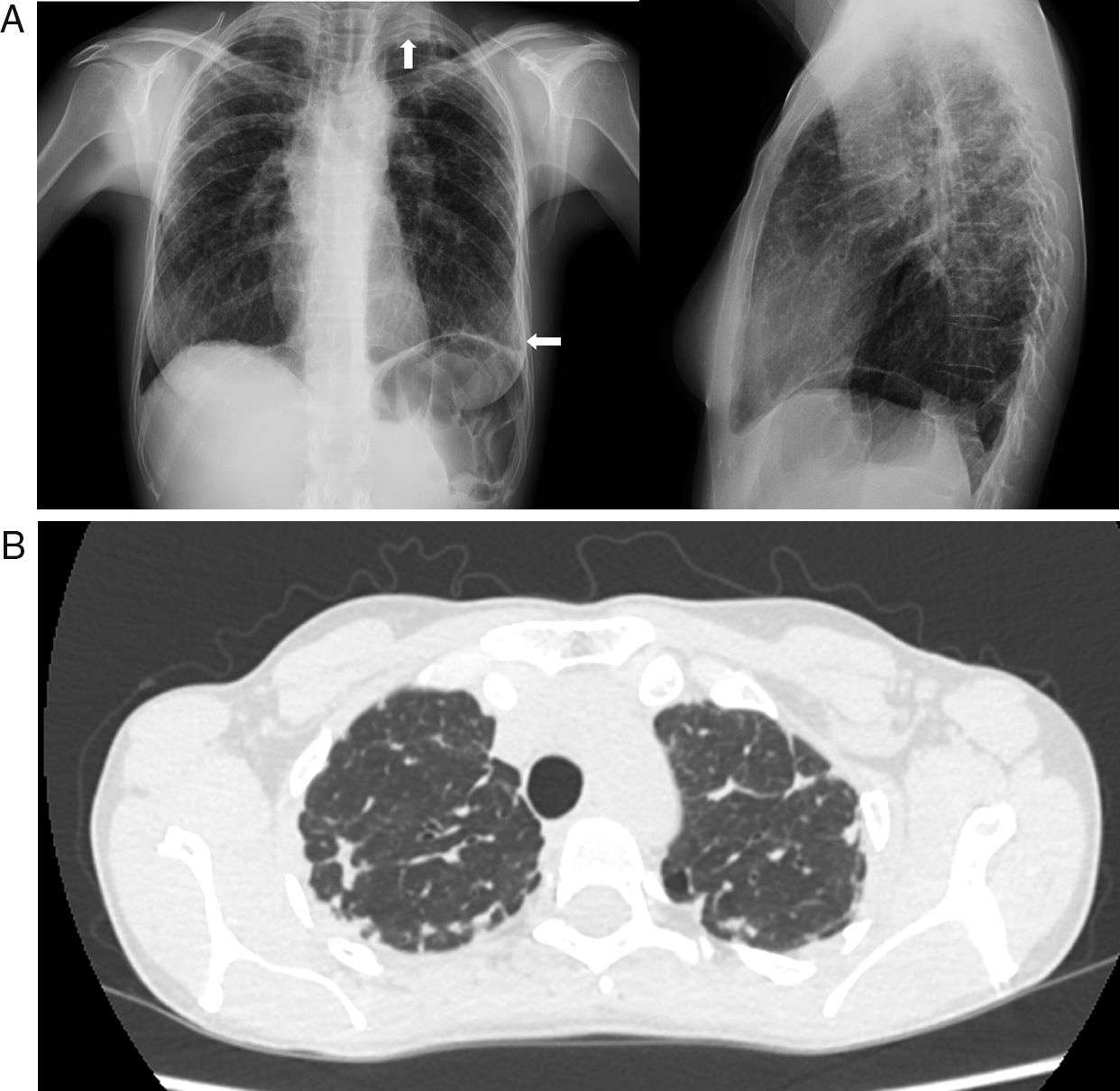
array:24 [ "pii" => "S2387020619301792" "issn" => "23870206" "doi" => "10.1016/j.medcle.2019.04.004" "estado" => "S300" "fechaPublicacion" => "2019-06-21" "aid" => "4571" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2018" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "crp" "cita" => "Med Clin. 2019;152:513-4" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S0025775318304068" "issn" => "00257753" "doi" => "10.1016/j.medcli.2018.06.004" "estado" => "S300" "fechaPublicacion" => "2019-06-21" "aid" => "4571" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "crp" "cita" => "Med Clin. 2019;152:513-4" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:2 [ "total" => 12 "formatos" => array:2 [ "HTML" => 8 "PDF" => 4 ] ] "es" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta científica</span>" "titulo" => "Fibroelastosis pleuropulmonar en una paciente con lupus eritematoso sistémico" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "513" "paginaFinal" => "514" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Pleuropulmonary fibroelastosis in a patient with systemic lupus erythematosus" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Figura 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1210 "Ancho" => 1242 "Tamanyo" => 141407 ] ] "descripcion" => array:1 [ "es" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">A) En la radiografía de tórax de la enferma se observa un engrosamiento pleural (flechas) con pérdida de volumen en los lóbulos superiores y un tórax <span class="elsevierStyleItalic">aplanado</span> en la proyección de perfil.</p> <p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">B) La tomografía computarizada torácica de alta resolución (cortes axiales) demuestra la presencia de un engrosamiento pleural irregular bilateral asociado a cambios de fibrosis (bronquiectasias de tracción, distorsión de la arquitectura pulmonar, reticulación y pérdida de volumen) en los lóbulos superiores.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Isabel Morales-Ivorra, María Molina-Molina, Javier Narváez" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Isabel" "apellidos" => "Morales-Ivorra" ] 1 => array:2 [ "nombre" => "María" "apellidos" => "Molina-Molina" ] 2 => array:2 [ "nombre" => "Javier" "apellidos" => "Narváez" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020619301792" "doi" => "10.1016/j.medcle.2019.04.004" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020619301792?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775318304068?idApp=UINPBA00004N" "url" => "/00257753/0000015200000012/v1_201906070610/S0025775318304068/v1_201906070610/es/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S2387020619301962" "issn" => "23870206" "doi" => "10.1016/j.medcle.2018.07.022" "estado" => "S300" "fechaPublicacion" => "2019-06-21" "aid" => "4636" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2019;152:515-6" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:11 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Multiple pyomyositis secondary to septic thrombophlebitis" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "515" "paginaFinal" => "516" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Piomiositis múltiple secundaria a tromboflebitis séptica" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1244 "Ancho" => 2500 "Tamanyo" => 155048 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Volumetric reconstruction from a SPECT/CT study with <span class="elsevierStyleSup">111</span>In-labeled leukocytes. (A) Fused axial slices of the right thigh that show an area of pyomyositis (thin arrow) and the site of an abscess (thick arrow). (B) Volume rendering that shows an irregular uptake in muscle tissue in yellow-orange color and multiple abscesses (thin arrows). (C) CT axial section of the right thigh showing the site of an abscess (thick arrow).