Chronic migraine (CM) is a complication of episodic migraine, favoured by risk factors as medication overuse (MO). We intend to compare demographic and clinic characteristics of a series of CM patients, with and without MO.
MethodsThe study included patients with CM (2006 revised criteria) attended in a headache outpatient office located in a tertiary hospital between January 2008 and May 2012. We recorded demographic characteristics, age at migraine onset, time from onset, previous use of symptomatic or preventive therapy, and headache impact measured with six-item headache impact test (HIT-6).
ResultsA total of 434 patients (357 women, 77 men) were diagnosed with CM out of the 1868 (23.2%) that attended our clinic. Of these, 258 (72.2%) fulfilled criteria of MO, and 59.8% of those with MO, and 41.1% of cases without MO had previously received preventative treatment (P<0.001). Age at onset of migraine was lower in MO patients (21.2±10.1 vs 23.8±12.5 years, P=0.02) and time from onset to headache clinic consultation was higher in MO cases (23.8±14.1 vs 18.3±14.8 years, P<0.001). We found no difference between both groups in average HIT-6 score and the percentage of patients with a HIT-6 score over 55.
ConclusionsCM, with or without MO, is a burdensome group of patients in our headache clinic. Patients with MO are referred later and have more frequently received preventive treatments.
La migraña crónica (MC) es una evolución de la migraña episódica favorecida por factores de riesgo, entre los que se encuentra el uso excesivo de medicación (UEM). Pretendemos comparar características clínicas y demográficas de una serie de casos de MC, con y sin UEM.
MétodosPacientes con MC (criterios revisados 2006) atendidos en una consulta monográfica de cefaleas de un hospital terciario entre enero del 2008 y mayo del 2012. Recogimos datos demográficos, evolución, utilización previa de preventivos e impacto de la migraña medido con la escala HIT-6.
ResultadosCuatrocientos treinta y cuatro pacientes (357 mujeres, 77 varones) fueron diagnosticados de MC entre un total de 1,868 (23,2%) atendidos en la mencionada consulta durante el periodo de inclusión. Doscientos cincuenta y ocho (72,2%) presentaban UEM. El 59,8% de los casos con UEM recibieron previamente tratamiento preventivo frente al 41,1% sin UEM (p<0,001). La edad de inicio de la migraña fue menor en los pacientes con UEM (21,2±10,1 vs. 23,8±12,5 años; p=0,02) y el tiempo de evolución al llegar a nuestra consulta mayor en los pacientes con UEM (23,8±14,1 vs. 18,3±14,8 años; p<0,001). No encontramos diferencia en la puntuación HIT-6 o el porcentaje de casos con HIT-6 mayor de 55 entre ambos grupos.
ConclusionesLa MC con o sin UEM es una afección frecuente y discapacitante en una consulta de cefaleas. En nuestra población, los pacientes con UEM llegan a la consulta tras una evolución más larga, en la que ya recibieron tratamientos preventivos.
