Occupational mutual insurance companies (OMICs), in collaboration with the Spanish Social Security System, provide healthcare and manage the economic benefits for the workers in Spain. They have ambulatory care centers that attend outpatient trauma pathology, although most of the studies published have focused on surgical and hospital activity.
The aim of this study was to detect adverse events (AEs) in outpatient trauma care in the context of an OMIC.
MethodsA cohort study designed to identify harmful safety incidents (adverse events, AEs) in 2017 was conducted. A random sample of 313 medical records among patients who were visited more than 3 medical and nursing attendances during their outpatient process. The AEs detected were classified according to category, severity and preventability.
ResultsWe identified 48 AEs (15.3% of medical records, 95% CI 11.3–19.3), most of them procedure-related, while 27 (56.2%) were preventable and 46 mild (95.8%).
ConclusionsThe AEs identified are double than those found in primary care general consultations in Spain and are close to the lower range of studies on surgical AEs in traumatology and orthopedics. Preventable AEs were within expected limits. Over half of AEs are preventable, within that group, the mild AEs have an increased rate of preventability. These results highlight the relevance of research of patient safety in the outpatient care of trauma and orthopaedic procedures in an OMIC for patient safety and contribute to introduce improvements in outpatient care.
Las Mutuas colaboradoras con la Seguridad Social gestionan las prestaciones sanitarias y económicas de la Seguridad Social para los trabajadores en España. Disponen de centros que atienden patología traumatológica ambulatoria poco conocidos en la bibliografía que se han centrado en la actividad quirúrgica y hospitalaria.
El objetivo de este estudio fue la detección de eventos adversos (EA) en la atención traumatológica ambulatoria en el contexto de una mutua laboral.
Materiales y MétodosSe desarrolló un estudio retrospectivo, observacional, descriptivo diseñado para identificar incidentes de seguridad con daño (EA) en 2017. Se analiza una muestra aleatoria de 313 historias clínicas de pacientes con más de tres atenciones médicas y de enfermería durante su proceso ambulatorio. Los EA detectados fueron clasificados según categoría, gravedad y evitabilidad.
ResultadosSe identificaron 48 EA (15,33% de historias clínicas, IC 95% 11,3-19,3), la mayoría relacionados con procedimientos, 27 (56,2%) se consideraron evitables y 46 leves (95,8%).
ConclusionesLos EA identificados multiplican por dos los hallados en los pacientes generales visitados en la atención primaria en España y se aproximan a la horquilla inferior de los estudios sobre EA quirúrgicos de traumatología y ortopedia. La evitabilidad es similar a la observada en otras series (en torno al 50%). Estos resultados ponen de manifiesto la situación, apenas estudiada hasta ahora, de la seguridad de pacientes en el caso de la atención ambulatoria traumatológica y ortopédica en una mutua laboral y contribuyen a la incorporación de mejoras en la atención ambulatoria.
Occupational mutual insurance companies (OMICs), in collaboration with the Spanish Social Security System, provide healthcare services and processes occupational contingencies economic benefits (accidents at work, occupational diseases, high-risk pregnancy and breastfeeding and help for parents of children affected by cancer or another serious illness) of workers in companies affiliated to the mutual societies and self-employed workers, as well as assessing temporary disability due to common contingencies.
These entities emerged at the beginning of the 20th century as voluntary associations of employers, constituted as private, non-profit entities.
