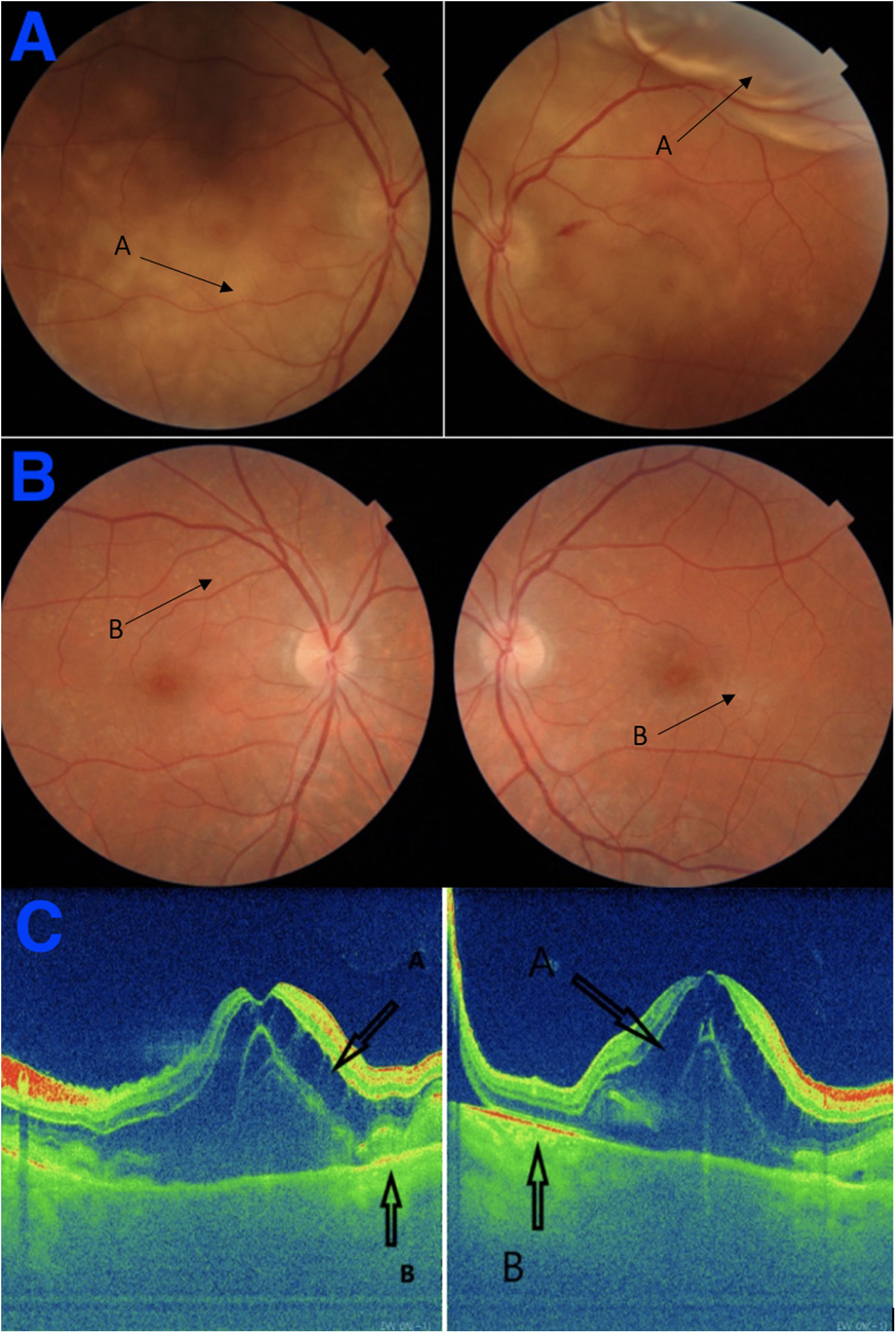
array:23 [ "pii" => "S238702062300181X" "issn" => "23870206" "doi" => "10.1016/j.medcle.2022.12.012" "estado" => "S300" "fechaPublicacion" => "2023-05-26" "aid" => "6161" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2022" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2023;160:461-3" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "itemSiguiente" => array:19 [ "pii" => "S2387020623001675" "issn" => "23870206" "doi" => "10.1016/j.medcle.2023.01.013" "estado" => "S300" "fechaPublicacion" => "2023-05-26" "aid" => "6184" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2023;160:463-4" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Infective endocarditis due to <span class="elsevierStyleItalic">Capnocytophaga canimorsus</span> in an immunocompetent patient" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "463" "paginaFinal" => "464" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Endocarditis infecciosa por <span class="elsevierStyleItalic">Capnocytophaga canimorsus</span> en una paciente inmunocompetente" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1480 "Ancho" => 2758 "Tamanyo" => 319250 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Figure " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Imaging tests performed on the case. (A) Dorsocervical spine MRI showing a posterior epidural abscess (arrow). (B) Transesophageal echocardiography, long-axis longitudinal plane, showing a periannular aortic abscess (arrow).</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Didac González Sans, Pau Carratalà Marín, Alfredo Guillen-del-Castillo" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Didac" "apellidos" => "González Sans" ] 1 => array:2 [ "nombre" => "Pau" "apellidos" => "Carratalà Marín" ] 2 => array:2 [ "nombre" => "Alfredo" "apellidos" => "Guillen-del-Castillo" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775323000325" "doi" => "10.1016/j.medcli.2023.01.014" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775323000325?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020623001675?idApp=UINPBA00004N" "url" => "/23870206/0000016000000010/v2_202311101432/S2387020623001675/v2_202311101432/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2387020623001638" "issn" => "23870206" "doi" => "10.1016/j.medcle.2022.12.011" "estado" => "S300" "fechaPublicacion" => "2023-05-26" "aid" => "6152" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2023;160:460-1" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "<span class="elsevierStyleItalic">Rickettsia sibirica</span> infection" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "460" "paginaFinal" => "461" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Infección por <span class="elsevierStyleItalic">Rickettsia sibirica</span>" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 622 "Ancho" => 1500 "Tamanyo" => 78317 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Fig. " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">A) Macular rash with pale pink lesions smaller than 0.5 cm. B) Ulcerated, necrotic, crusted lesion in the posterior cervical region, about 1 cm in size, surrounded by an erythematous halo.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Ignacio Lasierra Lavilla, Julien Paola Caballero Castro, Sergio Ignacio Zabala López" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Ignacio" "apellidos" => "Lasierra Lavilla" ] 1 => array:2 [ "nombre" => "Julien Paola" "apellidos" => "Caballero Castro" ] 2 => array:2 [ "nombre" => "Sergio Ignacio" "apellidos" => "Zabala López" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775322006698" "doi" => "10.1016/j.medcli.2022.12.012" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775322006698?