two weeks;Same time as meditation; |
| Alizadehgoradel et al. (2021) | MBSAT | 50 min | 12 | Two sessions a week for six weeks;Immediately after tDCS; | -F3 (left dlPFC);-F4 (right dlPFC); | Not stated | 20 min;No ramp stated**; | 1.5 mA | Yes;0 and 1.5 mA;30 s ramp up to 1.5 mA for 30 s with a ramp down to 0 mA (unspecified duration of ramp) for the remaining time; | 12 | Two sessions a week at least 72-hrs apart for six weeks;Immediately before MBSAT; |
| Brooks et al. (2021) | MBSR | 2.5 hr | 57 (9 including retreat) | Once a week for eight weeks;One half day retreat between weeks 6 and 7;Only at the same time as tDCS during meditation practices (tDCS for 30 min of the MBSR);Asked to practice at home with tDCS for the remaining 6 days of the week; | -Fz;-Iz; | 25 cm2 | 30 min;30 s ramp up at the beginning and 30 s ramp down at the end; | 2 mA(0.57 A/m2) | Yes;0 and 2 mA;30 s ramp up to 2 mA for 54 s(3% of active) with 30 s ramp down to 0 mA for the remaining time; | 57 (9 including retreat) | Once a week for eight weeks;Same time as guided meditation part of MBSR;Asked to complete at home for the remaining 6 days of the week; |
| Liao et al. (2021) | Yang StyleTai Chi | 40 min | 36 | Three times a week for 12 weeks;Same time as tDCS for the first 20 min | -F3 (left dlPFC);-Fp4 (right supraorbital); | 35 cm2 | 20 min;10 s ramp up at the beginning;Duration of ramp down not stated; | 2 mA | Yes;0 and 2 mA;10 s ramp up to 2 mA for 30 s then ramp down to 0 mA;Duration of ramp down not stated; | 36 | Three times a week for 12 weeks;Same time as Tai Chi for the first 20 min |
| Park et al. (2021)* | Yoga | 1 h | 16 (2) | Two times a week for eight weeks;One hour after tDCS when tDCS was performed; | -CP6 (right tPJ);-Left supraorbital; | 35 cm2 (rect-angular) | 20 min;8 s ramp up at the beginning and 8 s ramp down at the end; | 2 mA | Yes;0 and 2 mA;8 s ramp up to 2 mA and then 8 s ramp down to 0 mA;Duration of 2 mA not stated; | 4 (2) | Each condition two times a week during week 1 or week 5;One hour before yoga; |
| Pimenta et al. (2021) | MM | At least20 min** | 28 (12) | Daily for four weeks;Same time as tDCS when tDCS was performed; | -F3 (left dlPFC); –Fp2 (right supraorbital); | 25 cm2 | 20 min;No ramp stated; | 2 mA | Yes;No sham current intensity stated;No ramp stated;2 mA current turned off automatically after 30 s; | 12 | Three days a week for four weeks;Same time as meditation; |
| Gibson et al. (2022) | MBRP | 2 hr | 8 | Once a week rolling group sessions for eight weeks;First 30 mins of guided meditation practice at the same time as tDCS and the following 90 min of discussions of mindfulness; | -F10 (right IFG);-Left upper arm; | 15 cm2 | 30 min;30 s ramp up at the beginning and 30 s ramp down at the end; | 2 mA | Yes;0 and 2 mA;30 s ramp up to 2 mA with direct 30 s ramp down to 0 mA at the beginning and the end;0 mA for 28 min; | 8 | Once a week rolling group sessions for eight weeks;Same time as mindfulness; |
| Ramasawmy et al. (2022) | MM | 20 min(+ 5 min body scan) | 15 (10) | Once every weekday for three weeks, where the first week was for training only and the last 2 weeks at the same time as tDCS; | -Left primary motor cortex;-Right supraorbital; | 16 cm2 (anode; square);50 cm2 (cathode;Rectangu-lar) | 20 min;15 s ramp up at the beginning and 15 s ramp down at the end; | 2 mA | Yes;0 and 2 mA;15 s ramp up to 2 mA for 30 s then 15 s ramp down to 0 mA for the remaining time; | 10 | Once every weekday for two weeks;Same time as mediation; |
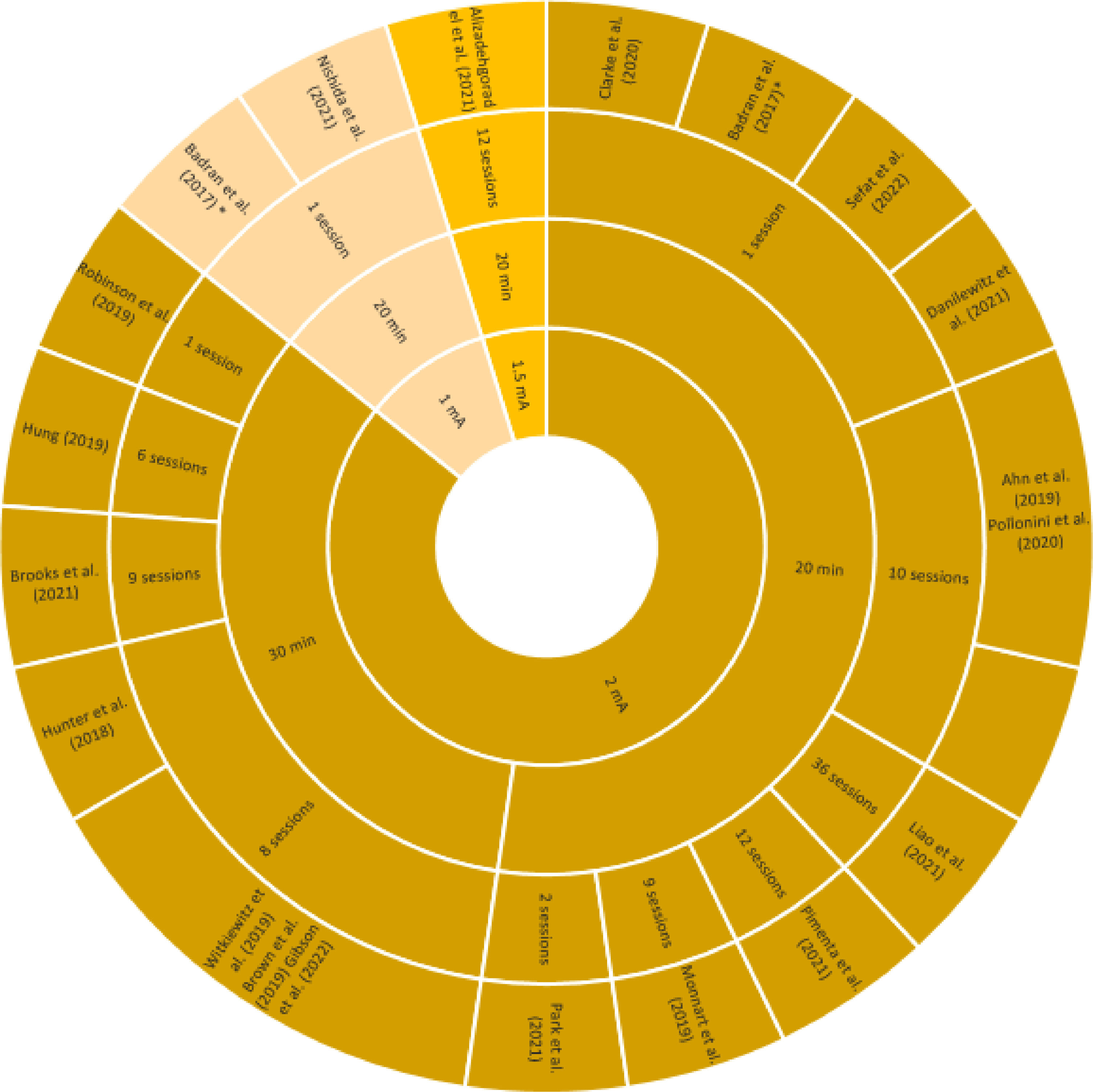
For the selected publications, the stimulation parameters are listed in Table 3 & 4 according to participant population groups and visualized in Fig. 3. The most common duration of stimulation was 20 min (65%, Fig. 3). The only studies that used 30-min stimulations were done at 2 mA (35%, Fig. 3). The montages of electrode placement for the 20 published studies were very different (Table 3 & 4). The most frequent montage was the left (anode, F3) and right (cathode, F4) dorsolateral prefrontal cortex (dlPFC) (25%, Alizadehgoradel et al., 2021; Danilewitz et al., 2021; Hung, 2019; Monnart et al., 2019; Sefat et al., 2022). Generally, most of the studies (95%) stimulated the frontal lobe with the exception being Park et al. (2021), who stimulated at the right temporoparietal junction (tPJ). It should also be noted that Robinson et al. (2019) also stimulated the tPJ along with the dlPFC. In addition, the overall number of sessions varied greatly across the tDCS parameters.