</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Ricardo A. Losno, Sergi Vidal-Sicart, Josep Maria Grau" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Ricardo A." "apellidos" => "Losno" ] 1 => array:2 [ "nombre" => "Sergi" "apellidos" => "Vidal-Sicart" ] 2 => array:2 [ "nombre" => "Josep Maria" "apellidos" => "Grau" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775318305402" "doi" => "10.1016/j.medcli.2018.07.020" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775318305402?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020619301962?idApp=UINPBA00004N" "url" => "/23870206/0000015200000012/v1_201906160657/S2387020619301962/v1_201906160657/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2387020619301949" "issn" => "23870206" "doi" => "10.1016/j.medcle.2019.01.020" "estado" => "S300" "fechaPublicacion" => "2019-06-21" "aid" => "4751" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "crp" "cita" => "Med Clin. 2019;152:508-12" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Diagnosis and treatment</span>" "titulo" => "Endometriosis: Diagnosis and treatment" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "508" "paginaFinal" => "512" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Endometriosis: diagnóstico y tratamiento" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Iñaki Lete" "autores" => array:1 [ 0 => array:2 [ "nombre" => "Iñaki" "apellidos" => "Lete" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S002577531930051X" "doi" => "10.1016/j.medcli.2019.01.005" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S002577531930051X?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020619301949?idApp=UINPBA00004N" "url" => "/23870206/0000015200000012/v1_201906160657/S2387020619301949/v1_201906160657/en/main.assets" ] "en" => array:15 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Scientific letter</span>" "titulo" => "Pleuropulmonary fibroelastosis in a patient with systemic lupus erythematosus" "tieneTextoCompleto" => true "saludo" => "Dear Editor," "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "513" "paginaFinal" => "514" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Isabel Morales-Ivorra, María Molina-Molina, Javier Narváez" "autores" => array:3 [ 0 => array:3 [ "nombre" => "Isabel" "apellidos" => "Morales-Ivorra" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] ] ] 1 => array:3 [ "nombre" => "María" "apellidos" => "Molina-Molina" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] ] ] 2 => array:4 [ "nombre" => "Javier" "apellidos" => "Narváez" "email" => array:1 [ 0 => "fjnarvaez@bellvitgehospital.cat" ] "referencia" => array:2 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] 1 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] ] "afiliaciones" => array:2 [ 0 => array:3 [ "entidad" => "Servicio de Reumatología, Hospital Universitario de Bellvitge, Hospitalet de Llobregat, Barcelona, Spain" "etiqueta" => "a" "identificador" => "aff0005" ] 1 => array:3 [ "entidad" => "Servicio de Neumología, Hospital Universitario de Bellvitge, Hospitalet de Llobregat, Barcelona, Spain" "etiqueta" => "b" "identificador" => "aff0010" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Fibroelastosis pleuropulmonar en una paciente con lupus eritematoso sistémico" ] ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1210 "Ancho" => 1242 "Tamanyo" => 141407 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">(A) On chest X-ray we can notice a pleural thickening (arrows) with volume loss of both upper lobes and a flattened thorax in the profile projection. (B) High resolution chest computed tomography (axial slices) shows the presence of bilateral irregular pleural thickening associated with changes in fibrosis (traction bronchiectasis, lung architectural distortion, reticulation and volume loss) in both upper lobes.</p>" ] ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">Pleuropulmonary fibroelastosis (PPFE) is a rare entity recently included in the group of rare interstitial lung diseases in the latest joint classification of the American Thoracic Society and the European Respiratory Society.<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">1</span></a> It is characterized by prominent fibrosis of the visceral pleura and subpleural parenchyma mainly in both upper lobes.<a class="elsevierStyleCrossRefs" href="#bib0035"><span class="elsevierStyleSup">2,3</span></a> Although it was initially considered as an idiopathic entity, cases have been progressively reported in patients transplanted with bone marrow, lung and after chemotherapy, as well as in patients with different systemic autoimmune diseases (SADs).<a class="elsevierStyleCrossRefs" href="#bib0035"><span class="elsevierStyleSup">2,4</span></a></p><p id="par0010" class="elsevierStylePara elsevierViewall">We present the case report of a patient with FEPP who was subsequently diagnosed with systemic lupus erythematosus (SLE). This is a 39-year-old woman with a history of papillary thyroid carcinoma diagnosed in 1986 and treated with thyroidectomy and radioactive iodine; and an abortion in 2005. In November 2016 she presented an episode of left pneumothorax. After the resolution of the pneumothorax, chest X-ray revealed a pleural thickening with volume loss in both upper lobes (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>a). High resolution chest computed tomography (HRCT) confirmed the presence of bilateral irregular pleural thickening, associated with changes in fibrosis (traction bronchiectasis, lung architectural distortion, reticulation and volume loss) in both upper lobes (<a class="elsevierStyleCrossRef" href="#fig0005">Fig. 1</a>b). In the respiratory functional tests the patient presented a restrictive pattern, with a reduction of total lung capacity and diffusing capacity of the lungs. Upon suspicion of PPFE, a lung biopsy confirmed the diagnosis, showing the presence of fibrosis of the visceral pleura and subpleural and parenchymal fibroelastosis.</p><elsevierMultimedia ident="fig0005"></elsevierMultimedia><p id="par0015" class="elsevierStylePara elsevierViewall">We detected antinuclear antibodies (a titre of 1/320), anti-DNA antibodies and antiphospholipid antibodies (anticardiolipin and beta-2-glycoprotein 1 antibodies), in 2 determinations. In the anamnesis, some of the information gathered was a history of Raynaud's phenomenon for years and recurrence of inflammatory arthralgia. During the first months of follow-up, she presented lesions of acute cutaneous lupus (typical butterfly rash or malar rash), and was finally diagnosed with SLE based on the criteria of the Systemic Lupus International Collaborating Clinics (SLICC) proposed in 2012.<a class="elsevierStyleCrossRef" href="#bib0050"><span class="elsevierStyleSup">5</span></a></p><p id="par0020" class="elsevierStylePara elsevierViewall">Dry cough and dyspnea on exertion are the most frequent form of PPFE clinical presentation.<a class="elsevierStyleCrossRefs" href="#bib0035"><span class="elsevierStyleSup">2,3</span></a> Pneumothorax is a common complication in these patients, being in some cases, as in this one, the first manifestation of the disease.<a class="elsevierStyleCrossRefs" href="#bib0035"><span class="elsevierStyleSup">2,3</span></a> On physical examination, in addition to dry crackles and acropachy, in advanced stages of the disease, these patients may present a thoracic cage deformity in the form of a “flattened thorax”. The diagnosis of this entity is based on the HRCT findings (pleural thickening in both upper lobes, with absence or less involvement of lower lobes) and histopathology (fibrosis of the visceral pleura in upper lobes with prominent and homogeneous intraalveolar fibrosis with alveolar and septal elastosis).<a class="elsevierStyleCrossRefs" href="#bib0035"><span class="elsevierStyleSup">2,3</span></a> The evolution of the disease is variable, presenting a progressive course in 60% of cases. In some cases, the evolution is slowly progressive, while in others there is a rapid clinical worsening, with an overall death rate up to 40%.<a class="elsevierStyleCrossRefs" href="#bib0035"><span class="elsevierStyleSup">2,3</span></a> Currently, no treatment has been proven effective in this disease. Empirically, glucocorticoids, N-acetyl cysteine and different immunosuppressants have been tested, with clear evidence of efficacy.<a class="elsevierStyleCrossRef" href="#bib0035"><span class="elsevierStyleSup">2</span></a> In patients with respiratory failure, oxygen therapy may be useful and, in selected patients, lung transplantation.<a class="elsevierStyleCrossRef" href="#bib0035"><span class="elsevierStyleSup">2</span></a></p><p id="par0025" class="elsevierStylePara elsevierViewall">In conclusion, PPFE is a rare form of interstitial lung disease, recently described and likely underdiagnosed because its knowledge is not widespread yet. In recent years, an increasing number of case reports on this disease associated with different SADs have been published, such as ulcerative colitis, ankylosing spondylitis, rheumatoid arthritis, systemic sclerosis, primary Sjögren's syndrome and polymyositis/dermatomyositis.<a class="elsevierStyleCrossRefs" href="#bib0035"><span class="elsevierStyleSup">2,4</span></a> In a significant number of these cases, the patients were first wrongly diagnosed with usual interstitial pneumonia.<a class="elsevierStyleCrossRef" href="#bib0045"><span class="elsevierStyleSup">4</span></a> Hence the importance of recognizing this entity to raise the degree of clinical suspicion and allow a proper diagnosis and therapeutic management by a multidisciplinary team.</p></span>" "pdfFichero" => "main.pdf" "tienePdf" => true "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Morales-Ivorra I, Molina-Molina M, Narváez J. Fibroelastosis pleuropulmonar en una paciente con lupus eritematoso sistémico. Med Clin (Barc). 2019;152:513–514.</p>" ] ] "multimedia" => array:1 [ 0 => array:7 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1210 "Ancho" => 1242 "Tamanyo" => 141407 ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">(A) On chest X-ray we can notice a pleural thickening (arrows) with volume loss of both upper lobes and a flattened thorax in the profile projection. (B) High resolution chest computed tomography (axial slices) shows the presence of bilateral irregular pleural thickening associated with changes in fibrosis (traction bronchiectasis, lung architectural distortion, reticulation and volume loss) in both upper lobes.