Streptococcus agalactiae is frequently an asymptomatic coloniser and a cause of neonatal and puerperal sepsis. Infections in non-pregnant adults are uncommon. The frequency of neurological complications caused by invasive infection with this microorganism in adults remains unknown. Here, we study the frequency and characteristics of central nervous system (CNS) involvement in adults with invasive S. agalactiae infection.
Patients and methodsReview of all adults with invasive S. agalactiae infection between 2003 and 2011 in a tertiary hospital.
ResultsS. agalactiae was isolated from blood, cerebrospinal fluid or synovial fluid in 75 patients. Among them, seven (9.3%) displayed neurological involvement: five men and two non-pregnant women, aged between 20 and 62 years. Diagnoses were spinal epidural abscess due to spondylodiscitis with spinal cord compression; acute bacterial meningitis; ischaemic stroke as presentation of bacterial endocarditis (two patients each); and meningoventriculitis after neurosurgery and ventricular shunting. One patient with endocarditis caused by S. agalactiae and S. aureus died in the acute phase, and another died 3 months later from metastatic cancer. The other patients recovered without sequelae. All patients had systemic predisposing factors for infection and five (71.4%) had experienced disruption of the mucocutaneous barrier as a possible origin of the infection.
ConclusionsCNS involvement is not uncommon in adult patients with invasive infection caused by S. agalactiae. Isolating S. agalactiae, especially in cases of meningitis, should lead doctors to search for predisposing systemic disease and causes of mucocutaneous barrier disruption.
El Streptococcus agalactiae (S. agalactiae) es un germen frecuentemente colonizador asintomático y causante de sepsis neonatal y puerperal. Las infecciones en adultos, fuera del embarazo, son poco frecuentes. No se conoce la frecuencia de complicaciones neurológicas en adultos con infección invasiva por este microorganismo. Hemos estudiado la frecuencia y las características de la afectación del sistema nervioso central (SNC) en pacientes adultos con infección invasiva por S. agalactiae.
Pacientes y métodosSe revisó a todos los pacientes adultos con infección invasiva por S. agalactiae en un hospital terciario entre 2003 y 2011.
ResultadosEn 75 pacientes se aisló S. agalactiae en sangre, líquido cefalorraquídeo o líquido articular. De ellos, 7 (9,3%) tuvieron afectación neurológica: 5 hombres y 2 mujeres no embarazadas, con edades entre 20 y 62 años. Los diagnósticos fueron: absceso epidural secundario a espondilodiscitis con compresión medular, meningitis bacteriana aguda, ictus isquémico como presentación de endocarditis bacteriana (2 pacientes cada uno) y meningoventriculitis tras neurocirugía y derivación ventricular. Un paciente con endocarditis por S. agalactiae y S. aureus falleció en la fase aguda y otra a los 3 meses por neoplasia metastásica. El resto se recuperó sin secuelas. En todos los casos, hubo factores predisponentes sistémicos para la infección y 5 (71,4%) tenían rotura de barrera mucocutánea como posible origen de la infección.
ConclusionesLa afectación del SNC es relativamente frecuente en pacientes adultos con infección invasiva por S. agalactiae. El aislamiento de S. agalactiae debe hacer investigar causas predisponentes sistémicas y causas de rotura de barrera mucocutánea, sobre todo en meningitis.
Streptococcus agalactiae, or group B beta-haemolytic streptococcus, colonises the gastrointestinal tract, urinary tracts, the female genital tract, and the skin. It frequently causes puerperal infections and sepsis, as well as neonatal meningitis.1 In non-pregnant adults, invasive infections caused by S. agalactiae are not infrequent, with an incidence of 4.4 cases per 100000 inhabitants.2 However, S. agalactiae infections of the central nervous system (CNS) are very rare in adults.1–12 The frequency of neurological complications caused by invasive infection by this microorganism remains unknown. This study analyses the cases of invasive S. agalactiae infection in adults seen in a tertiary hospital within a 7-year period in order to study the frequency and characteristics of CNS involvement in these patients.