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020623001638?idApp=UINPBA00004N" "url" => "/23870206/0000016000000010/v2_202311101432/S2387020623001638/v2_202311101432/en/main.assets" ] "en" => array:15 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Bilateral serous retinal detachment in pregnancy-induced hypertension" "tieneTextoCompleto" => true "saludo" => "<span class="elsevierStyleItalic">Dear Editor</span>," "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "461" "paginaFinal" => "463" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Francisco M. Hermoso-Fernández, Cristina Palma Conesa, Carmen Gonzalez-Gallardo" "autores" => array:3 [ 0 => array:4 [ "nombre" => "Francisco M." "apellidos" => "Hermoso-Fernández" "email" => array:1 [ 0 => "framaherfer@gmail.com" ] "referencia" => array:2 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] 1 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] 1 => array:3 [ "nombre" => "Cristina" "apellidos" => "Palma Conesa" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] ] ] 2 => array:3 [ "nombre" => "Carmen" "apellidos" => "Gonzalez-Gallardo" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] ] ] ] "afiliaciones" => array:2 [ 0 => array:3 [ "entidad" => "Department of Ophthalmology, Hospital Universitario San Cecilio, 18016 Granada, Spain" "etiqueta" => "a" "identificador" => "aff0005" ] 1 => array:3 [ "entidad" => "Department of Pediatrics, Hospital Universitario San Cecilio, 18016 Granada, Spain" "etiqueta" => "b" "identificador" => "aff0010" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Desprendimiento de retina bilateral seroso en un caso de hipertensión inducida por el embarazo" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 2239 "Ancho" => 1505 "Tamanyo" => 408751 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">(A) Arrows A: Detachment in the posterior pole. (B) Arrows B: Residual pigmentary changes (Elschnig spots). (C) On the left RE and on the right LE. Arrow A: sensorineural detachment; Arrow B: detachment of the pigment epithelium.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">Pregnancy-induced hypertension (PIH) is believed to cause acute retinal pigment epitheliopathy due to choroidal ischemia. It has been also demonstrated that nonperfusion of the choriocapillaris can cause necrosis of the overlying retinal pigment epithelium (RPE), which leads to the breakdown of the outer blood–retinal barrier and the development of serous retinal detachment (SRD).<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">1</span></a></p><p id="par0010" class="elsevierStylePara elsevierViewall">We report the case of a 31 years old woman who presented blurry vision in both eyes a few hours after the delivery. In the systemic exploration a peripartum eclampsia was detected. A nuclear magnetic resonance was performed with suggestive findings of small acute ischemic lesion in left caudate nucleus that during the follow up over the next three months, were normalized without any sequels.</p><p id="par0015" class="elsevierStylePara elsevierViewall">Ophthalmologist exploration revealed: visual acuity (VA) in his right eye (RE) was 0.2 and 0.12 in his left eye (LE). Intra-ocular pressure (IOP) was 8 and 6<span class="elsevierStyleHsp" style=""></span>mmHg in RE and LE respectively. Fundoscopy examination showed a bilateral serous retinal detachment associated with choroidal detachment (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>A). OCT revealed a neuro-sensory detachment with cystoid macular edema (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>C).</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0020" class="elsevierStylePara elsevierViewall">The visual field showed a superior temporal peripheral scotoma, in agreement with the lower peripheral zone where the retinal detachment is finally found before complete resorption. The patient was treated with labetalol 200<span class="elsevierStyleHsp" style=""></span>mg/8<span class="elsevierStyleHsp" style=""></span>h, aspirin 100<span class="elsevierStyleHsp" style=""></span>mg/24<span class="elsevierStyleHsp" style=""></span>h and omeprazole 20<span class="elsevierStyleHsp" style=""></span>mg/24<span class="elsevierStyleHsp" style=""></span>h. Treatment with corticosteroids was proposed: oral prednisone 30<span class="elsevierStyleHsp" style=""></span>mg per day, dexamethasone eye drops every six hours and topical dexamethasone ointment twice a day with the aim of increasing IOP and correcting ocular hypotonia caused by choroidal detachment. An enhancement of VA (RE<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>1, LE<span class="elsevierStyleHsp" style=""></span>=<span class="elsevierStyleHsp" style=""></span>0.8) was observed in recent checkups and there was also a spontaneous resorption of the subretinal fluid and resolution of retinal detachment.</p><p id="par0025" class="elsevierStylePara elsevierViewall">Regarding the visual sequelae of the patient, it is worth highlighting a slight alteration in VA as well as poor color vision, due to the involvement of the cones in the macula and the fovea as a result of hypertrophy of the RPE and strongly correlated with a lack of underlying outer segment regeneration.<a class="elsevierStyleCrossRef" href="#bib0035"><span class="elsevierStyleSup">2</span></a> In addition, there was a reduced visual field due to the presence of scotomas, a consequence of several ischemic points that translated into definitive lesions of peripheral photoreceptors.</p><p id="par0030" class="elsevierStylePara elsevierViewall">PIH is believed to cause acute retinal pigment epitheliopathy due to choroidal ischemia. Endothelial damage of the choroidal vasculature can also lead to fibrinoid necrosis of the choroidal arterioles with choriocapillaris occlusion. Other studies have also demonstrated that nonperfusion of the choriocapillaris can cause necrosis of the overlying RPE, which leads to the breakdown of the outer blood–retinal barrier and the development of SRD. In the case of our patient, despite the fact that it is a case of late-onset eclampsia, cases in which it is assumed, as described in the literature the imbalance between angiogenic factors is not generated.<a class="elsevierStyleCrossRef" href="#bib0040"><span class="elsevierStyleSup">3</span></a> However, the ischemic lesions found both at the central level (nucleus putamen) as well as the lesions at the ophthalmological level support the theory that it is a HELLP syndrome characterized by thrombotic microangiopathy.</p><p id="par0035" class="elsevierStylePara elsevierViewall">The principal management of retinal detachment in pre-eclampsia is conservative and involves treating the underlying condition. After delivery, the sub-retinal fluid is reabsorbed and the visual acuity returns within weeks.<a class="elsevierStyleCrossRef" href="#bib0045"><span class="elsevierStyleSup">4</span></a> Although retinal detachments have previously been related to preeclampsia, both choroidal detachments with a marked drop in intraocular pressure and retinal cystic edema that we observed in our patient have not been described in other cases published in the literature.<a class="elsevierStyleCrossRef" href="#bib0050"><span class="elsevierStyleSup">5</span></a> On the other hand, the use of ocular hypotensive treatment is usually described in retinal and choroidal detachments to achieve the application of said ocular layers. But, hypotension and therefore choroidal detachments would have been aggravated. Therefore, it was decided to use only corticosteroids, both systemic and topical.</p><p id="par0040" class="elsevierStylePara elsevierViewall">Clinicians should be aware of these ocular manifestations and careful ophthalmological and neurological evaluation should be carried out along with neuroimaging to ascertain the various causes of blindness in pregnancy. The prognosis is usually good, especially with cortical blindness where the loss of vision is transient.<a class="elsevierStyleCrossRef" href="#bib0045"><span class="elsevierStyleSup">4</span></a></p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Ethical approval</span><p id="par0045" class="elsevierStylePara elsevierViewall">Informed consent for publication of clinical details and/or images was obtained from the patient. Ethics approval is not applicable. Written informed consent was acquired.</p></span><span id="sec0010" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0010">Funding</span><p id="par0050" class="elsevierStylePara elsevierViewall">No funds have been received for this study.</p></span><span id="sec0015" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0015">Conflict of interest</span><p id="par0055" class="elsevierStylePara elsevierViewall">We have no conflicts of interest to disclose.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:4 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Ethical approval" ] 1 => array:2 [ "identificador" => "sec0010" "titulo" => "Funding" ] 2 => array:2 [ "identificador" => "sec0015" "titulo" => "Conflict of interest" ] 3 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "multimedia" => array:1 [ 0 => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 2239 "Ancho" => 1505 "Tamanyo" => 408751 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">(A) Arrows A: Detachment in the posterior pole. (B) Arrows B: Residual pigmentary changes (Elschnig spots). (C) On the left RE and on the right LE. Arrow A: sensorineural detachment; Arrow B: detachment of the pigment epithelium.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0015" "bibliografiaReferencia" => array:5 [ 0 => array:3 [ "identificador" => "bib0030" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Subretinal deposits in pre-eclampsia and malignant hypertension: implications for age-related macular degeneration" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "O. Otero-Marquez" 1 => "H. Chung" 2 => "C.S. Lee" 3 => "E.Y. Choi" 4 => "G. Ledesma-Gil" 5 => "S. Alauddin" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Ophthalmol Retin" "fecha" => "2021" "volumen" => "5" "paginaInicial" => "750" "paginaFinal" => "760" ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0035" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Retinal reattachment of the primate macula. Photoreceptor recovery after short-term detachment" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "C.J. Guerin" 1 => "D.H. Anderson" 2 => "R.N. Fariss" 3 => "S.K. Fisher" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Invest Ophthalmol Vis Sci" "fecha" => "1989" "volumen" => "30" "paginaInicial" => "1708" "paginaFinal" => "1725" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/2527212" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0040" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Choroidal thickening and macular serous retinal detachment in pregnancy-induced hypertension" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "R. Aoyagi" 1 => "T. Hayashi" 2 => "H. Tsuneoka" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.2147/IMCRJ.S95442" "Revista" => array:5 [ "tituloSerie" => "Int Med Case Rep J [Internet]" "fecha" => "2015" "volumen" => "8" "paginaInicial" => "291" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/26635487" "web" => "Medline" ] ] ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0045" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "The eye and visual system in the preeclampsia/eclampsia syndrome: What to expect?" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "K. Abu Samra" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Saudi J Ophthalmol Off J Saudi Ophthalmol Soc [Internet]" "fecha" => "2013" "volumen" => "27" "paginaInicial" => "51" "paginaFinal" => "53" ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0050" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "syndrome with unilateral exudative retinal detachment treated conservatively" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "A.V. Pradeep" 1 => "S. Rao" 2 => "R. Ramesh Kumar" 3 => "HELLP. Partial" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Saudi J Ophthalmol Off J Saudi Ophthalmol Soc [Internet]" "fecha" => "2014" "volumen" => "28" "paginaInicial" => "329" "paginaFinal" => "331" ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000016000000010/v2_202311101432/S238702062300181X/v2_202311101432/en/main.assets" "Apartado" => array:4 [ "identificador" => "43309" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Letters to the Editor" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000016000000010/v2_202311101432/S238702062300181X/v2_202311101432/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S238702062300181X?idApp=UINPBA00004N" ]
Journal Information
Vol. 160. Issue 10.
Pages 461-463 (May 2023)
Vol. 160. Issue 10.
Pages 461-463 (May 2023)
Letter to the Editor
Bilateral serous retinal detachment in pregnancy-induced hypertension
Desprendimiento de retina bilateral seroso en un caso de hipertensión inducida por el embarazo
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail