Fabry disease is an X-linked disorder of lysosomal metabolism that causes glycosphingolipid deposits in different tissues, with vascular endothelium being particularly susceptible. Clinical manifestations vary depending on the patient's age at onset; they include skin lesions, acroparesthesia, pain episodes, anhidrosis, corneal opacity, hearing loss, and others. However, its vascular complications in the kidneys, heart, and brain are severe, especially in late-onset cases or in patients with longer histories of the disease. Although other types of neurological manifestations may be present, cerebrovascular problems are particularly frequent and serious.1,2 Doctors consider Fabry disease in the differential diagnosis of strokes of undetermined causes, and these strokes are most commonly linked to the vertebrobasilar territory.
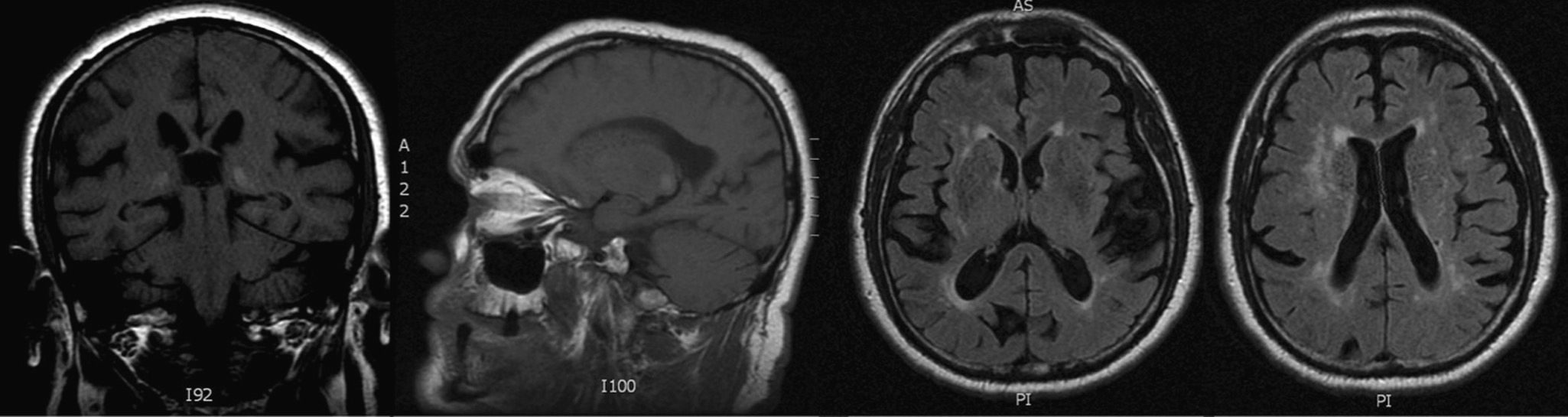
Early diagnosis of this disease is important, given the availability and usage recommendations for enzyme replacement therapy with recombinant acid alpha-glucosidase.3 For example, researchers have described that hyperintensities in both pulvinar nuclei in a T1-weighted MRI sequence may be a pathognomonic sign for Fabry disease.4
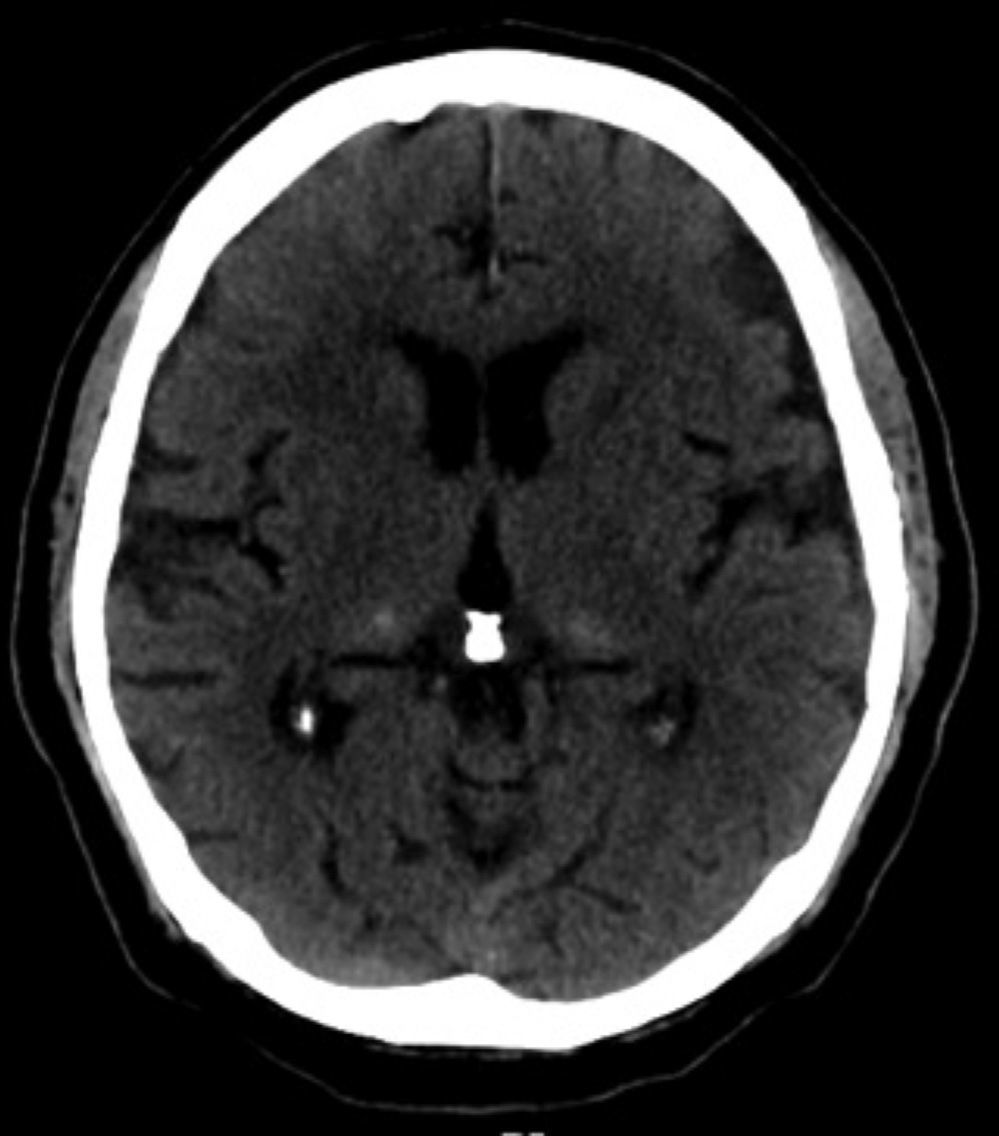
We present the case of a patient with ischaemic stroke and bilateral pulvinar hyperintensities whose enzyme analysis was negative for Fabry disease. This 64-year-old man with hypertension and dyslipidaemia experienced sudden-onset dizziness and instability together with loss of lower limb strength and impaired enunciation. Neurological examination observed right hemiparesis which abated over the next few hours. Cranial CT revealed hyperintensities in both pulvinar nuclei (Fig. 1). A T2-weighted MRI also showed a hyperintense lesion in the left hemi-pons with restricted diffusion; findings are compatible with a recent infarct. In the T1-weighted sagittal sequence, we also observed hyperintensity restricted to both pulvinar nuclei (Fig. 2). Hyperintense lesions in the subcortical and periventricular white matter are also apparent in the T2-weighted sequence. There were no clinical signs