Patients and methodsWe retrospectively analysed the clinical histories of all patients older than 18 years diagnosed with systemic or invasive infection caused by S. agalactiae and treated in our hospital from January 2003 to May 2011. To this end, we reviewed the database of the microbiology department and identified all S. agalactiae isolates detected during the study period. Isolates were selected from normally sterile sites such as blood cultures, cerebrospinal fluid (CSF), and synovial fluid (invasive infection), excluding any isolates from urine or skin. We selected all cases of neurological involvement in patients with invasive infections caused by S. agalactiae. We collected clinical and epidemiological data, results from complementary tests, treatments used, and outcomes of cases of neurological involvement.
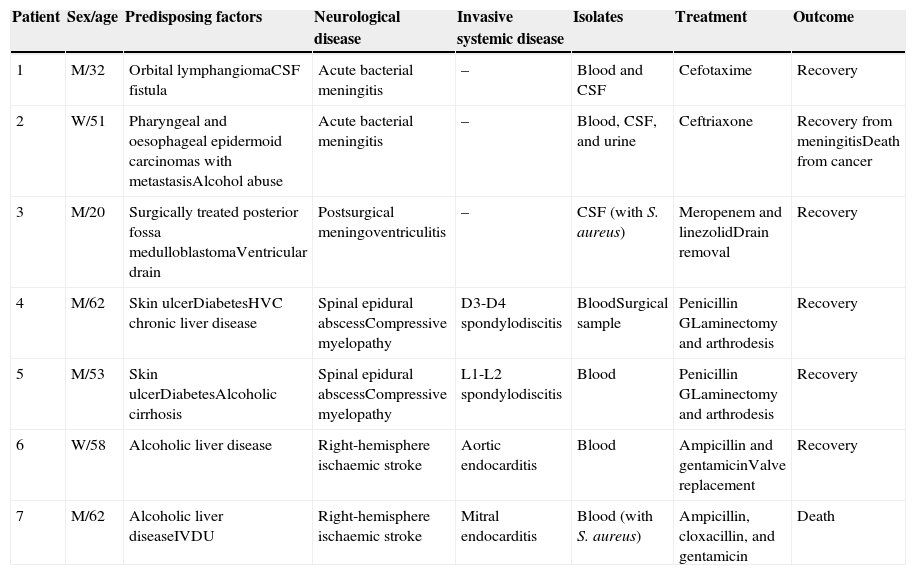
ResultsS. agalactiae was isolated in 75 patients, including 72 isolates from blood cultures, 3 from CSF, and 2 from synovial fluid. Of these patients, seven (9.3%) displayed neurological involvement: five men and two non-pregnant women with a mean age of 48 years (range 20–62). The patients’ clinical characteristics are listed in Table 1.
Clinical characteristics and outcomes of patients with neurological involvement associated with invasive S. agalactiae infection
| Patient | Sex/age | Predisposing factors | Neurological disease | Invasive systemic disease | Isolates | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | M/32 | Orbital lymphangiomaCSF fistula | Acute bacterial meningitis | – | Blood and CSF | Cefotaxime | Recovery |
| 2 | W/51 | Pharyngeal and oesophageal epidermoid carcinomas with metastasisAlcohol abuse | Acute bacterial meningitis | – | Blood, CSF, and urine | Ceftriaxone | Recovery from meningitisDeath from cancer |
| 3 | M/20 | Surgically treated posterior fossa medulloblastomaVentricular drain | Postsurgical meningoventriculitis | – | CSF (with S. aureus) | Meropenem and linezolidDrain removal | Recovery |
| 4 | M/62 | Skin ulcerDiabetesHVC chronic liver disease | Spinal epidural abscessCompressive myelopathy | D3-D4 spondylodiscitis | BloodSurgical sample | Penicillin GLaminectomy and arthrodesis | Recovery |
| 5 | M/53 | Skin ulcerDiabetesAlcoholic cirrhosis | Spinal epidural abscessCompressive myelopathy | L1-L2 spondylodiscitis | Blood | Penicillin GLaminectomy and arthrodesis | Recovery |
| 6 | W/58 | Alcoholic liver disease | Right-hemisphere ischaemic stroke | Aortic endocarditis | Blood | Ampicillin and gentamicinValve replacement | Recovery |
| 7 | M/62 | Alcoholic liver diseaseIVDU | Right-hemisphere ischaemic stroke | Mitral endocarditis | Blood (with S. aureus) | Ampicillin, cloxacillin, and gentamicin | Death |
Two patients (patients 1 and 2) presented symptoms of acute bacterial meningitis with fever, headache, and neck rigidity lasting 7 days in the first patient and 2 days in the second. Patient 2 displayed an altered level of consciousness. In both patients, CSF showed polymorphonuclear pleocytosis (4640 and 3800cells/mm3) with elevated protein levels (2 and 1.5mg/dL) and low glucose levels (40 and 35mg/dL). After recovering from meningitis, they were diagnosed with CSF fistula (patient 1) and pharyngeal and oesophageal epidermoid carcinomas with lymph node metastases (patient 2).