The 19 OMICs manage around €13,500 million, with a health expenditure of €1,500 million. They have approximately 10,600 healthcare professionals, 1,000 primary ambulatory care centers, 23 hospitals, 1,300 hospital beds and 77 operating theatres. They undertake approximately 25 million consultations with patients who have suffered an accident at work and are on sick leave.1
Although it is the outpatient care of trauma pathology that predominates in the activity of OMICs, most studies have focused on surgical and hospital activity. Likewise, the analysis of the frequency of adverse events (AEs) in the course of this trauma care has focused on surgical activity, probably because, in this type of surgery, we know that AEs and claims for compensation and legal proceedings are higher than in other specialties.2–5
More than half of the AEs that occur in hospitals are related to general and orthopaedic surgery.6 Spine, knee and hip surgeries accumulate the highest number of claims.7 Surgical AE rates range, according to some studies, from 11 to 66%.4,8,9 Sathiyakumar et al.10 in 2015 found AE rates of 11.4% in trauma and 4.1% in orthopaedics. Pelvis and hip were three times more likely to develop incidents than lower extremities, and we found a prevalence of 45% of AEs in orthopedic surgery in latin American countries.11
Recently, in OMICs, as part of the promotion of patient safety policies,12,13 dashboards have been set up to monitor quality and safety key performance indicators, reporting systems,14 best practices and, since 2016, trigger tools which have been adapted to the reality of OMICs.15–17 However, the frequency of AEs in the outpatient activity of OMICs has not been analysed. The aim of this study was to detect AEs in outpatient trauma care in the context of an occupational mutual insurance company.
MethodsRetrospective, observational, descriptive (cohort study), designed to identify safety harmful incidents (AEs) in the course of outpatient health care provided to trauma patients, in 2017, in the ambulatory care centers of MC MUTUAL.
Study sampleThe review was conducted on a random sample (simple sampling) of 313 medical records of patients on sick leave greater than seven days with more than three medical and nursing attendances during their outpatient process, representing a sampling error of 3% (sample size calculated for an expected rate of 15%, 95% confidence level). These records were drawn from the pool of 870 patient records that were reviewed in the course of the annual quality audit programme of patient records. In these audits, 10 patient records were randomly reviewed (5 every semester) from each of the 87 ambulatory care centers of the company.
ReviewersThe medical records audit programme is carried out by a medical reviewer who is an expert in auditing, with specific training in quality, with periodic concordance analysis of a subset of the records reviewed, carried out by nurses who are experts in clinical management.
ProcedureThe sample is drawn from all records closed in the previous three months. The most complex patients’ records were selected, defined as patients who were off work sick greater than 7 days and received more than 3 visits (medical, nursing or physiotherapy) during the sick leave. From each of the 87 ambulatory care centers, 5 records are drawn at random every semester, which are audited. This audit focuses on clinical record quality items previously defined by the headquarters technical departments and reported to the whole organisation, referring to the work of medicine, nursing and physiotherapy. Allergies, prescription, medication reconciliation, drug administration, VAS pain scale and radiological protection among others were reviewed. If there was doubt, the reviewer consulted with members of the Healthcare Quality Unit team (comprising a doctor and two expert nurses) who agreed on the recording of the audit results. Systematic concordance analyses were carried out with double reading by one of the expert nurses of the Healthcare Quality team on a set of 5% of the total number of records reviewed. The medical records used for the concordance study were randomly drawn from the total number of records audited and reviewed according to a protocol and recorded in a Data Record Book (DRB) prepared by the Care Management Team (doctors, nurses and physiotherapists) and Healthcare Quality Unit (doctors and nurses) teams. All have specific training to ensure the validity of the procedure. The 80% concordance values obtained were considered to be adequate. The audit procedure was approved by the Health Quality Monitoring Committee, led by the first level of management of the company and with the participation of the top professional managers of the ambulatory care centers and hospitals, with the support of the Health Quality Unit.
In this study, a simple randomisation procedure was applied to extract 313 medical records from the 870 records included in the planned audit. Trigger tools designed for this case study were applied to identify adverse events.17 The information for each AE was coded in the DRB.