Chronic migraine (CM) is an important cause of disability and has a negative impact on patients’ professional, social, and family lives. Diagnostic criteria have evolved over the years, and some descriptions dating back to the second century CE resemble what is recognised today as CM.1
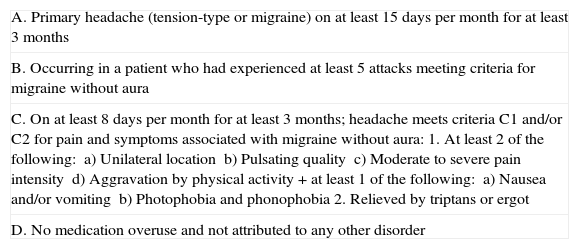
In 1982, the concept of ‘transformed migraine’ was introduced to refer to progression from episodic migraine (EM) to CM.2 The first diagnostic criteria for CM were proposed in 1996.3 The International Classification of Headache Disorders, second edition (ICHD-II), published in 2004, lists CM among complications of migraine, and provides very strict diagnostic criteria for that entity which many authors consider to be impractical.4 In 2006, the International Headache Society proposed new criteria, which were well-received by the scientific and medical communities (Table 1).5,6 These criteria have been revised for the recently published International Classification of Headache Disorders, third edition (ICHD-III).7
Revised diagnostic criteria for CM (ICHD-II, 2006)
| A. Primary headache (tension-type or migraine) on at least 15 days per month for at least 3 months |
| B. Occurring in a patient who had experienced at least 5 attacks meeting criteria for migraine without aura |
| C. On at least 8 days per month for at least 3 months; headache meets criteria C1 and/or C2 for pain and symptoms associated with migraine without aura:1. At least 2 of the following:a) Unilateral locationb) Pulsating qualityc) Moderate to severe pain intensityd) Aggravation by physical activity+ at least 1 of the following:a) Nausea and/or vomitingb) Photophobia and phonophobia2. Relieved by triptans or ergot |
| D. No medication overuse and not attributed to any other disorder |
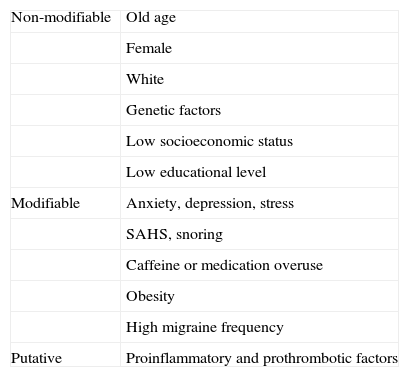
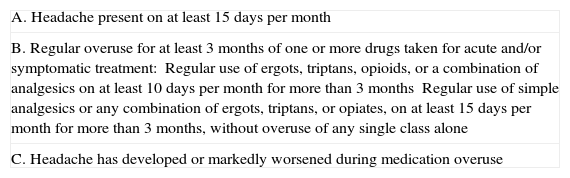
Several modifiable and non-modifiable risk factors predisposing individuals to CM have been described (Table 2). One of the best known and most frequent risk factors is symptomatic medication overuse (MO).8 In 2006, the definition and diagnostic criteria for medication-overuse headache (MOH) were also revised: it is now possible to diagnose MOH during MO, whereas the 2004 criteria required observation of improvement after discontinuing drug therapy (Table 3). However, the revised criteria of 2006 did not identify an association between MOH and CM.6 Based on our clinical practice, we support the widespread recommendation of assigning an initial diagnosis of CM, and later checking for MO since it is one of the potential risk factors for developing CM.9 ICHD-III criteria now include the possibility that MO may be associated with a diagnosis of CM.7
Risk factors for CM
| Non-modifiable | Old age |
| Female | |
| White | |
| Genetic factors | |
| Low socioeconomic status | |
| Low educational level | |
| Modifiable | Anxiety, depression, stress |
| SAHS, snoring | |
| Caffeine or medication overuse | |
| Obesity | |
| High migraine frequency | |
| Putative | Proinflammatory and prothrombotic factors |
Revised criteria for medication overuse headache (ICHD-II 2006)
| A. Headache present on at least 15 days per month |
| B. Regular overuse for at least 3 months of one or more drugs taken for acute and/or symptomatic treatment:Regular use of ergots, triptans, opioids, or a combination of analgesics on at least 10 days per month for more than 3 monthsRegular use of simple analgesics or any combination of ergots, triptans, or opiates, on at least 15 days per month for more than 3 months, without overuse of any single class alone |
| C. Headache has developed or markedly worsened during medication overuse |
Based on the above, our main purpose is to compare clinical and demographical characteristics in a large hospital series of CM patients, with and without MO, in addition to comparing the same characteristics between CM and EM patients.
Patients and methodsIn January 2008, a specialist headache clinic was created at our tertiary hospital. Since then, we have prospectively recorded all patients attending our unit.
Of the patient total attending the specialist headache unit between January 2008 and May 2012, we prospectively analysed all patients with a diagnosis of migraine (according to ICHD-III criteria)4 and CM with MO (ICHD-II revised criteria, 2006).6 For each eligible patient, we recorded age, sex, age at migraine onset, progression time (years), previous use of preventive or symptomatic medication, and impact of migraine on daily life activities as measured with the Headache Impact Test (HIT-6). We determined the monthly frequency of migraine episodes and the presence of MO by checking the patients’ diaries, which had been updated during the months previous to initial consultation.
We compared clinical and demographical characteristics between CM and EM groups, and subsequently between CM patients with and without MO. We used the t test or the chi-square test, depending on the data distribution, and set the level of statistical significance at P=0.05. SPSS version 15.0 was used for statistical analysis.
ResultsA total of 1868 patients attended our headache clinic during the inclusion period, and 1249 of them (66.8%) were diagnosed with migraine: 815 with EM (65.2%) and 434 with CM (34.8%).
Female/male ratio in the EM group was 2.82. Mean (SD) age at initial consultation was 37.1 (14.3) years (range, 11-80); mean reported age at migraine onset was 23.6 (11.9) years (range, 6-78); and mean progression time was 13.5 (12.8) years (range, 0-62). While 97.2% of patients had tried some type of symptomatic treatment before the initial consultation, only 33.1% had received preventive treatment. Mean (SD) HIT-6 score in the EM group was 57.7 (9) points (range, 36-78); 63% of these patients scored higher than 55 points.
In the CM group, female/male ratio was 4.6, mean age at initial consultation was 43.9 (14.6) years (range, 14-92), mean reported age at migraine onset was 22.2 (11.2) years (range, 6-71), and mean progression time was 21.6 (14.4) years (range, 1-78). All patients had previously received some type of symptomatic treatment and 56.9% had received preventive treatment. Estimated impact on daily life was 61.7 (6.8) points (range, 38-76) according to HIT-6; 84.4% of CM patients showed at least moderate disability (HIT-6>55).
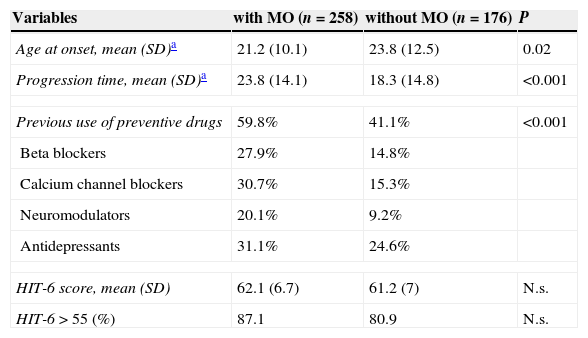
When comparing data between CM patients with MO (258 patients: 211 women and 47 men) and CM patients without MO (176 patients: 146 women and 30 men), we found that reported age at migraine onset was significantly lower, and time elapsed between migraine onset and first visit to our clinic was longer, in patients with both CM and MO. Additionally, the percentage of patients who had previously taken a preventive treatment was substantially higher in the MO group. The most common preventive treatments prescribed to patients in both groups prior to being attended in our clinic were antidepressants (31.1% in patients with MO and 24.6% in patients without MO). A large percentage of patients in both CM groups (28.8% of patients with MO and 24.6% of patients without MO) had received only one type of preventive treatment before visiting our clinic. The breakdown of treatments linked to MO was as follows: analgesics, 61.6%; drug combinations, 30.9%; triptans, 3.7%; ergotamine, 2.8%; and opioids, 0.2%. The impact of migraine in daily life was similar in the 2 groups according to HIT-6. Comparative data from CM patients with and without MO are listed in Table 4.
Comparison between CM patients with and without symptomatic medication overuse
| Variables | with MO (n=258) | without MO (n=176) | P |
|---|---|---|---|
| Age at onset, mean (SD)a | 21.2 (10.1) | 23.8 (12.5) | 0.02 |
| Progression time, mean (SD)a | 23.8 (14.1) | 18.3 (14.8) | <0.001 |
| Previous use of preventive drugs | 59.8% | 41.1% | <0.001 |
| Beta blockers | 27.9% | 14.8% | |
| Calcium channel blockers | 30.7% | 15.3% | |
| Neuromodulators | 20.1% | 9.2% | |
| Antidepressants | 31.1% | 24.6% | |
| HIT-6 score, mean (SD) | 62.1 (6.7) | 61.2 (7) | N.s. |
| HIT-6>55 (%) | 87.1 | 80.9 | N.s. |
SD: standard deviation; HIT-6: Headache Impact Test-6; N.s.: non-significant; MO: medication overuse.