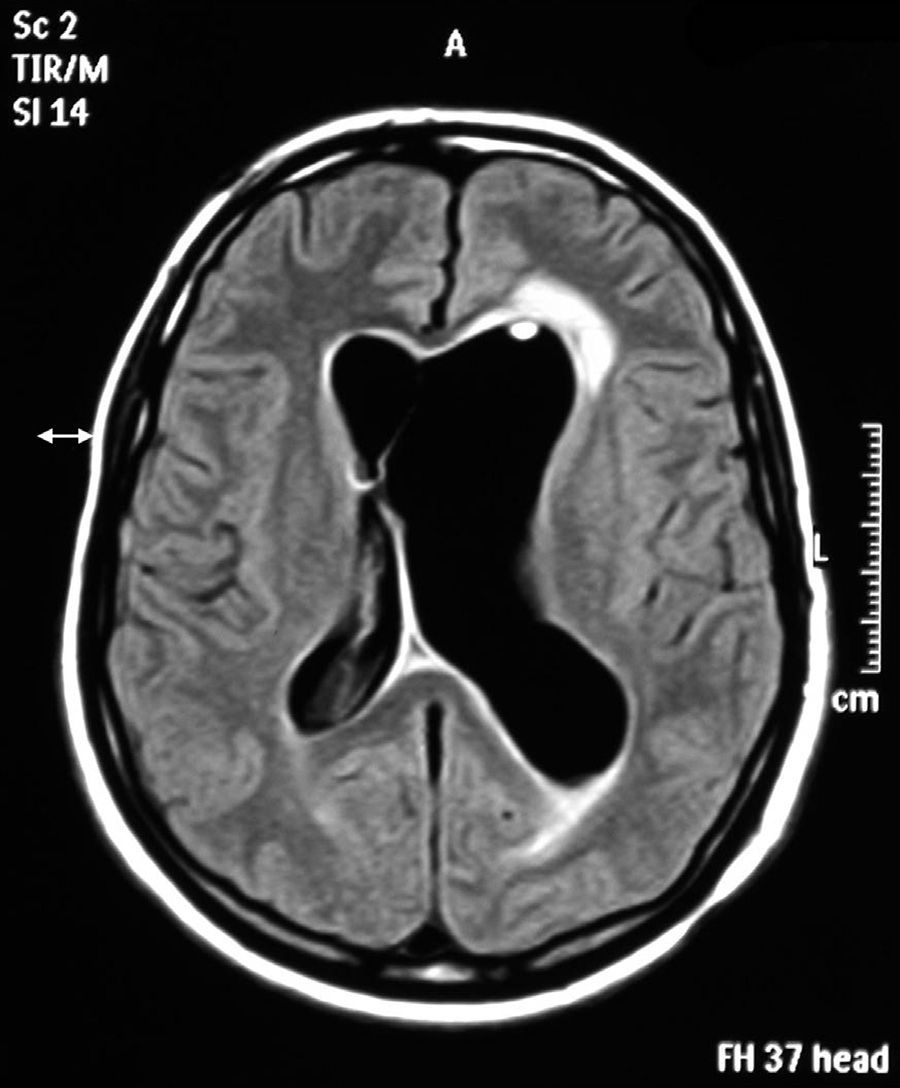
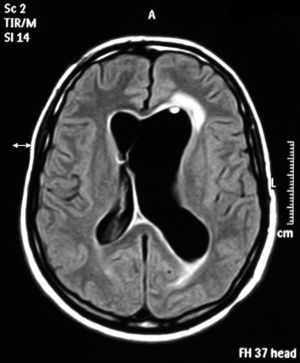
Patient 3 displayed symptoms of meningitis and ventriculitis, characterised by fever and decreased level of consciousness. These features appeared less than 24hours after an external ventricular drain was placed to treat hydrocephalus secondary to resection of posterior fossa medulloblastoma. The CSF study revealed 2000leukocytes/mm3 (predominantly polymorphonuclear cells), a protein level of 0.75g/dL, and a glucose level of 75mg/dL. Cranial magnetic resonance imaging (MRI) revealed significant meningeal and ventricular contrast uptake (Fig. 1).
