Wernicke encephalopathy is an acute neurological disorder secondary to thiamine deficiency. Its characteristic clinical triad, present in 16% to 38% of all patients, comprises confusion, eye disorders, and ataxia.1
Cytotoxic and vasogenic oedema are the most typical neuroimaging findings, and they appear as symmetrical hypointensities in T2-weighted sequences.2
The most frequently affected areas are the medial thalami and the periventricular region of the third ventricle (0%–85%), the periaqueductal area (59%–65%), the mammillary bodies (38%–65%), and the tectal plate (superior and inferior colliculus) (36%–38%).3 These regions are thought to be more sensitive to thiamine deficiency due to their high rates of oxidative and glucose metabolism associated with thiamine.
Atypical MR images have been described showing altered signal intensity in the cerebellum including the vermis, the nuclei of the cranial nerves, red nucleus, dentate nucleus, caudate nucleus, splenium, and cerebral cortex. These atypical alterations seem more frequent in non-alcoholic patients,4 and they are associated with typical lesions in most of the cases described in the literature.
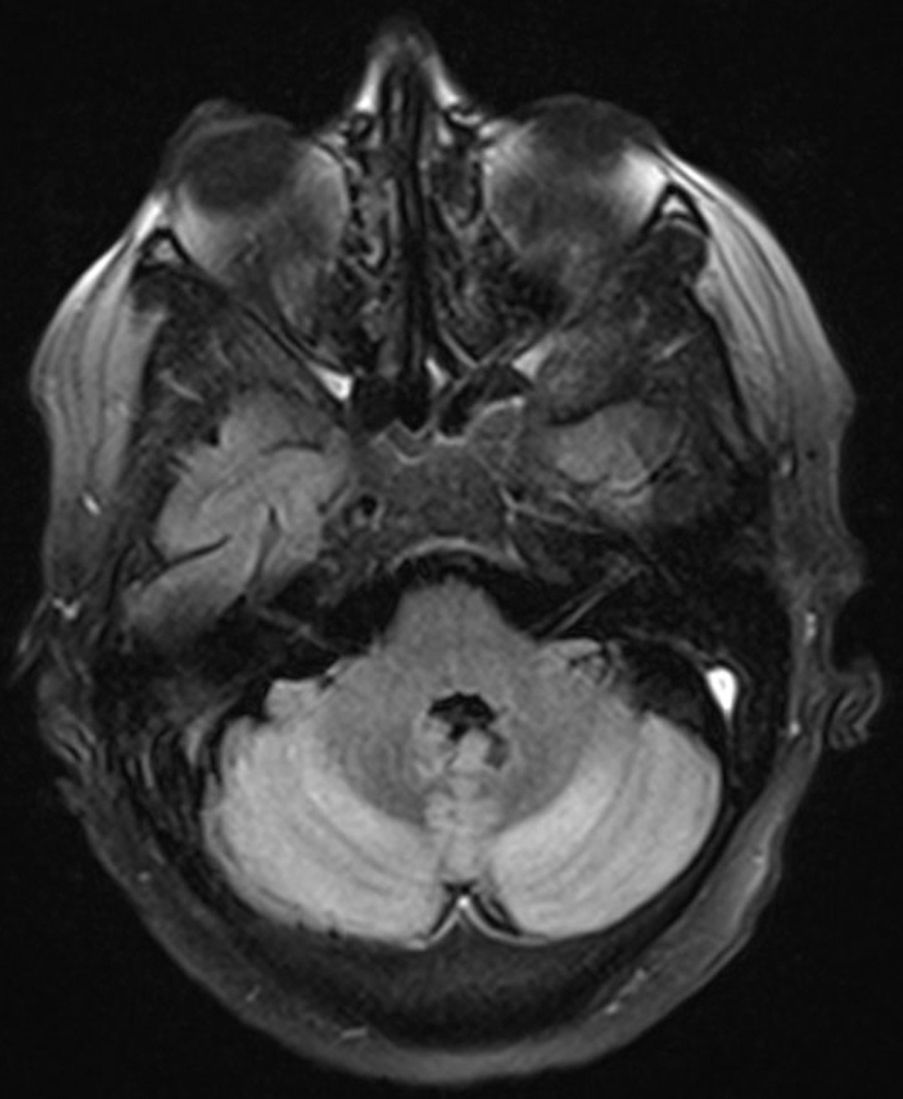
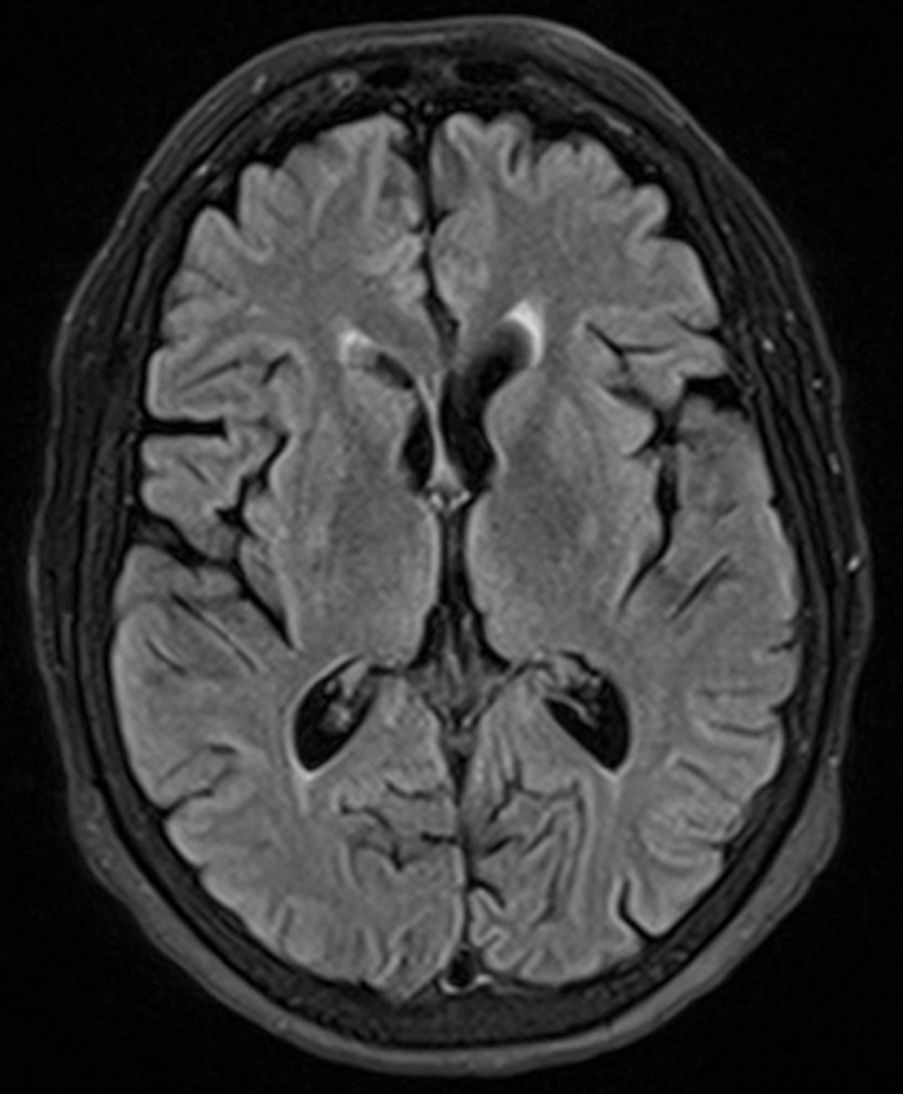
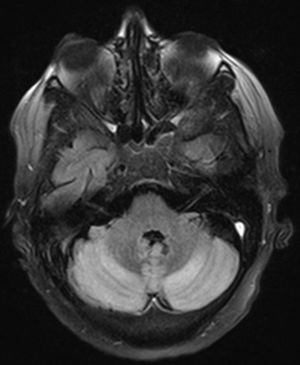
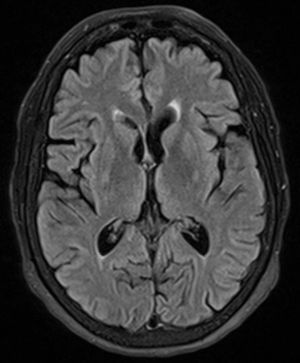
We present the case of a 51-year old woman with a history of type 2 diabetes mellitus, arterial hypertension, and a significant alcohol habit with secondary liver disease. She had been admitted to the haematology department the previous year due to folic acid deficiency. A relative brought her to our emergency department after finding her at home with signs of confusion and reporting double vision and difficulty speaking. She also presented difficulty walking and significant balance problems. Examination upon admission revealed evident dysarthria, horizontal diplopia and persistent left- and right-beating horizontal nystagmus, frank dysmetria of all 4 limbs, and ataxia rendering her unable with to walk independently. We performed a brain CT which showed no obvious acute lesions with the exception of mild cortical and subcortical atrophy, predominantly on the frontal and temporal lobes. A brain MRI alerted us to the presence of a diffuse hyperintensity in the cortex of both cerebellar hemispheres and vermis, with restricted diffusion in the T2-weighted sequence (Fig. 1). We observed no white matter lesions or alterations in the supratentorial brain parenchyma (Fig. 2). In light of these findings, we performed a SAT and brain MRI angiography which showed no alterations. We also performed a lumbar puncture and CSF showed normal biochemical results.
We initiated treatment with thiamine at high doses during hospitalisation (500mg IV every 8hours for 2 days, 500mg IV every 24hours for 5 days) according to the recommendations of the latest guidelines on treatment of Wernicke encephalopathy. The dose was subsequently changed to 300mg/24hours orally and maintained after discharge. From treatment onset, clinical symptoms improved progressively. Our patient was transferred to a medium- to long-stay centre to convalescence and undergo rehabilitating therapy. One month later, in a follow-up visit in our clinic, we observed that she had improved significantly: her speech was normal, she showed no diplopia or oculomotor alterations, and she was able to walk independently.
We present a case of Wernicke syndrome with an atypical radiological presentation, although cases with cerebellar involvement have already been described in the literature.5 Some believe cerebellar involvement may be present in more than half of the cases in autopsy studies.6 In almost all of published cases, cerebellar lesions are associated with altered signals in typical locations.1,7,8
This case highlights the absence of the MRI alterations pathognomonic for this entity, and the importance of early diagnosis and treatment of a patient at risk for thiamine deficiency and a suspicious clinical profile, regardless of the locations of altered MRI signals.
Conflicts of interestThe authors have no conflicts of interest to declare, and have not received any funding for this study.
Please cite this article as: Ruiz Bajo B, Moreno García MP, Rueda Mena E, González Chinchón G. Presentación atípica delsíndrome de Wernicke conafectación cerebelosa enresonancia magnética sinafectación en localizacionestípicas. Neurología. 2016;31:495–496.