Patients with Systemic Lupus Erythematosus (SLE) have an increased risk of metabolic syndrome (MS) and cardiovascular disease (CVD). MS is evaluated binary, limiting the understanding of each component's severity individually. Therefore, severity scores for MS that evaluate them separately have been developed. This study aims to determine the prognosis between MS severity and the occurrence of major adverse cardiovascular events (MACE) in SLE patients.
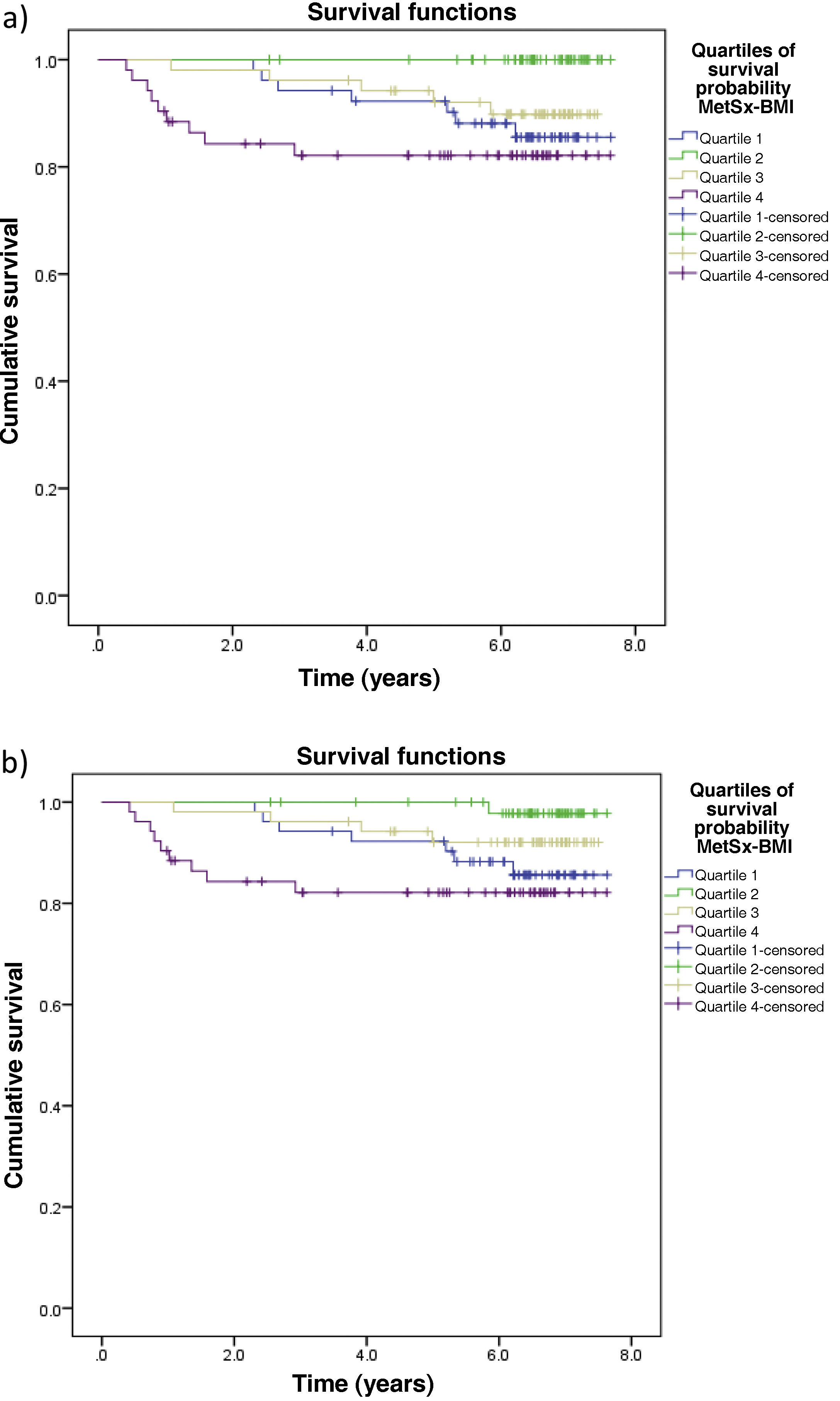
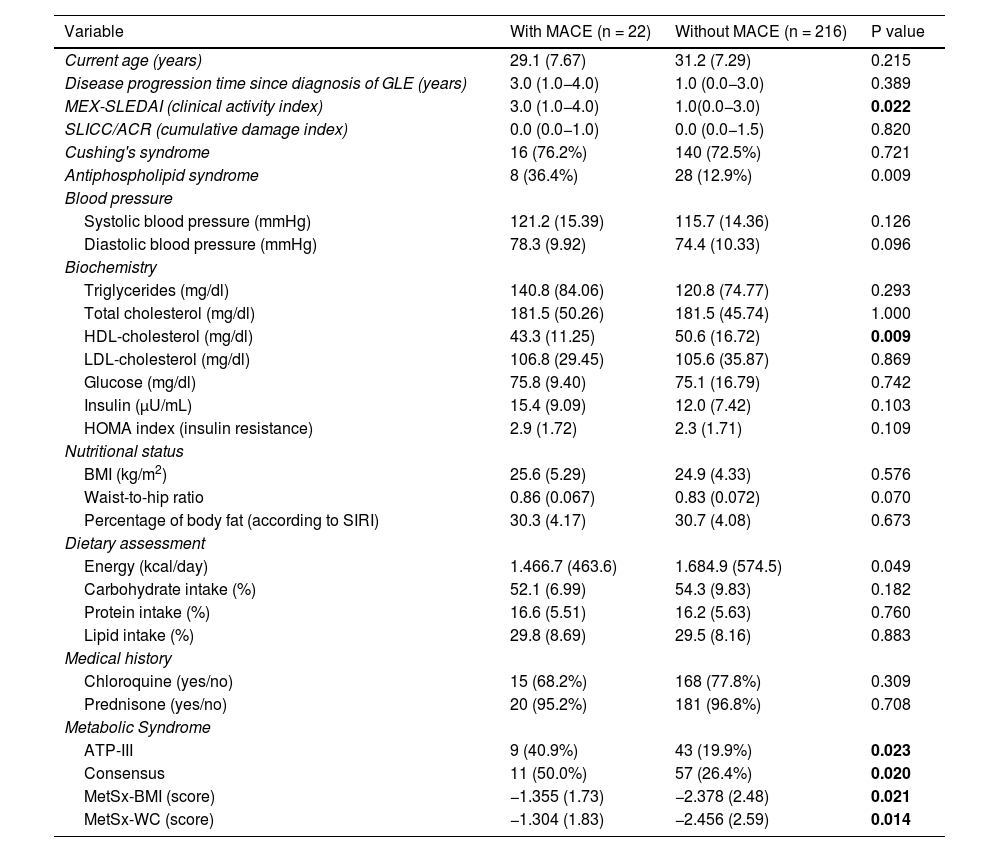
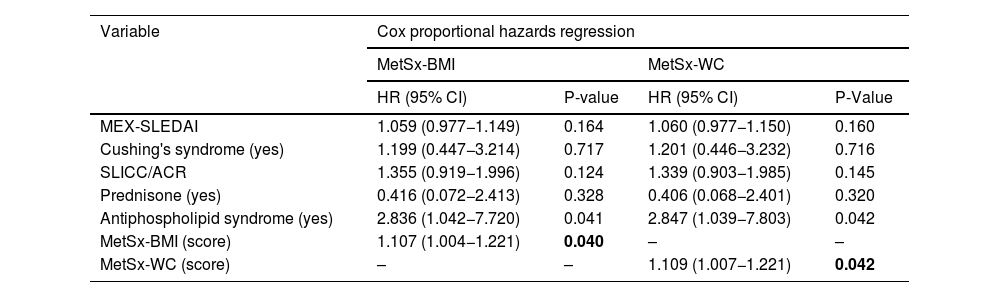
Methods10-year follow-up cohort study. Premenopausal >18-year-old women with a previous diagnosis of SLE were included. Patients with recent cardiovascular (CV) events, pregnancy, thyroid disease, and liposuction were excluded. The variables of interest were CV events, the confounding variables, and the MS severity indexes were examined. Hazard ratios and Kaplan–Meier survival curves were estimated through Cox regression.
Results238 women were analyzed; 22 presented MACE, and 216 did not. MS prevalence, measured according to Consensus and ATPII criteria, was higher in MACE patients (50% and 40,95%, respectively). The MetSx-IMC severity index was higher within the MACE group. COX analysis showed an increase in the MetSX-IMC associated with the risk of suffering MACE in a 1,107 ratio.
ConclusionsThe MetSx-IMC severity index, contrary to the binary approaches, is suggested to evaluate MS as a predictor of MACE in SLE patients. Offering improved and more accurate prognosis in patients at risk of developing MCE.
Los pacientes con lupus eritematoso sistémico (LES) tienen mayor riesgo de síndrome metabólico (SM) y enfermedad cardiovascular. El SM se evalúa de forma binaria, limitando la comprensión de la gravedad de los componentes por separado. Por lo anterior, se han desarrollado puntajes de gravedad de SM evaluándose individualmente. Este estudio tiene como objetivo determinar el pronóstico entre la gravedad de SM y el desarrollo de evento cardiovascular mayor (ECM) en pacientes con LES.
Metodologíaestudio de cohorte con seguimiento de 10 años, incluyendo mujeres premenopáusicas >18 años con LES. Se excluyeron pacientes con ECV, embarazo, enfermedad tiroidea y liposucción. La variable de interés fue ECV, y se examinaron las variables confusoras y los índices de gravedad de SM. Se estimaron las curvas de supervivencia de Kaplan–Meier y los cocientes de Hazard (HR) a través de la regresión de Cox.
ResultadosSe analizaron 238 mujeres: 22 presentaron ECM y 216 no. La prevalencia de SM, evaluada según los criterios de Consenso y ATPIII, fue mayor en pacientes con ECM (50% y 40,9%, respectivamente). El índice de gravedad MetSx-IMC fue más alto en el grupo de ECM. El análisis de COX, demostró incremento en el MetSx-IMC, asociándose al aumento del riesgo de experimentar ECM en un factor de 1,107.
ConclusionesEl índice de gravedad MetSx-IMC, contrario a los enfoques binarios, se sugiere para evaluar el SM como predictor de ECM en pacientes con LES. Ofreciendo mayor capacidad pronóstica y precisa de pacientes en riesgo de desarrollar ECM.