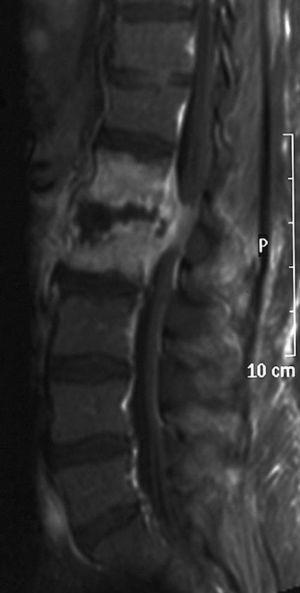
Two patients (patients 4 and 5) came to the emergency department due to subacute symptoms (2- and 1-week histories, respectively) of progressive myelopathy with paraparesis, hypoaesthesia showing a sensory level, and pyramidal syndrome. Patient 5 also displayed urinary retention. Both patients had symptoms of fever and back pain that had presented 30 and 10 days before, respectively. Neither patient had been examined for these symptoms. Spinal MRI revealed spondylodiscitis with epidural abscess causing compression of the spine in both patients (Fig. 2).
Two patients (patients 6 and 7) were admitted due to hemispheric acute ischaemic stroke. Patient 6 had been experiencing fever for 5 days, as well as moderate dyspnoea. Patient 7 had fever at the time of admission. He also experienced confusional symptoms in addition to his focal symptoms. Heart murmur was auscultated in both cases, and echocardiography confirmed presence of wart-like lesions on the heart valves due to bacterial endocarditis.
Regarding predisposing factors of systemic infection, four patients (57.1%) presented chronic alcohol abuse; three of the same patients had chronic liver disease (cirrhosis in one case), and one had C virus-related chronic liver disease. In addition, three patients (42.9%) had tumours and two (28.6%) had diabetes. Furthermore, five (71.4%) of the seven patients presented breaks in the skin barrier that may have favoured invasive infection by skin bacteria: skin ulcers (two patients), CSF fistula, intravenous drug use, and neurosurgery. Co-infection with another skin pathogen, Staphylococcus aureus, was reported in two of these patients (patients 3 and 7).
All S. agalactiae isolates were sensitive to penicillin, ampicillin, and cephalosporins. All patients were treated with penicillin G or third generation cephalosporins, with the exception of the patient with postsurgical meningitis and ventriculitis associated with S. aureus. This patient was treated with meropenem and linezolid. The two patients with spondylodiscitis were treated with surgical decompression and subsequent stabilisation. The extraventricular drain was removed from the patient with associated meningoventriculitis.
Two patients (28.6%) died, one due to multiple organ dysfunction (patient 7) and the other due to underlying neoplasia, 3 months after recovering from meningitis (patient 2). Outcomes for the remaining cases were favourable regarding resolution of the infection. The two patients with myelopathy recovered their strength completely thanks to early surgical decompression. The patient with stroke who survived also recovered from her motor deficit.
