Prognostic scales can be helpful for selecting patients for reperfusion treatment. This study aims to assess the prognostic ability of the recently published SPAN-100 index in a large cohort of stroke patients treated with intravenous thrombolysis (IV rtPA).
MethodsUsing data from the prospective registry of all reperfusion treatments administered in Catalonia, we selected patients treated with IV rtPA alone between 2011 and 2012. The SPAN-100 index was calculated as the sum of age (years) and NIHSS score, and patients in the cohort were classified as SPAN-100 positive [≥100] or SPAN-100 negative [<100]. We measured raw and adjusted rates of symptomatic intracerebral haemorrhage (SICH), mortality, and 3-month functional outcome (mRS 0-2) for each SPAN-100 category. Area under the ROC curve was calculated to predict the main outcome measures.
ResultsWe studied 1685 rtPA-treated patients, of whom 1405 (83%) were SPAN-100 negative. The SICH rates adjusted for sex, pre-stroke mRS, hypertension, diabetes, dyslipidaemia, ischaemic heart disease, heart failure, atrial fibrillation, prior TIA/stroke and time to thrombolysis did not differ between groups, but likelihood of functional independence (mRS 0-2) at 3 months was nearly 8 times higher in the SPAN-100 negative group than in the positive group. Furthermore, the 3-month mortality rate was 5 times higher in the SPAN-100 positive group. ROC curve analysis showed high specificities for predicting both functional independence and 3-month mortality for a cut-off point of 100.
ConclusionThe SPAN-100 index is a simple and straightforward method that may be useful for selecting candidates for rtPA treatment in doubtful cases, and for informing patients and their relatives about likely outcomes.
Las escalas pronósticas pueden ayudar a seleccionar pacientes para tratamientos de reperfusión. Objetivo: aplicar el índice SPAN-100 en una cohorte de pacientes tratados con rtPA por vía intravenosa y evaluar su capacidad pronóstica.
MétodosSe utilizaron datos del registro prospectivo de reperfusión de Cataluña y se seleccionaron casos consecutivos que recibieron rtPA por vía intravenosa aislado en 2011-2012. A partir del sumatorio de edad y NIHSS se categorizó la cohorte en SPAN-100 positivos [≥ 100] y SPAN-100 negativos [< 100 puntos]. Se determinaron las tasas crudas y ajustadas de hemorragia sintomática (HICS), muerte e independencia funcional (ERm 0-2) a partir del índice SPAN-100 y se calculó la curva ROC para la predicción de las principales medidas de resultado.
ResultadosDe los 1.685 casos incluidos, 1.405 (83%) eran SPAN-100 negativos. La tasa de HICS ajustada por sexo, ERm preictus, hipertensión, diabetes, dislipemia, cardiopatía isquémica, insuficiencia cardíaca, fibrilación auricular, ictus/AIT previos y tiempo hasta la trombólisis no fue diferente según las dos categorías pero la probabilidad de tener una ERm 0-2 al 3.er mes fue hasta casi 8 veces mayor entre los SPAN-100 negativos. El riesgo de muerte al 3.er mes fue 5 veces superior en los SPAN-100 positivos. El análisis ROC mostró especificidades altas tanto en la predicción de independencia funcional como mortalidad al 3.er mes cuando el punto de corte era de 100.
ConclusionesEl índice SPAN-100 es un índice sencillo y de fácil aplicación que puede guiar la selección de pacientes para trombólisis cuando existen dudas razonables y asesorar al paciente/familia acerca de los resultados esperables.
Intravenous tissue plasminogen activator (IV rtPA) is the only reperfusion treatment proven effective for acute ischaemic stroke (AIS).1–3 However, not all patients with AIS show a satisfactory response to thrombolytic treatment; only half achieve revascularisation, which has repeatedly been linked to a favourable functional outcome (modified Rankin Scale [mRS] scores 0-2) at 3 months.4,5 Numerous factors affect outcomes after IV rtPA, especially age, baseline stroke severity, and time to treatment.3,6–8 There is a growing need for new prognostic scales or indexes to predict stroke outcomes. On the one hand, clinicians need to determine patients’ prognoses due to the undisputed importance of this factor in their decision-making process. In clinical practice, time is a fundamental variable for acute stroke and treatment is increasingly complex, which requires neurologists to decide as quickly as possible whether or not the patient should be treated. On the other hand, families also need prognostic information in order to adapt the living environment before the patient is discharged. In recent years, evidence of the benefit of prognostic scales or indexes has been mounting. In current routine use of IV rtPA, eligibility criteria are less strict than the inclusion criteria used in the original clinical trials9–11; prognostic indexes are especially useful in cases of off-label IV rtPA administration. The purpose of this study was to determine the ability of the SPAN-100 index to predict clinical outcomes in a prospective cohort of consecutive patients treated with IV rtPA.
Patients and methodsStudy design and populationThis observational study included a prospective cohort of consecutive patients with AIS treated with IV rtPA in reference hospitals (n=14), and in regional hospitals using the Teleictus virtual consult system (n=3), in Catalonia between 1 January 2011 and 31 December 2012. As of January 2011, all patients with AIS in Catalonia receiving reperfusion treatment (IV rtPA alone, IV rtPA followed by endovascular rescue therapy) must be included in the online database SONIIA. These data are managed by the Stroke Programme for Catalonia, which also analyses data and sends clinicians a quarterly newsletter with database information. In addition, the Stroke Programme for Catalonia monitors the representativeness of the sample using a complex external auditing process to minimise inclusion biases. Therefore, all undiagnosed cases of stroke detected by the external audit will be included retrospectively in the SONIIA database. This study included patients treated with IV rtPA alone (excluding those who received endovascular rescue therapy) between 2011 and 2012.
Data were collected prospectively and included a set of clinical and radiological variables. We gathered the following baseline data: age, sex, medical history, and functional status before stroke. Clinical variables included stroke onset, time of arrival at the hospital, stroke severity (NIHSS score), and time beginning thrombolytic therapy. At 24-36hours, we recorded neurological status (NIHSS score), presence of symptomatic intracerebral haemorrhage (SICH) as defined by SITS-MOST criteria,12 and survival. At 3 months, we recorded survival and functional status according to the mRS; this scale was administered in in-person or telephone interviews conducted by expert clinicians.
The SONIIA database complies with current data protection regulations. All participants signed informed consent forms.
Outcome variablesThe outcome variables analysed in this study are: (1) SICH rate, defined as the percentage of patients experiencing SICH (SITS-MOST criteria12) in the first 24-36hours after stroke; (2) cumulative mortality at 3 months; and (3) functional independence at 3 months (mRS 0-2).
Statistical analysisThe SPAN-100 index combines the age in years and baseline NIHSS score for a given patient. According to a previous study, SPAN-100–positive patients (age+NIHSS score>100 total points) tend to have poorer prognoses.13 After classifying the study population as either SPAN-100–positive or SPAN-100–negative, we compared raw and adjusted rates of SICH, mortality, and functional independence between groups and determined the area under the ROC curve to predict outcomes based on the SPAN-100 index. Multivariate models for functional independence and mortality at 3 months were adjusted by sex, mRS score before stroke, hypertension, diabetes, dyslipidaemia, ischaemic heart disease, heart failure, atrial fibrillation, history of stroke/TIA, and time to treatment.
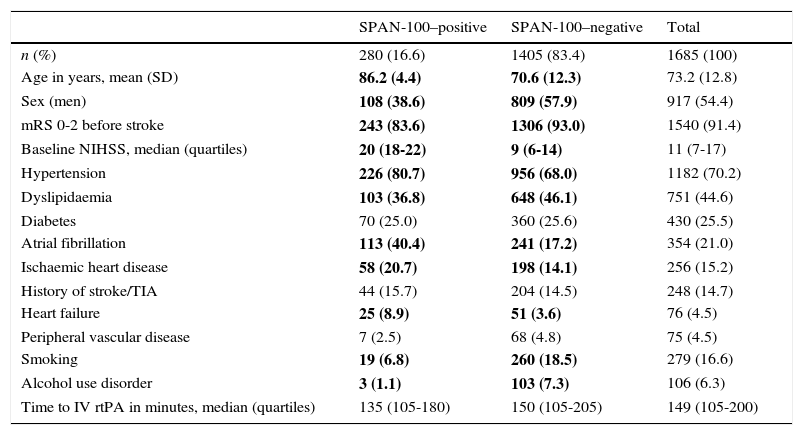
ResultsDuring the study period, 1685 patients with AIS were treated with IV rtPA; 1405 of them (83.4%) were classified as SPAN-100–negative. Table 1 shows the baseline characteristics of the study population. Disregarding age and baseline NIHSS scores (the variables used to define and distinguish between positive and negative SPAN-100 groups, with no overlaps) the SPAN-100–negative group included a greater percentage of men, patients functionally independent before stroke, and patients with dyslipidaemia, and a lower percentage of patients with hypertension, atrial fibrillation, ischaemic heart disease, and heart failure. However, we found a significantly higher percentage of smokers and alcoholic patients in the SPAN-100–negative group.
Baseline characteristics of the study population by SPAN-100 category.
| SPAN-100–positive | SPAN-100–negative | Total | |
|---|---|---|---|
| n (%) | 280 (16.6) | 1405 (83.4) | 1685 (100) |
| Age in years, mean (SD) | 86.2 (4.4) | 70.6 (12.3) | 73.2 (12.8) |
| Sex (men) | 108 (38.6) | 809 (57.9) | 917 (54.4) |
| mRS 0-2 before stroke | 243 (83.6) | 1306 (93.0) | 1540 (91.4) |
| Baseline NIHSS, median (quartiles) | 20 (18-22) | 9 (6-14) | 11 (7-17) |
| Hypertension | 226 (80.7) | 956 (68.0) | 1182 (70.2) |
| Dyslipidaemia | 103 (36.8) | 648 (46.1) | 751 (44.6) |
| Diabetes | 70 (25.0) | 360 (25.6) | 430 (25.5) |
| Atrial fibrillation | 113 (40.4) | 241 (17.2) | 354 (21.0) |
| Ischaemic heart disease | 58 (20.7) | 198 (14.1) | 256 (15.2) |
| History of stroke/TIA | 44 (15.7) | 204 (14.5) | 248 (14.7) |
| Heart failure | 25 (8.9) | 51 (3.6) | 76 (4.5) |
| Peripheral vascular disease | 7 (2.5) | 68 (4.8) | 75 (4.5) |
| Smoking | 19 (6.8) | 260 (18.5) | 279 (16.6) |
| Alcohol use disorder | 3 (1.1) | 103 (7.3) | 106 (6.3) |
| Time to IV rtPA in minutes, median (quartiles) | 135 (105-180) | 150 (105-205) | 149 (105-200) |
Data are expressed in n (%) unless otherwise indicated. Values in bold indicate statistical significance (P<.05).
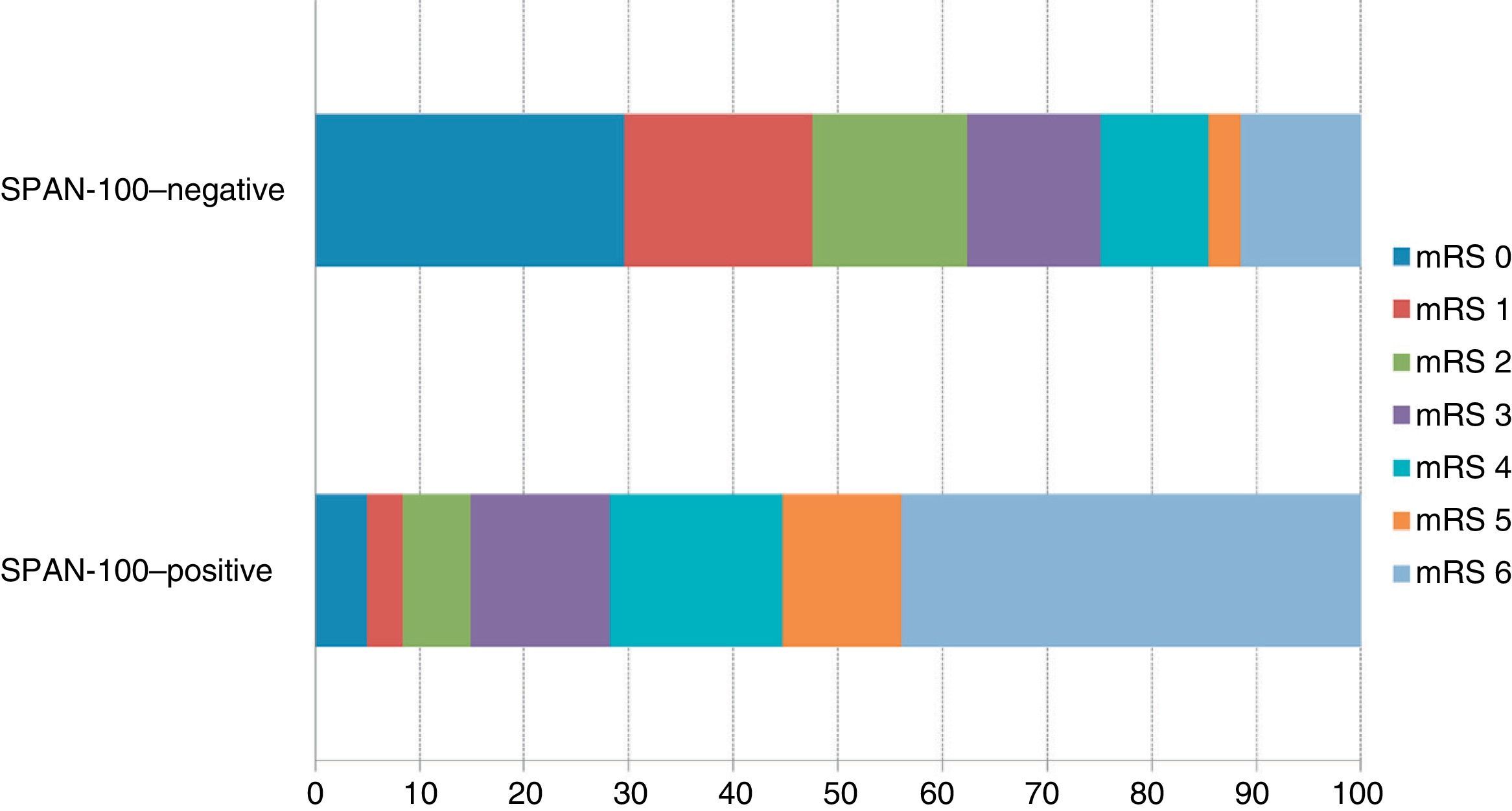
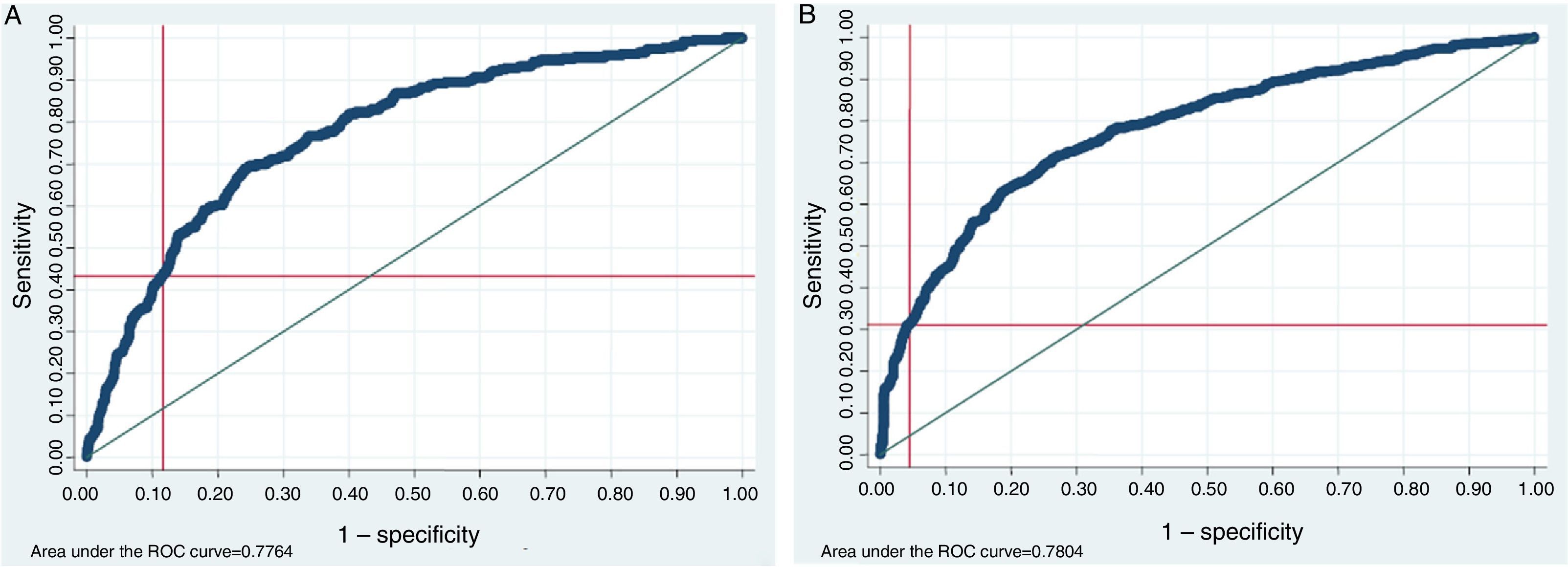
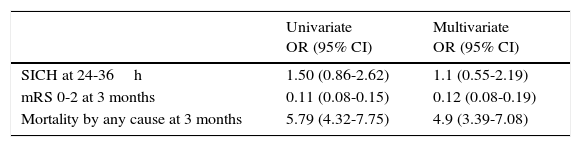
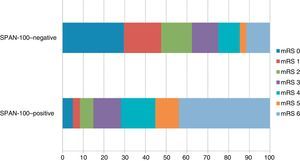
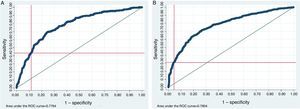
The distribution of mRS scores at 3 months shows significant differences between the 2 SPAN-100 groups in terms of functional status and mortality at 3 months (Fig. 1). Regarding raw and adjusted rates of outcome variables, the SPAN-100–positive group displayed a significantly lower probability of achieving functional independence at 3 months and a 5-times higher risk of mortality (Table 2). ROC analysis revealed an area under the curve of 0.78 for predicting either mortality or functional independence at 3 months. Using a value of 100 on the SPAN-100 index as its cut-off point, the ROC analysis showed low sensitivity (mRS 0-2: 0.31; mortality: 0.42) and high specificity (mRS 0-2: 0.95; mortality: 0.88) (Fig. 2).
Risk of SICH, mortality, and functional independence in the SPAN-100–positive group.
| Univariate OR (95% CI) | Multivariate OR (95% CI) | |
|---|---|---|
| SICH at 24-36h | 1.50 (0.86-2.62) | 1.1 (0.55-2.19) |
| mRS 0-2 at 3 months | 0.11 (0.08-0.15) | 0.12 (0.08-0.19) |
| Mortality by any cause at 3 months | 5.79 (4.32-7.75) | 4.9 (3.39-7.08) |
The SPAN-100–negative group is set as a reference. Multivariate models are adjusted by sex, mRS score before stroke, hypertension, diabetes, dyslipidaemia, ischaemic heart disease, heart failure, atrial fibrillation, history of stroke/TIA, and time to treatment.
The purpose of our study was to apply the SPAN-100 index (baseline NIHSS score and age in years) to an independent sample of patients treated with IV rtPA and describe its predictive ability for clinical outcomes after treatment. In line with results of the study by Saposnik et al.13 published in early 2013, we found that patients in the SPAN-100–positive group (age+NIHSS score>100) were at a higher risk of death and disability (mRS>3) at 3 months than SPAN-100–negative patients. In addition, the ROC curve analysis shows that the SPAN-100 index has a good predictive ability (with an area under the curve of 0.78) for predicting both functional status and mortality at 3 months.
Several clinical and demographical variables, including age,8,14 severity at onset,8,15 comorbidities before stroke,16 baseline glycaemia,17,18 and time to treatment,3 have demonstrated a good predictive ability for stroke outcomes. As a result, most predictive indexes or scales for stroke outcome list a combination of these factors. In patients with AIS, prompt diagnosis and decision-making about treatment is essential. The use of a predictive scale or tool, and whether or not it becomes widespread, therefore depends not only on the tool's metric characteristics, but also on whether it is easy and quick to administer. Applying the currently available prognostic tools and indexes (iScore, DRAGON, ASTRAL, and HAT score) is a complex task since it depends on how the stroke subtype is determined by the neurologist, initial neuroimaging studies, etc. This limits large-scale use of these tools.13,19–24 In early 2013, the results of a new prognostic tool, the SPAN-100 index, were published; SPAN-100 results are calculated using age and baseline NIHSS scores only. There are obvious advantages to working with a predictive scale which is easy to remember and whose results can be calculated mentally in a few seconds. The study by Saposnik et al.13 analysed the ability of this scale to predict short- and long-term clinical outcomes, including risk of haemorrhagic complication. Our data does not show the SPAN-100 index to have a good predictive ability for risk of SICH, although this may be due to the low statistical power in our sample in which only 5.8% had SICH, or to differences in how SICH was defined in each of the studies. In line with this idea, the original study used the NINDS definition of SICH: the presence of blood in cranial CT images at 24hours or at 7 to 10 days after stroke, plus worsening of neurological symptoms. In our study, SICH was defined according to SITS-MOST criteria, including presence of local or remote parenchymal haematoma type 2 shown by the 22-36hours post-treatment imaging scan, combined with neurological deterioration (increase of 4 points or more compared to NIHSS score at 24h) or any fatal haemorrhage.2 Our data, however, do show that the SPAN-100 index is able to discriminate between survivors and non-survivors as well as between functionally independent and dependent patients at 3 months. In both cases, SPAN-100 scores >100 at baseline predicted a lower probability of positive outcomes.
We will now briefly cover the analysis of the ROC curve and sensibility and specificity data. At first it may seem that the low sensitivity of the SPAN-100 index for predicting dependence (0.32) and death (0.44) constitutes a drawback. However, the SPAN-100 index is a prognostic rather than a diagnostic tool in this case, used as a decision-making aid in cases in which treatment may be unclear, or to inform patients and/or their families on stroke prognosis after treatment. The goal in our case is to minimise the number of patients with false positives (cases in which the SPAN-100 index mistakenly identifies patients likely to achieve good outcomes after thrombolysis as patients with a poor prognosis), especially when the decision of not to treat depends on prognosis. The high specificity associated with the SPAN-100 cut-off point in our sample indicates a low number of false positives. These characteristics support using this index to help determine whether IV rtPA is suitable for patients who do not meet traditional treatment criteria. In these circumstances, the SPAN-100 index may improve therapeutic performance (clinical outcomes of treated patients) by identifying patients with better prognoses so that patients likely to benefit from IV rtPA treatment will receive it despite having SPAN-100 scores above 100. In any case, this tool cannot replace current patient selection criteria for thrombolysis, which have been tested experimentally. Selection must therefore be supported by the traditional criteria; basing treatment decisions on the SPAN-100 index alone does not seem prudent even in cases for which the tool provides valid prognostic data.
Our study's main limitation is its lack of a control group with which to compare the prognostic performance of the SPAN-100 index; this aspect was covered in the original study by Saposnik et al.13 Despite the above, we feel that our results support the use of the SPAN-100 index to categorise and quantify data based on such well-known prognostic variables as age and baseline stroke severity. Our study sample does not come from a single hospital: it includes all patients receiving isolated intravenous thrombolytic treatment in Catalonia between 2011 and 2012. Our results therefore represent routine clinical practice, unlike those from the original study, which was based on data from the NINDS clinical trial.1 The representative nature of our data relies on the SONIIA database, which was created in January 2011 and must be used by all hospitals, and on external audits, which guarantee inclusion of all consecutive cases. Although the total number of intravenous thrombolytic treatments administered during the study period was 2032, corresponding to a total treatment rate of 13%, we included only those patients receiving IV rtPA and no other treatments in order to have a more homogeneous sample in terms of baseline severity and treatment management.
ConclusionsIn routine clinical practice, prognostic indices which are easy to remember and quick to administer to patients with AIS in the emergency department may be extremely helpful for selecting patients eligible for IV rtPA in unclear cases (off-label use) and to inform patients and/or their families about clinical prognosis.
Conflict of interestThe authors have no conflict of interest to declare.
This study was made possible by the participation of a great number of clinicians from the emergency departments of every hospital in Catalonia and professionals working for the emergency services.
Members of the Catalan Code Stroke and Reperfusion Consortium (Cat-SCR). Hospital Arnau de Vilanova (Lleida): Jordi Sanahuja, Francisco Purroy; Hospital Doctor Josep Trueta (Girona): Joaquín Serena, Mar Castellanos, Yolanda Silva, Cecile van Eendenburg; Hospital Joan XXIII (Tarragona): Anna Pellisé, Xavier Ustrell, Rafael Marés; Hospital Verge de la Cinta (Tortosa): Juanjo Baiges, Moisés Garcés; Hospital Fundació Althaia (Manresa): Júlia Saura, Josep Maria Soler Insa; Hospital General de Vic (Vic): Josep Maria Aragonés; Hospital General de Granollers (Granollers): Pilar Otermin, Dolores Cocho; Hospital de Mataró (Mataró): Ernest Palomeras; Hospital Universitari Germans Trias i Pujol (Badalona): Antoni Dávalos, Mònica Millán, Natalia Pérez de la Ossa, Meritxell Gomis, Elena López-Cancio, Laura Dorado, Carlos Castaño, Pablo García-Bermejo; Hospital Universitari Vall d’Hebron (Barcelona): José Álvarez-Sabín, Marc Ribó, Marta Rubiera, Esteban Santamarina, Jorge Pagola, Carlos Molina, Alejandro Tomasello, Pilar Coscojuela; Hospital Universitari de Bellvitge (L’Hospitalet): Helena Quesada, Lluis Cano, Pere Cardona, Francisco Rubio, Lucía Aja, María Ángeles de Miquel, Paloma Mora; Hospital Clínic i Provincial (Barcelona): Ángel Chamorro, Víctor Obach, Álvaro Cervera, Sergio Amaro, Xabier Urra, Juan M. Macho, Jordi Blasco-Andaluz, Luis San Roman; Hospital de Sant Pau (Barcelona): Joan Martí-Fàbregas, Raquel Delgado-Mederos, Lavinia Dinia, David Carrera-Giraldo; Hospital del Mar (Barcelona): Jaume Roquer, Ana Rodríguez-Campello, Ángel Ois, Elisa Cuadrado-Godia, Elio Vivas; Hospital del Parc Taulí (Sabadell): David Cánovas, Maria del Carmen García, Jordi Estela, Joan Perendreu; Hospital Mútua de Terrassa (Terrassa): Jerzy Krupinski, Sonia Huertas-Folch, M. Carme Nicolás-Herrerias; Hospital Moisès Broggi (Sant Joan Despí): Manuel Gómez-Choco, Sonia García, Raul Martínez; Stroke Programme (Health Department of Catalonia): Miquel Gallofré, Sònia Abilleira.
Further information about the members of this group is shown in Appendix A.
Please cite this article as: Abilleira S, Ribera A, Quesada H, Rubiera M, Castellanos M, Vargas M, et al. Aplicabilidad del índice SPAN-100 en una cohorte prospectiva y contemporánea de pacientes tratados con rtPA por vía intravenosa en Cataluña. Neurología. 2016;31:592–598.