Estimated prevalence of CM in the general population ranges from 1.4% to 2.2%.10 In line with previous studies, we have observed that CM is a very common diagnosis not only among patients attending our headache clinic (23.2% in our series) but also in neurology departments in general (5-10% of all patients11). However, these percentages vary between studies; a previous study published by our research group, analysing 1000 headaches in 682 patients, found that 12.4% of the patient total met ICHD-II diagnostic criteria for CM.12 Another study by Irimia et al. including 370 patients found that 46.4% of them had migraine, and CM accounted for 5.4% of the total diagnoses.13
Epidemiological studies further our understanding of the magnitude and impact of migraine in our setting, but additional research may still be needed to explain the role of certain predictors of incidence and progression of migraine.14 Migraine is an important social and healthcare problem worldwide; in fact, according to the WHO Global Burden of Disease Study 2010, migraine is the main cause of disability among the neurological diseases.15
In our study we have assumed that CM and chronic headache associated with MO are not independent diseases, but rather that MO is one among many risk factors involved in CM development. This assumption may have inflated the percentage of CM patients. If we consider only CM patients without MO (in keeping with the revised criteria of 2006), the percentage of CM patients in our study drops to 9.4%. Nevertheless, revised ICHD-III criteria (2013)7 were published after this study had been completed. The ICHD-III currently lists the possibility of MO being associated with a diagnosis of CM, as we had assumed in our research.
In line with other published studies,11,16,17 our series showed a greater proportion of women in both the CM and EM groups, although the female/male ratio was higher in the CM group. We observed that CM patients tend to delay visiting our clinic more than EM patients, since their overall progression time after migraine onset is often longer. Virtually all patients had received symptomatic treatment prior to visiting our clinic, while only 33.1% of EM patients and 56.9% of CM patients had ever taken some type of preventive treatment.
Numerous studies have already shown the impact of migraine on patients’ professional, social, and family lives.18–20 HIT-6, the tool we use in daily practice, is a 6-item scale that evaluates functional health and well-being. It measures the impact of headache on daily life activities and cognitive function, as well as its associated degree of psychological impact. Although several authors support the idea that the impact and disability produced by CM are greater in patients with MO,21 our findings show that CM has a sizeable impact on both patients with and without MO, and that the impact of CM is clearly greater than that of EM. This difference, previously emphasised by other authors,22–24 shows the need for early diagnosis of CM, which will in turn allow us to apply more specific treatment measures at earlier stages.
As in other studies that have examined CM-related care burden,25 our data analysis reveals that CM patients with MO experience migraine onset at an earlier age than their counterparts without MO, and also visit our clinic with a longer history of the disease (progression time>20 years). Our study also shows that a larger percentage of CM patients with MO than those without MO had received some type of preventive treatment before visiting our clinic. Antidepressants were the most frequent preventive treatment in both groups. Increased use of preventive treatments in CM patients with MO, which accompanies the prolonged progression time in these patients, may not be the cause of EM chronification: rather, these patients will require symptomatic treatment more frequently as their migraines become chronic. This reflection may help us provide better care for our patients by proposing more effective and practical therapeutic alternatives than simply discontinuing analgesic drugs.
In conclusion, we can state that CM (both with and without MO) is a very common disease in a specialist headache unit at a tertiary hospital. The impact of migraine, which was measured using HIT-6, is significant in both CM groups and causes at least moderate disability in more than 80% of all MC patients. In addition, CM patients with MO experience migraine onset at a younger age and are seen in our clinic after a longer progression time; prior to that visit, they have already received preventive treatment, mainly antidepressants.
FundingThis study has received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Rojo E, Pedraza MI, Muñoz I, Mulero P, Ruiz M, de la Cruz C, et al. Diferencias entre migraña crónica con y sin uso excesivo de medicación: experiencia en una serie hospitalaria de 434 pacientes. Neurología. 2015;30:153–157.
Part of this study was presented as an oral communication at the 64th Annual Meeting of the Spanish Society of Neurology, Barcelona, November 2012.