DiscussionAlmost half of all invasive infections due to S. agalactiae present in adults.2 Several studies suggest that incidence of these infections in adults has increased over the past decades, and this trend is probably associated with ageing and diseases favouring infection.1,2,7 Invasive infection due to this microorganism is most frequently found in the skin, soft tissues, bones, joints, urinary tract, lungs, and peritoneum, as well as the genital tract during pregnancy and puerperium. Endocarditis is very infrequent (0%–3%). Between 19.4% and 48% of patients presented bacteraemia without a focus.1–8 In adults, CNS infections due to S. agalactiae, almost always meningitis, are very rare.9–12 These infections represent between 0.3% and 4.3% of all cases of bacterial meningitis.9,10 In contrast with what one might expect, meningitis due to S. agalactiae associated with pregnancy is not frequent,9,13 and we found no cases in our series. In our study, the frequency of meningitis in all adult patients with invasive infections due to S. agalactiae was 4%. A frequency of approximately 1% (range 0%–4%) has been reported in other studies,1–5 although another study reported a frequency of 9.8%.6 We should highlight our study's high rate of neurological involvement, detected in 9.3% of patients with invasive S. agalactiae infection due to this pathogen. Although four of our patients displayed neurological symptoms that were secondary to infection in a different location (endocarditis and spondylodiscitis), they all came to the emergency department due to their neurological signs. Fever and other previous or simultaneous symptoms help identify the infection underlying the neurological condition. Although endocarditis and spondylodiscitis14 due to S. agalactiae are rare diseases, all the patients in our study presented with neurological complications.
A large percentage of adults with invasive S. agalactiae infections present conditions other than pregnancy that can favour this type of infection (64.6%–98.8%, depending on the series). These conditions include diabetes, kidney failure, cancer, liver disease, and cardiovascular disease.1,3,5,6,8 In our study, all patients with neurological involvement presented at least one systemic factor favouring infection (liver disease, tumour, diabetes). But more striking is the fact that 71.4% of the patients presented breaks in the skin or mucosa that may have allowed the infection to enter, since S. agalactiae may colonise the skin and pharynx. This portal of entry hypothesis is supported by the fact that infection was associated with S. aureus in two cases. This portal of entry is clear in cases of meningitis associated with CSF fistula and postsurgical meningoventriculitis associated with shunting. We cannot rule out pharyngeal and oesophageal carcinomas as the cause of the broken barrier in the other case of meningitis. In a review of 64 cases of meningitis due to S. agalactiae, 11% were associated with communication between the subarachnoid space and the skin or mucosal surfaces, while 3% were post-neurosurgical.9 Our results indicate the need to search for causes of broken skin or mucosa in all patients with invasive infection due to this pathogen, and especially in cases of meningitis.
Mean age in our patients (48 years) is lower than that reported by other studies in adults excluding pregnant women (58–63 years).1,2,4 Although incidence of invasive S. agalactiae infection increases with age,1,2 it affected young and middle-aged patients in our group with neurological involvement, and all of them presented predisposing factors. This tendency indicates that any age-related increase in risk of the infection probably results from age-related increase in its predisposing factors.
S. agalactiae is almost always sensitive to penicillin, ampicillin, and cephalosporins,1,6 as in our cases. For this reason, mortality associated with this infection has been low in our study. Only one patient died during the acute phase (14.3%), but this case also featured co-infection with S. aureus, a pathogen associated with high mortality endocarditis. Overall mortality (28.6%) is within the range reported by other studies (6.25%–33%), in which comorbidity and age have an important impact on mortality.1,3–7 As can be expected, higher rates of mortality are associated with meningitis. In one series, 66.7% of the patients with meningitis died, although overall mortality in the literature was 34.4%.9
In conclusion, CNS involvement is relatively frequent among patients with invasive infection due to S. agalactiae. Although cases of meningitis are relatively rare, cases of serious infections due to this microorganism can present such neurological complications as endocarditis or spondylodiscitis. S. agalactiae isolation should lead to an investigation of systemic predisposing factors and causes of mucocutaneous barrier disruption, especially in cases of meningitis.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Oyanguren B, Esteban L, Guillán M, de Felipe A, Alonso Cánovas A, Navas E, et al. Afectación del sistema nervioso central en la infección invasiva por Streptococcus agalactiae en adultos. Neurología. 2015;30:158–162.
Presented at the 63rd Annual Meeting of the Spanish Society of Neurology. Barcelona, 2011.