Hierarchical representation of the stimulation parameters that was used in tandem with a meditation technique for the selected studies. The order of significance from the inside-out is the intensity (mA), duration, and then number of sessions. The number of sessions only represent those that were active sessions together with the meditation technique. The outer most layer is the study itself. The * represents the study that had two different stimulation intensities.
Review of Selected Groups of Studies
tDCS + meditation in healthy peopleImpact on psychological and emotional wellbeingIn 2017, Badran et al. were the first to combine tDCS with meditation, donning the term E-meditation with the goal of facilitating meditation practice in naïve meditators to potentially enhance wellbeing. With respect to the meditation ability of the 15 included participants, those receiving 1 mA anodal tDCS applied at the left ventrolateral prefrontal cortex paired with MM showed higher ability to act with awareness as a measure of mindfulness level, compared to sham and frontal tDCS at 2 mA group. They found that E-meditation with tDCS at both 1 mA and 2 mA showed relevant mathematical improvements in positive affect of the participants (Badran et al., 2017). To further test the potential impact of E-meditation on facilitating mindfulness acquisition, Nishida et al. (2021) investigated brain function using electroencephalography (EEG) and anxiety levels following an intervention of 1 mA anodal tDCS applied at the left dlPFC concurrently paired with TW-FM. Participants in the active group reported one week later significantly lower state anxiety and current density of the alpha band at the rostral anterior cingulate cortex (rACC) which was significantly correlated to the anxiety scores than the sham group (sham tDCS+TW-FM). The authors suggest that the immediate reduction in rACC alpha activity might modulate the long-term activity of the amygdala, hence reducing anxiety level (Nishida et al., 2021).
Robinson et al. (2019) used a more robust study design with 8 arms to test the effects of concurrent anodal tDCS-LKM intervention on positive affect and emotional intelligence, varying the electrode placement (left dlPFC; right tPJ), current intensity (2 mA-active; 0.1 mA-sham) and meditation type (real LKM, control). Participants who received anodal tDCS at the tPJ with real LKM had a significantly higher positive affect to neutral and positive images after stimulation regardless of current strength than the other electrode position. However, they did not find any main effect of stimulation current strength, electrode placement, or LKM group on emotional intelligence or positive affect (Robinson et al., 2019). More recently, Clarke et al. (2020) investigated the combination of anodal tDCS over the left dlPFC and a guided body scan, a type of MM, on anxious responses to induced worry. They found significantly higher anxiety reactivity to intentional worry in participants receiving active tDCS regardless of active or sham MM condition, which they further argue that the enhanced emotional reactivity is rather due to the interaction between tDCS and networks involved in negative cognitive patterns such as worry (Clarke et al., 2020).
Impact on cognitive functionHunter et al. (2018) were the first to test the combination of MM and anodal tDCS at 2 mA over the right inferior frontal gyrus on working memory (WM) and attentional resource allocation using EEG. They found a group specific improvement in WM performance for the active group, but not for the sham group (real MM and sham tDCS). The observed larger P3 amplitude and redistribution of frontal and posterior theta power during the N-back WM task is in line with the neural efficiency hypothesis, which proposes a more efficient brain functioning with higher cognitive capacity level (Neubauer & Fink, 2009).
Along the same line of interest, Danilewitz et al. (2021) and Sefat et al. (2022) paired yoga with tDCS targeting WM. Danilewitz et al. (2021) found that one session of yoga following anodal 2 mA (left dlPFC) tDCS failed to show any improvement on WM or mindfulness level compared to a sham session of yoga combined with sham tDCS in a cross-over design. However, a placebo effect was observed with higher WM performances after first session than second one. Sefat et al. (2022) had a similar intervention design to Danilewitz et al. (2021), but rather, participants performed yoga prior to stimulation. Despite finding no significant differences in power spectral density, they found that anodal tDCS over the left dlPFC at 2 mA and yoga had significantly increased functional connectivity in the frontal lobe, as measured using EEG. They argued that this increased connectivity could lead to changes in executive and attentional functions.
tDCS + meditation in diseased patientsChronic painCombining meditation and tDCS opens a novel avenue in chronic pain management through their potential additive effects. Ahn et al. (2019) showed that patients suffering from knee osteoarthritis reported significant improvements of clinical pain and quantitative sensory assessments than the sham group (sham tDCS+sham MM) after 10 sessions of MM concurrently paired with 2 mA anodal tDCS over the primary motor cortex of the hemisphere contralateral to the affected knee. Pollonini et al. (2020) analyzed a participant subset from Ahn et al. (2019) to test the neuronal responses due to heat evoked pain using functional near-infrared spectroscopy. They showed significant reduction in pain intensity only in the active treatment group, but not in the sham group. Following active treatment, there was an increase in oxyhemoglobin activation in the superior motor and somatosensory cortices next to the anode (Pollonini et al., 2020). Recently, we tested the efficacy of 10 sessions with concurrent MM and 2 mA anodal tDCS over the left primary motor cortex in patients with fibromyalgia syndrome who received a brief 5-day training in MM (Ramasawmy et al., 2022). We found a significant improvement in the quality of life in patients in the active groups compared to the sham group (sham tDCS+real MM) and to a waiting-list control group, without any improvement in pain intensity, pain sensitivity, sleep and psychological symptoms.
Lastly, in a study on migraine headache, Pimenta et al. (2021) found that 4 weeks (3 days per week) of therapy combining MM and 2 mA anodal tDCS for 20 min over the left dlPFC concurrently in patients with chronic migraine improved results of both mindfulness and clinical headache pain assessments. Both the sham group (sham tDCS+real MM) and the active group benefitted from the therapy, but the effect sizes were larger in the active group than sham one.
Psychological disordersFour published studies investigated the effects of combined intervention on substance abuse disorders. However, a double-blinded study testing the combined effects of MBRP with tDCS in patients with alcohol use disorders led to three separate investigations of the data (Brown et al., 2020; Gibson et al., 2022; Witkiewitz et al., 2019). In this experiment, participants received either 8 sessions of 2 mA anodal tDCS over the right interior frontal gyrus or sham tDCS concurrently with MBRP training. Witkiewitz et al. (2019) demonstrated a significant decrease in alcohol consumption and craving across all groups post intervention, with effects lasting up to two months. However, there was no specific group effect observed, yet the more MBRP sessions participants took part in, the greater decrease in alcohol consumption occurred (Witkiewitz et al., 2019). Despite the lack of combined effects of tDCS and MBRP, the mindfulness intervention alone led to decreases in craving in response to alcohol cues was also supported by electrophysiological measurements (Brown et al., 2020). An interesting observation by Gibson et al. (2022) was that participants in the sham group with more mindfulness intervention sessions attended reported larger decreases in craving than the active tDCS group. However, no interaction effect for self-reported mindfulness was reported. Contrastingly, in a methamphetamine abuse study, Alizadehgoradel et al. (2021) evaluated the impact of combining anodal tDCS over the left dlPFC with MBSAT on executive function in young adults with methamphetamine addictions. They found that the combination of tDCS and MBSAT significantly improved most of the executive tasks and craving after intervention, while only the executive tasks were still improved one month later (Alizadehgoradel et al., 2021).
On the other hand, three studies were interested in effects of the combination therapy on depressive and anxiety disorders. Hung (2019) tested the therapeutic effects of combining 2 mA anodal tDCS over the left dlPFC and mindfulness training in patients with treatment resistant depression as compared to active tDCS and sham tDCS monotherapies. Hung (2019) found that the first e-mindfulness session after two weeks of tDCS training significantly decreased the depression ratings in all three groups, and the effect persisted over the remaining 6 weekly mindfulness trainings (including 2 e-mindfulness sessions). In a similar study with treatment resistant depression (Monnart et al., 2019), patients also received anodal tDCS over the left dlPFC but prior to undergoing MBCT or Jacobsen relaxation (sham MBCT). Nevertheless, their results show a significant improvement of anxiety, depression and cognitive symptoms post intervention compared to baseline in both groups, regardless of MBCT or relaxation, after 8 consecutive sessions with tDCS. However, those that received MBCT maintained more positive clinical and cognitive symptoms after an additional session 2 weeks after the 8 sessions of treatment (Monnart et al., 2019). Brooks et al. (2021) also examined the impact of concurrent anodal tDCS over Fz and MBSR in depressed and/or anxious elderly people on psychological impairment and cognition. Participants received 57 concurrent tDCS and meditation sessions (nine of which were performed in the clinic) during 8-weeks of MBSR, with the active group receiving 2 mA frontal anodal tDCS and the control group receiving sham tDCS. They found improvements without statistical significance in anxiety, mindfulness, social functioning, depression and cognitive performances with varying effect sizes in both interventions.
Other diseasesIn the elderly with mild cognitive impairment, Liao et al. (2021) found that 36 sessions of 40 min Yang style Tai Chi paired with 2 mA anodal tDCS over the left dlPFC (tDCS only during first 20 min of Tai Chi) significantly enhanced cognitive dual task performance, specifically gait, compared to a sham group combing sham tDCS and Tai Chi. Furthermore, one recent crossover pilot study (Park et al., 2021) with only five participants investigated the combined effects of yoga and anodal tDCS at 2 mA over the right temporoparietal junction in functional movement disorder. Each participant underwent a twice-weekly yoga session for eight weeks and received two sessions of either active or sham tDCS one hour before yoga on either the first or the fifth week of stimulation. They found no group effect on clinical symptom improvement and motor cortex excitability measured using transcranial magnetic stimulation (Park et al., 2021).
Overview of combined interventionsEighteen studies (90%) showed general improvements in either mindfulness behavior or primary clinical outcomes. Two studies, Danilewitz et al. (2021) and Clarke et al. (2020) showed no significant results and even worsened symptoms, respectively. Approximately less than half of the studies (40%: Ahn et al., 2019; Alizadehgoradel et al., 2021; Hunter et al., 2018; Liao et al., 2021; Nishida et al., 2021; Pollonini et al., 2020; Ramasawmy et al., 2022; Sefat et al., 2022) showed significant main effects from the combination of a meditation technique with anodal active over sham tDCS stimulation, where all but Nishida et al. (2021) and Sefat et al. (2022) had more than one active session. Five showed significant improvements without having any main or group effects (25%: Hung, 2019; Monnart et al., 2019; Pimenta et al., 2021; Robinson et al., 2019; Witkiewitz et al., 2019).
Four other studies did not show a significant effect of intervention but showed numerical improvements in the appropriate measurements or interaction effects (Badran et al., 2017; Brooks et al., 2021; Brown et al., 2020; Park et al., 2021), where two had specific improvements in the active group (active tDCS and meditation technique; Badran et al., 2017; Brown et al., 2020). The other remaining two studies had either improved across all groups with larger effect size in the active group (Brooks et al., 2021), or only showed general therapeutical improvements (Park et al., 2021).
In general, only five studies applied tDCS non-simultaneously with a meditation technique. In Sefat et al. (2022), participants practiced yoga prior to tDCS stimulation, while in the other four studies participants received tDCS stimulation prior to practicing in yoga (Danilewitz et al., 2021; Park et al., 2021), MBCT (Monnart et al., 2019), or MBSAT (Alizadehgoradel et al., 2021). In addition, out of the twenty studies included, only three studies included a sham meditation condition with active tDCS (Clarke et al., 2020; Monnart et al., 2019; Robinson et al., 2019). Meanwhile, three other studies included a sham tDCS with sham MM as the only control group (Ahn et al., 2019; Hunter et al., 2018; Pollonini et al., 2020).
DiscussionSummary of results from selected studiesThe above studies show promising results for the combined effects of tDCS and meditation on emotion regulation, psychological wellbeing, working memory, and pain perception. More specifically, all but two studies (Danilewitz et al., 2021: no significant results; Clarke et al., 2020: worsened symptoms) showed general improvements in either mindfulness behavior or primary clinical outcomes after one or more sessions. This aligns with previous studies claiming that tDCS is more effective with more sessions (Stagg et al., 2018). The studies that showed improvements in their outcomes, but did not necessarily have significant effects, typically improved when meditation training and practice was given.
However, the role of combined therapy on the overall improvements is not as clear across the remaining studies. Pimenta et al. (2021) had a larger effect size for the group with active tDCS and MM despite including additional MM training. Robinson et al. (2019) found significant results at a specific location with LKM, regardless of tDCS intensity, which could be explained by the lack of LKM and tDCS sessions. In addition, Gibson et al. (2022), one of the secondary analyses from Witkiewitz et al. (2019), interestingly only showed significant effects in the sham tDCS group and MBSR training group, but also had no interaction effect on mindfulness.
Methodological considerationsIn general, studies are inconsistent in terms of participant population, sample size, and study design. For example, most of the studies have small sample sizes for the active condition (mean n = 19.7) which diminishes the statistical power. Moreover, the clinical condition of the participants is very inconsistent across all studies, making it difficult to compare findings across the studies. It is known that the effects of meditation depend on the physical and emotional state of the subject especially based on their own personal goals and beliefs (Wolsko et al., 2004). On the other hand, tDCS effects also vary depending on whether the subject has had any caffeine or medicine that day, the mental and physical condition, as well as their age and education (Antal et al., 2008; Terranova et al., 2019). Moreover, if participants are aware of the conditions they are receiving, it can influence how they feel (placebo effect), and if experimenters are aware of the condition, it could skew their interpretation of the data. Therefore, having at least a double blinded study is crucial, yet 20% of the studies did not have such a design (Alizadehgoradel et al., 2021; Clarke et al., 2020; Hung, 2019; Monnart et al., 2019).
The studies that did not show a significant effect of intervention could be due to having cross over designs (Badran et al., 2017; Park et al., 2021), not having tDCS and meditation technique at the same time (Park et al., 2021), or not having a proper sham mediation technique (Badran et al., 2017; Brooks et al., 2021; Brown et al., 2020; Park et al., 2021). However, more research is necessary to confirm whether the combined techniques is sufficient for a non-invasive treatment. On the other hand, it is possible that Nishida et al. (2021) had such distinct results since participants were encouraged to practice mindful walking at home for 1 week prior to the last measurements and Sefat et al. (2022) had increased functional connectivity but not in power spectral density (EEG) possibly due to having a cross over design and including yoga as its meditation technique, which its effects have not been as thoroughly investigated in combination with tDCS.
Moreover, most of the studies did not control for meditation type, and thus only looked at the impact active tDCS on meditation. In general, meditation control conditions are important to investigate and determine, and thus should also be implemented alone. However, it is also important to have proper tDCS controls as comparing active tDCS combined with real meditation to a condition where sham tDCS is paired with control meditation makes it challenging to determine what is causing the effect. Therefore, monotherapies of both interventions should be included similarly to Hung (2019) and Alizadehgoradel et al. (2021). Lastly, the parameters of the sham tDCS condition was variable and needs to be further investigated so that there is a more universal sham condition in general. These make it challenging to discern whether the effects in the active tDCS and meditation group is due to the combination of effects or just active tDCS altering the brain responses from the meditation.
In addition to the study and participant characteristics, the number of sessions as well as the duration, and parameters of both tES and meditation techniques are essential for interpreting the results. It has been previously shown that repeated tDCS shows better offline effects (Nitsche & Paulus, 2011), which could explain why the studies with one active session does not show very conclusive effects. However, these studies, among some of the others, mostly did not include a proper training for learning meditation. Ramasawmy et al. (2022) was the only study to include MM training prior to the active sessions, while three other studies included training before and during the total experiment (Brooks et al., 2021; Park et al., 2021; Pimenta et al., 2021). Meditation especially can be difficult for those trying to meditate for the first time. On the other hand, the montage, intensity, and duration of tDCS used by these studies could also influence the final effects. In this review, many studies use the dlPFC as the anodal stimulation site, but it has been argued across majority of the studies that tDCS could have effects across the brain in addition to this location and that the site of stimulation is important for online and offline effects (Nitsche & Paulus, 2011). This means that other areas of the brain, when stimulated, may show better results when combined with meditation.
Expanding on the online and offline effects of tDCS, the interaction between the two techniques’ role in manipulating the brain could significantly influence the result. It is possible, as mentioned in Gibson et al. (2022), that the active tDCS and meditation group might be not showing an impact in these studies. They argue that mindfulness techniques cause the ongoing neural activity, which tDCS causes changes in, to be dispersed and more dynamic and thus the effects of tDCS are potentially diminished. In addition, the online and offline effects of both techniques could be cancelling each other out from the brain activity of mindfulness shifting between focused attention and monitoring (Gibson et al., 2022). Overall, it may be beneficial for future studies to implement more modeling and analysis of individual brain currents and circuitry with EEG or fMRI to help discern the precise techniques necessary (Terranova et al., 2019).
Finally, the timing of the tES and the meditation could also influence the impact shown on the measured outcomes. Out of the seven studies with healthy participants, five of them implemented the tDCS and meditation intervention at the exact same time (Badran et al., 2017; Clarke et al., 2020; Hunter et al., 2018; Nishida et al., 2021; Robinson et al., 2019). All but one (Clarke et al., 2020) showed improvements with the combined intervention. Lastly, the two remaining studies with healthy participants used tDCS and yoga one before another and found no combined effect on working memory (Danilewitz et al., 2021) but showed that there were functional connections occurring (Sefat et al., 2022). For the participants with mental or physical conditions, the results were even more variable.
The ongoing studies promote promising studies that investigate more thoroughly the impacts of tDCS and meditation/meditation techniques. Future studies should include larger sample sizes and precision of double blinding and study designs. In addition, investigating the longer lasting effects of the intervention will be very important for understanding the efficacy of these interventions. It is much easier for someone who is undergoing difficulties to do as little as possible to result in long term improvements, especially when it comes to lifestyle practices. Finally, the overall interaction between tDCS and meditation techniques still needs further analysis with proper control groups so that the influence of one on the other could be revealed.
LimitationsThis review has a few limitations. Firstly, this review is a traditional, systematic, qualitative clinical review on studies that involve a form of tDCS and meditation techniques. Therefore, there is no quantitative analysis on the included studies regarding their significance and clinical relevance. In addition, the general grouping of meditation was broadly defined and considered studies that included combined therapies of mindfulness and meditation techniques. Finally, some of the studies included were not the complete published papers, but rather manuscripts, letters, or proceedings, making it challenging to accurately display the results.
ConclusionHere, we investigated and discussed 20 published studies that used a combination of tDCS and a meditation technique with 664 participants comprising of both healthy and diseased participants. Furthermore, the most common combined techniques were anodal tDCS with mindfulness meditation. This study provides the general overview that the combination of tDCS and meditation shows promising yet inconclusive results of improvements on the physical, mental, and normal aspects of daily life. This review suggests that further studies need to improve on the mentioned limitations of study design and experimental stimulation and meditation training limitations in order to produce more reliable results. Combining tES and meditation is important to examine as both are non-invasive techniques that in combination have shown promising, but mostly not significant results of unclear clinical relevance. Their “combined” potential to enhance short- and long-term effects deserves further study.
We acknowledge the support by the Open Access Publication Funds of the Göttingen University. In addition, RD & PR was supported by the MSc/PhD program “Neurosciences” – International Max Planck Research School at the Georg August University Göttingen.