or symptoms that would indicate Fabry disease, and the patient had no family history of the entity. Spectrofluorimetric determination of acid alpha-glucosidase in blood showed an activity level of 100%. We also ruled out other causes of calcification in the basal ganglia by measuring calcium, parathyroid hormone, glucose, and ammonia; HIV serology was also tested. It is therefore possible to state that pulvinar hyperintensity in this case may be secondary to small-vessel impairment due to arterial hypertension. Furthermore, pulvinar hyperintensity was secondary to calcifications at this location according to CT and MRI; similar findings have also been demonstrated in studies of Fabry disease.
To the best of our knowledge, this is the first reported case in which T1-weighted images of pulvinar hyperintensity are not linked to Fabry disease. Two other case studies have questioned whether the sign is really pathognomonic; in both, however, hyperintensity was not limited to the pulvinar nucleus and also affected the lenticular nucleus.5 The frequency of this radiological sign in patient series with Fabry disease4–6 has been estimated at 25% in men, but exceptionally rare in women. For this reason, theories suggest that this pattern could be related to the lower enzymatic activity in men, which would result in the formation of vascular microcalcifications. Presence of the sign has been correlated to age and severity of kidney disease, but not to the appearance of ischaemic stroke.5
The case we present confirms that T1-weighted images of bilateral pulvinar hyperintensity secondary to calcification are not pathognomonic for Fabry disease. Researchers require further studies to evaluate the frequency of this sign, and its association with Fabry disease, in populations not previously diagnosed with Fabry disease. This will help us ascertain the diagnostic utility of this radiological sign in establishing ischaemic stroke aetiology.
Please cite this article as: Matías-Guiu JA, Yus M, Jorquera M, Porta-Etessam J. Hiperintensidad pulvinar en T1: ¿un signo patognomónico de enfermedad de Fabry? Neurología. 2014;29:442–443.