Data analysisThe AEs detected were classified according to the categories defined in the Spanish ENEAS report18 (Care, Medication, Infections, Procedures and Diagnosis), after that, APEAS report defines the different causality for each category which specific causal factors were identified for each group of AEs following the proposed taxonomy.19 For each AE, severity was assessed in levels E to G, ranging from mild to more serious effect, following the recommendation of the National Coordinating Council for Medication Error Reporting and Prevention (NCCMERP)20 (we have not considered incidents in categories A to D, and we have not had any serious AEs corresponding to categories H and I). Preventability was determined by using the scale 1–6, ranging from 1 not clear that it could be preventable to 6 absolute evidence that it is preventable, used in the APEAS report.19
ResultsAmong the 313 patient records with the highest care workload, 48 AEs were identified (15.3% of patient records, 95% CI 11.3–19.3).
The average age of patients who experienced AEs was 45.1 years (CV 22%) compared to 41.9 years (CV 25.3%) among patients who did not experience AEs, showing no statistically significant differences. 55% of patients who experienced an AE were male compared to 65% male in the no AE group, showing no statistically significant differences. A review of the group of patients with AEs revealed that 25% underwent surgery compared to 6.3% of patients in the group without AEs (Chi 2: 14.0, df:1, p<0.0001).
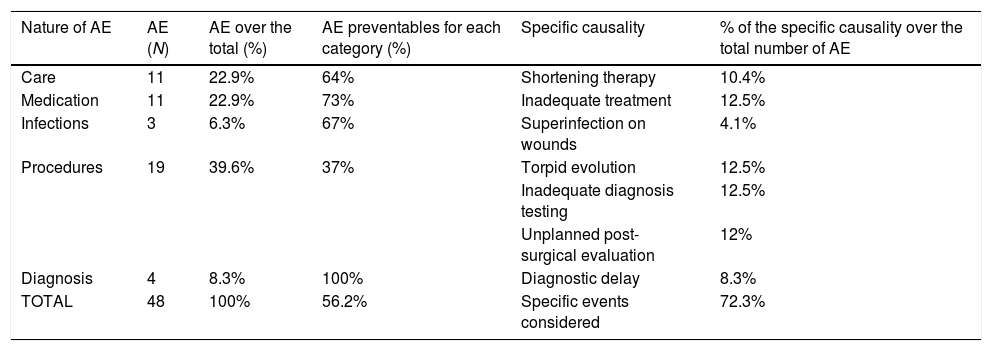
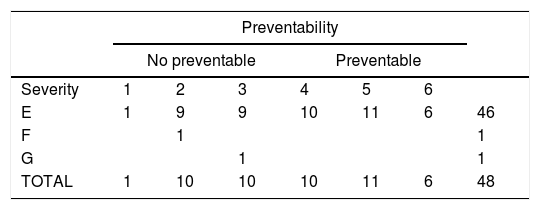
The majority of AEs were procedure-related (39.6% of the total), due to torpid evolution, inadequate testing and unplanned post-surgical evaluation. This was followed by AEs care-related (22.9%), especially those caused by shortening therapy and those related to medication (22.9%). AEs related to infections and diagnosis accounted both for less than 10 percent. The specific causal factors considered account for 72.3% of the total number of AE (Table 1). More than half of the AEs were considered preventable. Overall, the 27 preventable AEs were mild and showed different preventability rates depending on their nature (Table 2 shows all the combinations between preventability and severity). The other 21 EAs no preventable (43.8% of the total of EAs) were 90.4% mild and two moderate and serious (4.8% each).
Frequency, nature, preventability and specific causality of adverse events.
| Nature of AE | AE (N) | AE over the total (%) | AE preventables for each category (%) | Specific causality | % of the specific causality over the total number of AE |
|---|---|---|---|---|---|
| Care | 11 | 22.9% | 64% | Shortening therapy | 10.4% |
| Medication | 11 | 22.9% | 73% | Inadequate treatment | 12.5% |
| Infections | 3 | 6.3% | 67% | Superinfection on wounds | 4.1% |
| Procedures | 19 | 39.6% | 37% | Torpid evolution | 12.5% |
| Inadequate diagnosis testing | 12.5% | ||||
| Unplanned post-surgical evaluation | 12% | ||||
| Diagnosis | 4 | 8.3% | 100% | Diagnostic delay | 8.3% |
| TOTAL | 48 | 100% | 56.2% | Specific events considered | 72.3% |
N=48 AEs.
Preventability and severity of Adverse Events.
| Preventability | |||||||
|---|---|---|---|---|---|---|---|
| No preventable | Preventable | ||||||
| Severity | 1 | 2 | 3 | 4 | 5 | 6 | |
| E | 1 | 9 | 9 | 10 | 11 | 6 | 46 |
| F | 1 | 1 | |||||
| G | 1 | 1 | |||||
| TOTAL | 1 | 10 | 10 | 10 | 11 | 6 | 48 |
N=48 AEs.
Severity categories – A: Circumstances or events that have the capacity to cause error. B: An error occurred but the error did not reach the patient. C: An error occurred that reached the patient, but did not cause patient harm. D: An error occurred that reached the patient and required monitoring to confirm that it resulted in no harm to the patient and/or required intervention to preclude harm. E: Mild effect that resulted in temporary harm to the patient and required intervention, F: Moderate effect that resulted in temporary harm to the patient and required initial or prolonged care, G: More serious effect that resulted in permanent patient harm.
Preventability – 1–6, where 6 represents an incident that could certainly have been prevented.
The frequency of AEs per patient observed in our sample was 15.3%, slightly more than double those calculated in the APEAS study19 (7.4 AEs per 100 patients extrapolating the findings per appointment), likely related to the bias of our sample, and were close to the lower range of studies on surgical AEs in trauma and orthopaedics.2,8–10 Preventable AEs were within expected limits. Over half of AEs were preventable,21,22 within that group, the mild AEs had an increased rate of preventability.
These results highlight the problem of patient safety in the attendance of trauma and orthopaedic processes in the highest care workload outpatients in an OMIC, which has hardly been studied to date. The data was extracted from those cases in which, due to their complexity, the probability of AEs in outpatient care was expected to be higher and excluded surgical patients in trauma and orthopaedics for whom the frequency of occurrence of safety incidents is known.2,5–9 The main value of this data is that it explores the frequency of AEs in a previously unanalysed population and highlights the need to implement patient safety plans in a systematised way, including an analysis of the safety incidents’ causes, especially the most serious ones, in order to prevent their recurrence.23
The implementation of patient safety plans in OMICs has required the development of risk maps, treatment plans and safety incident reporting systems. These instruments can give a false sense of security in the perception that things are reasonably under control. The review of medical records, or other clinical review systems, offers a unique opportunity to identify what really needs to be done. However, the identification of AEs in ambulatory trauma procedures appears more complex and variable than in surgical procedures.24
Medical record audits are widely used tools for quality review of clinical records. It has progressively shown its usefulness for the review of some quality standards or, as in this case, the detection of undeclared AEs. The use of trigger tools increases the ability to identify safety incidents and should be considered when interpreting and comparing these results.25,26
The study sample was drawn during the audit of medical records and represents the picture of the highest workload cases seen in outpatient care. This review was based on a single, but highly trained and systematically oriented observer and double reading of a sub-sample.
In patient safety studies, it is recognised that there is a particular difficulty in categorising AEs, specifying their diagnosis, extent, severity and preventability. Moreover, in each specialty and in each setting, there are particularities that need to be considered. Outpatient care shows particular difficulties, related to the extent of its care, the generality of its actions and a certain perception, totally incorrect, that “nothing important happens” due to the false belief that all AEs are mild. The ambulatory care centers of the OMICs are entities that bring together several of the aforementioned difficulties, the general ones and those peculiar to occupational trauma, of the healthy population injured and cared for in the ambulatory care centers. This study shows the convenience of patient safety plans, also for outpatient care.
FundingThe present research has not received any specific financial support from agencies in the public, commercial, or non-profit sectors.
Conflict of interestNone.