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0015" "bibliografiaReferencia" => array:5 [ 0 => array:3 [ "identificador" => "bib0030" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "W.D. Travis" 1 => "U. Costabel" 2 => "D.M. Hansell" 3 => "T.E. King Jr." 4 => "D.A. Lynch" 5 => "A.G. Nicholson" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1164/rccm.201308-1483ST" "Revista" => array:6 [ "tituloSerie" => "Am J Respir Crit Care Med" "fecha" => "2013" "volumen" => "188" "paginaInicial" => "733" "paginaFinal" => "748" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/24032382" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0035" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Fibroelastosis pleuropulmonar: ¿es también una entidad idiopática?" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "K. Portillo" 1 => "I. Guasch Arriaga" 2 => "J. Ruiz-Manzano" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.arbres.2015.05.002" "Revista" => array:6 [ "tituloSerie" => "Arch Bronconeumol" "fecha" => "2015" "volumen" => "51" "paginaInicial" => "509" "paginaFinal" => "514" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/26099364" "web" => "Medline" ] ] ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0040" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Idiopathic pleuroparenchymal fibroelastosis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "M. Bonifazi" 1 => "M.A. Montero" 2 => "E.A. Renzoni" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1007/s13665-017-0160-5" "Revista" => array:6 [ "tituloSerie" => "Curr Pulmonol Rep" "fecha" => "2017" "volumen" => "6" "paginaInicial" => "9" "paginaFinal" => "15" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28344924" "web" => "Medline" ] ] ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0045" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Radiologic pleuroparenchymal fibroelastosis-like lesion in connective tissue disease-related interstitial lung disease" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "Y. Enomoto" 1 => "Y. Nakamura" 2 => "T.V. Colby" 3 => "T. Johkoh" 4 => "H. Sumikawa" 5 => "K. Nishimoto" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1371/journal.pone.0180283" "Revista" => array:5 [ "tituloSerie" => "PLOS ONE" "fecha" => "2017" "volumen" => "12" "paginaInicial" => "e0180283" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/28666014" "web" => "Medline" ] ] ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0050" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "M. Petri" 1 => "A.M. Orbai" 2 => "G.S. Alarcón" 3 => "C. Gordon" 4 => "J.T. Merrill" 5 => "P.R. Fortin" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1002/art.34473" "Revista" => array:6 [ "tituloSerie" => "Arthritis Rheum" "fecha" => "2012" "volumen" => "64" "paginaInicial" => "2677" "paginaFinal" => "2686" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/22553077" "web" => "Medline" ] ] ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000015200000012/v1_201906160657/S2387020619301792/v1_201906160657/en/main.assets" "Apartado" => array:4 [ "identificador" => "43311" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Scientific letters" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000015200000012/v1_201906160657/S2387020619301792/v1_201906160657/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020619301792?idApp=UINPBA00004N" ]
Journal Information
Vol. 152. Issue 12.
Pages 513-514 (June 2019)
Share
Download PDF
More article options
Vol. 152. Issue 12.
Pages 513-514 (June 2019)
Scientific letter
Pleuropulmonary fibroelastosis in a patient with systemic lupus erythematosus
Fibroelastosis pleuropulmonar en una paciente con lupus eritematoso sistémico
Visits
3
This item has received
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail