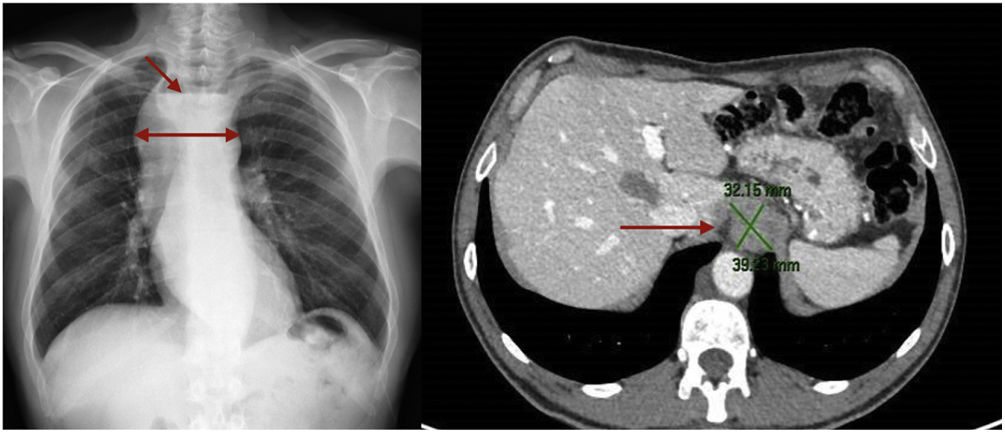
array:24 [ "pii" => "S2387020623003480" "issn" => "23870206" "doi" => "10.1016/j.medcle.2023.09.002" "estado" => "S300" "fechaPublicacion" => "2023-09-29" "aid" => "6284" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2023" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2023;161:269-70" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S002577532300249X" "issn" => "00257753" "doi" => "10.1016/j.medcli.2023.04.025" "estado" => "S300" "fechaPublicacion" => "2023-09-29" "aid" => "6284" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2023;161:269-70" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta al Editor</span>" "titulo" => "Seudotumor inflamatorio como forma de presentación atípica de acalasia" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "269" "paginaFinal" => "270" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Inflammatory pseudotumor as an atypical presentation of achalasia" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figura 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 433 "Ancho" => 1005 "Tamanyo" => 61237 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">A) Radiografía de tórax anteroposterior donde se visualiza ensanchamiento de mediastino anterior (flecha larga) con nivel hidroaéreo en su interior (flecha corta). B) Corte transversal de tomografía computarizada de abdomen. Se observa una masa de 39<span class="elsevierStyleHsp" style=""></span>×<span class="elsevierStyleHsp" style=""></span>32<span class="elsevierStyleHsp" style=""></span>mm a nivel de la unión gastroesofágica de bordes bien definidos (flecha).</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Antonio Bustos-Merlo, Ana Peragón-Ortega, Antonio Rosales-Castillo" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Antonio" "apellidos" => "Bustos-Merlo" ] 1 => array:2 [ "nombre" => "Ana" "apellidos" => "Peragón-Ortega" ] 2 => array:2 [ "nombre" => "Antonio" "apellidos" => "Rosales-Castillo" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020623003480" "doi" => "10.1016/j.medcle.2023.09.002" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020623003480?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S002577532300249X?idApp=UINPBA00004N" "url" => "/00257753/0000016100000006/v1_202309190535/S002577532300249X/v1_202309190535/es/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S2387020623003492" "issn" => "23870206" "doi" => "10.1016/j.medcle.2023.04.030" "estado" => "S300" "fechaPublicacion" => "2023-09-29" "aid" => "6289" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2023;161:270-1" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Polymyalgia rheumatica after pembrolizumab treatment" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "270" "paginaFinal" => "271" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Polimialgia reumática tras tratamiento con pembrolizumab" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Silvia Ramirez-Poza, Alfredo José Pardo-Cabello, Juan Salvatierra" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Silvia" "apellidos" => "Ramirez-Poza" ] 1 => array:2 [ "nombre" => "Alfredo José" "apellidos" => "Pardo-Cabello" ] 2 => array:2 [ "nombre" => "Juan" "apellidos" => "Salvatierra" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775323002464" "doi" => "10.1016/j.medcli.2023.04.030" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775323002464?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020623003492?idApp=UINPBA00004N" "url" => "/23870206/0000016100000006/v1_202309251317/S2387020623003492/v1_202309251317/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2387020623003455" "issn" => "23870206" "doi" => "10.1016/j.medcle.2023.04.028" "estado" => "S300" "fechaPublicacion" => "2023-09-29" "aid" => "6273" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "crp" "cita" => "Med Clin. 2023;161:267-8" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Scientific letter</span>" "titulo" => "Caplacizumab in acquired thrombotic thrombocytopenic thrombocytopenic purpura: dose adjustment based on von Willebrand factor level" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "267" "paginaFinal" => "268" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Caplacizumab en la púrpura trombocitopénica trombótica adquirida: ajuste de la dosis basado en el factor de von Willebrand" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0005" "etiqueta" => "Figure 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 2096 "Ancho" => 3175 "Tamanyo" => 420638 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Figure " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Change in main laboratory parameters and summary of key aspects and clinical outcomes of caplacizumab treatment. The horizontal line indicates treatment duration in days. (E) Change in ADAMTS13 activity (%). (A) Change in platelet count. (F) Change in von Willebrand factor (vWF). (B) Changes in lactate dehydrogenase (LDH). (C) Changes in haemoglobin. (D) Trends in total bilirubin. (G) Key aspects and clinical outcome of the patient. The horizontal line indicates the duration of treatment in days.</p> <p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">ADAMTS13, a disintegrin and metalloproteinase with thrombospondin type 1 motif, 13; vWF, von Willebrand factor; IgG, immunoglobulin G; LDH,: lactate dehydrogenase; PE, plasma exchange.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Marta Albanell-Fernández, Inés Monge-Escartín, Joan Cid" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Marta" "apellidos" => "Albanell-Fernández" ] 1 => array:2 [ "nombre" => "Inés" "apellidos" => "Monge-Escartín" ] 2 => array:2 [ "nombre" => "Joan" "apellidos" => "Cid" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S002577532300235X" "doi" => "10.1016/j.medcli.2023.04.017" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S002577532300235X?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020623003455?idApp=UINPBA00004N" "url" => "/23870206/0000016100000006/v1_202309251317/S2387020623003455/v1_202309251317/en/main.assets" ] "en" => array:15 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Inflammatory pseudotumor as an atypical presentation of achalasia" "tieneTextoCompleto" => true "saludo" => "Dear Editor," "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "269" "paginaFinal" => "270" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Antonio Bustos-Merlo, Ana Peragón-Ortega, Antonio Rosales-Castillo" "autores" => array:3 [ 0 => array:4 [ "nombre" => "Antonio" "apellidos" => "Bustos-Merlo" "email" => array:1 [ 0 => "antoniobustosmerlo@gmail.com" ] "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] 1 => array:2 [ "nombre" => "Ana" "apellidos" => "Peragón-Ortega" ] 2 => array:2 [ "nombre" => "Antonio" "apellidos" => "Rosales-Castillo" ] ] "afiliaciones" => array:1 [ 0 => array:2 [ "entidad" => "Servicio de Medicina Interna, Hospital Universitario Virgen de las Nieves, Granada, Spain" "identificador" => "aff0005" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Seudotumor inflamatorio como forma de presentación atípica de acalasia" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 433 "Ancho" => 1005 "Tamanyo" => 62885 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Fig. " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">(A) Anteroposterior chest X-ray showing widening of the anterior mediastinum (long arrow) with air-fluid level inside (short arrow). (B) Cross section of abdominal computed tomography. A 39 × 32 mm mass can be seen at the level of the gastroesophageal junction with well-defined margins (arrow).</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">Achalasia is an oesophageal motility disorder manifested by the absence of peristalsis and insufficient relaxation of the lower oesophageal sphincter. The pathophysiological substrate is the destruction of neurons of the autonomic nervous system at this level. The annual incidence is estimated at 1.6 cases per 100,000 individuals, and a prevalence of 10 cases per 100,000 individuals.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> The most common clinical manifestations are dysphagia, regurgitation, chest pain and weight loss. Diagnosis is confirmed by oesophageal manometry, which also allows classification according to the contractility pattern.</p><p id="par0010" class="elsevierStylePara elsevierViewall">We report the case of a male patient with a high suspicion of gastroesophageal cancer, whose final diagnosis was inflammatory pseudotumour at the gastroesophageal junction secondary to type-1 achalasia.</p><p id="par0015" class="elsevierStylePara elsevierViewall">52-year-old man with a personal history of active smoking (40 packs/year) and chronic alcoholism (5 SD per day up to 6 months previously). Originally from Spain, where he had been living for 6 years after having lived in Colombia and Ecuador for 5 years. His usual treatment was lormetazepam 2 mg and omeprazole 20 mg/day. He came to the emergency department for progressive weight loss of 15 kg in the last 2 months, without associated anorexia. He had experienced episodes of mild generalised abdominal pain, together with dysphagia to solids and early postprandial fullness. Symptoms were relieved by occasional vomiting of food, with worsening in the last 6 weeks. Physical examination revealed a significant mucocutaneous dryness with preserved general condition and normal vital signs. No palpation of peripheral lymph nodes. Rhythmic heart tones, no murmurs. Excavatum, soft abdomen with no abnormal enlargement. Lower limbs without oedema or signs of deep vein thrombosis. Laboratory tests showed acute renal failure with a pre-renal profile and no electrolyte abnormalities. CBC and coagulation without anomalies. The systematic urine analysis showed ketonuria and the chest X-ray showed an anterior mediastinal widening with the presence of an air-fluid level inside. Given the high suspicion of an underlying neoplastic process, tests were arranged preferentially to accelerate the workup. <span class="elsevierStyleItalic">Trypanosoma cruzi</span> serology was negative. A cervicothoracic CT scan showed a stenosing mass at the gastroesophageal junction with severe retrograde oesophageal dilatation and retained food debris (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>). This was a major limitation for performing an upper gastrointestinal endoscopy, requiring 3 attempts, hospital admission, insertion of a nasogastric drainage tube, establishment of total parenteral nutrition and fasting for 72 h in order to achieve its performance. This showed an oesophageal dilatation with a tortuous appearance, without endoluminal lesions. Finally, an endoscopic ultrasound revealed a submucosal thickening at the subcarinal level with biopsy, which reported fibromuscular hyperplasia in the lamina propria, abundant lymphoplasmacytic infiltrate in the lamina propria and muscularis mucosae, and absence of intestinal metaplasia. Positron emission tomography (PET/CT) showed no pathological uptake at the gastroesophageal junction or at other distant sites. The study was completed with a manometry that showed a total absence of peristalsis and a pressurisation pattern compatible with type 1 achalasia. The patient’s final diagnosis was inflammatory pseudotumour at the gastroesophageal junction secondary to type 1 achalasia. Endoscopic dilatation with a 20 mm balloon was performed without complications, after which clinical improvement was observed. At the subsequent 3-month follow-up visit, there were no new episodes of dysphagia or vomiting, and weight gain was observed.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0020" class="elsevierStylePara elsevierViewall">There are few reported cases secondary to oesophageal inflammatory pseudotumour.<a class="elsevierStyleCrossRefs" href="#bib0010"><span class="elsevierStyleSup">2–4</span></a> It is an exceptionally rare entity, which makes it a diagnostic and therapeutic challenge. The aetiology is unknown; some authors suggest that the origin of this lesion is an inflammatory response to mucosal ulceration, while others attribute it to gastroesophageal reflux. It usually affects the submucosal layer in the lower portions of the oesophagus, with reactive cells, myofibroblasts and fibroblasts being confirmed histopathologically, together with inflammatory cells, dysplasia and in some cases pseudomalignant mesenchymal cells. As for the therapeutic approach, surgical resection is encouraged whenever possible, although in some cases the use of glucocorticoids is recommended as an alternative, although there is no clear consensus.<a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">5</span></a></p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">Funding</span><p id="par0025" class="elsevierStylePara elsevierViewall">The authors declare that they have not received any funding.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:2 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "Funding" ] 1 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "multimedia" => array:1 [ 0 => array:8 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 433 "Ancho" => 1005 "Tamanyo" => 62885 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Fig. " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">(A) Anteroposterior chest X-ray showing widening of the anterior mediastinum (long arrow) with air-fluid level inside (short arrow). (B) Cross section of abdominal computed tomography. A 39 × 32 mm mass can be seen at the level of the gastroesophageal junction with well-defined margins (arrow).</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0005" "bibliografiaReferencia" => array:5 [ 0 => array:3 [ "identificador" => "bib0005" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Achalasia: incidence, prevalence and survival. A population-based study" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "D.C. Sadowski" 1 => "F. Ackah" 2 => "B. Jiang" 3 => "L.W. Svenson" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1111/j.1365-2982.2010.01511.x" "Revista" => array:5 [ "tituloSerie" => "Neurogastroenterol Motil" "fecha" => "2010" "volumen" => "22" "paginaInicial" => "e256" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/20465592" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0010" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Inflammatory pseudotumor of the esophagus" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "A.P. Saklani" 1 => "C.S. Pramesh" 2 => "A.A. Heroor" 3 => "R. Saoji" 4 => "S. Sharma" 5 => "R.K. Deshpande" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1046/j.1442-2050.2001.00202.x" "Revista" => array:6 [ "tituloSerie" => "Dis Esophagus" "fecha" => "2001" "volumen" => "14" "paginaInicial" => "274" "paginaFinal" => "277" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/11869339" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0015" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Inflammatory pseudotumor of the esophagus-GI image" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "J. Li" 1 => "F. Liu" 2 => "Z. Wang" 3 => "Q. Liu" 4 => "Y. Wang" 5 => "Q. Zhou" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1007/s11605-009-0893-8" "Revista" => array:6 [ "tituloSerie" => "J Gastrointest Surg" "fecha" => "2010" "volumen" => "14" "paginaInicial" => "195" "paginaFinal" => "198" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/19381734" "web" => "Medline" ] ] ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0020" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Esophageal inflammatory pseudotumor mimicking malignancy" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "K. Kurihara" 1 => "K. Mizuseki" 2 => "M. Ichikawa" 3 => "K. Okada" 4 => "Y. Miyata" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.2169/internalmedicine.40.18" "Revista" => array:6 [ "tituloSerie" => "Intern Med" "fecha" => "2001" "volumen" => "40" "paginaInicial" => "18" "paginaFinal" => "22" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/11201363" "web" => "Medline" ] ] ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0025" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "European guidelines on achalasia: United European Gastroenterology and European Society of Neurogastroenterology and Motility recommendations" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "R.A.B. Oude Nijhuis" 1 => "G. Zaninotto" 2 => "S. Roman" 3 => "G.E. Boeckxstaens" 4 => "P. Fockens" 5 => "M.W. Langendam" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1177/2050640620903213" "Revista" => array:6 [ "tituloSerie" => "United European Gastroenterol J" "fecha" => "2020" "volumen" => "8" "paginaInicial" => "13" "paginaFinal" => "33" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/32213062" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000016100000006/v1_202309251317/S2387020623003480/v1_202309251317/en/main.assets" "Apartado" => array:4 [ "identificador" => "43309" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Letters to the Editor" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000016100000006/v1_202309251317/S2387020623003480/v1_202309251317/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020623003480?idApp=UINPBA00004N" ]
Journal Information
Vol. 161. Issue 6.
Pages 269-270 (September 2023)
Share
Download PDF
More article options
Vol. 161. Issue 6.
Pages 269-270 (September 2023)
Letter to the Editor
Inflammatory pseudotumor as an atypical presentation of achalasia
Seudotumor inflamatorio como forma de presentación atípica de acalasia
Antonio Bustos-Merlo
, Ana Peragón-Ortega, Antonio Rosales-Castillo
Corresponding author
Servicio de Medicina Interna, Hospital Universitario Virgen de las Nieves, Granada, Spain
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail